Patients, tumors, and clinics
Detailed demographic and clinical data are summarized in Tables 1 and 2.
Table 1 Demographic data of 90 operated intracranial meningiomas in 48 NF2 patients.Table 2 Preoperative and postoperative symptoms in 80 surgeries due to intracranial NF2-associated meningiomas.
One patient exhibited a unilateral VS. Ten patients received external off-label treatment with bevacizumab prior to surgery and due to VS. To minimize adverse events such as bleeding and wound healing disorders, systemic treatment was halted four weeks before and after surgery. None of the three patients without additional intracranial meningiomas (apart from the operated lesion) showed any other non-vestibular schwannomas besides the bilateral VS.
Of the 31 patients who underwent genetic testing, 12 patients (39%) had NF2 truncating mutations (8 frameshift and four nonsense mutations), while 11 patients (35%) were mosaics. In the remaining eight patients, two splicing (6%), five deletions (16%), and one large genome alteration (3%) were identified in their blood DNA.
In five patients (10%), cerebrospinal fluid drainage (4 ventriculoperitoneal shunts and one endoscopic third ventriculostomy) was performed in the postoperative course due to newly developed signs of intracranial pressure.
Of the 32 (36%) meningiomas affecting the venous sinuses, 19 (59%) involved the superior sagittal sinus, 10 (31%) the cavernous sinus, two (6%) the transverse sinus, and one (3%) both the superior sagittal and confluent sinuses. A total of 67 (74%) meningiomas were completely resected (Simpson Grade I-III), while 23 (26%) were resected incompletely.
Seventy-five percent of cases with signs of increased ICP involved convexity and skull base meningiomas (each n = 6, 38%), while 19% (n = 3) and 1% (n = 1) involved falcine and tentorial meningiomas, respectively. Out of the 16 cases with signs or symptoms of increased ICP, 50% (n = 8) demonstrated a stenosis of the adjacent venous sinus. Most of these cases exhibited infiltration of the anterior or middle segment of the superior sagittal sinus, while only one tumor infiltrated each cavernous and transverse sinus.
Skull base tumors were highly (83%, n = 29) associated with focal neurological deficits, primarily due to intracranial nerve involvement, followed by falcine (6%, n = 2), intraorbital (8%, n = 3), and convexity (3%, n = 1) meningiomas, with no deficits reported in tentorial and intraventricular meningiomas. Only one patient with an operated falcine meningioma experienced seizures before surgery. In patients who experienced new postoperative seizures, two tumors were located at the falx, while the remaining tumor was found at the skull base.
Six patients exhibited postoperative complications, including cerebrospinal fluid leaks (which were manageable with a lumbar drain in all cases involving extensive intraoperative dura reconstruction), and two patients exhibited wound healing disorders, one of whom required surgical revision (this patient was under external off-label treatment with bevacizumab).
Additionally, one patient died during the postoperative outpatient period due to brain herniation after the second postoperative day and exhausted conservative and surgical (decompressive craniectomy) treatment. The exact cause of death was unclear, but there was a retrospective suspicion of silent status epilepticus or thromboembolic event. Notably, there were no postoperative bleeding events, particularly among those who externally received bevacizumab.
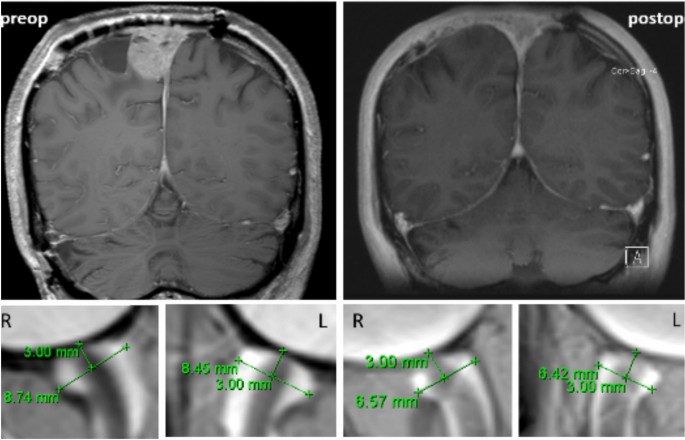
Pre- and postoperative ONSD course and association with influencing factors
Data are presented as mean ± standard deviation. In the comparison analysis of the 80 performed surgeries, 2 cases had incomplete ONSD values and were excluded for further analysis. Three outliers were identified through an inspection of a boxplot. The analysis was conducted both with and without these outliers, and since the results showed no significant differences, the outliers were retained in the final dataset.ONSD values immediately after surgery were normally distributed (p > 0.05), whereas the other time points were not normally distributed, as assessed by Shapiro–Wilk’s test (p < 0.05), respectively.
Mauchly’s test of sphericity indicated that the assumption of sphericity had been violated, x2 (5) = 34.23, p < 0.001.
There was an increase of ONDS values from the initial MRI (mean 6 ± 1.08, 4.45–8.49 mm) to immediately before surgery (mean 6.11 ± 0.89, 4.45–8.49 mm) with a further decrease immediately after surgery (mean 5.88 ± 0.91, 4.45–7.89 mm) up to the last MRI (mean 5.76 ± 0.86, 4.55–8.03 mm).
Epsilon (ε) was 0.810, calculated by Greenhouse and Geisser (1959), and was applied to correct the one-way repeated measures ANOVA. ONSD was statistically significantly different at the different time points during the course, F (2.429, 187.069) = 7.296, p < 0.001. Post hoc analysis with a Bonferroni adjustment revealed that ONSD values at the first MRI were statistically significant to the last MRI (95%CI, 0.005 to 0.364, p = 0.04). Furthermore, ONSD values immediately before surgery were statistically significant to immediately after surgery (95%CI, 0.021 to 0.094, p = 0.01) and to the last MRI (95%CI, 0.094 to 0.467, p < 0.001). All other comparisons were not statistically significant (p > 0.05).
In the multiple regression model, Simpson grading, Cranial Region, and segment of obstructed venous sinus did not significantly predict ONSD over the four-time points, p > 0.05.
For the following analysis of influencing factors, only the 72 cases involving the resection of a meningioma in a single operation were included.
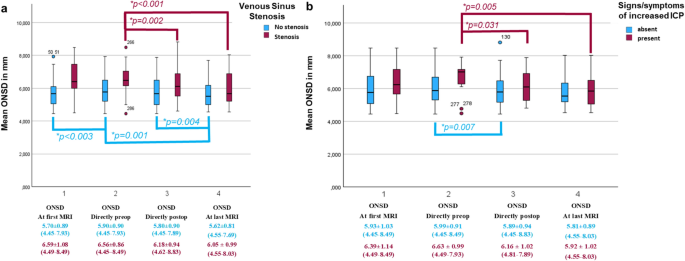
A two-way repeated measures ANOVA was run to determine the effect of venous sinus stenosis and ICP symptoms overtime on the ONSD course (ONSD at first MRI, ONSD directly preoperative, ONSD directly postoperative, ONSD at last postoperative MRI). Both comparisons for all tumors are illustrated in Fig. 2.
Boxplot Model of the ONSD course in the paired comparison meningioma groups: a) with/without venous sinus stenosis by compression or invasion, and b) preoperative signs/symptoms of increased ICP.
Venous sinus stenosis
The analysis of the studentized residuals confirmed normality (Shapiro–Wilk test) and the absence of outliers, as assessed by studentized residuals greater than ± 2 standard deviations. Mauchly’s test indicated sphericity (p > 0.05). A significant interaction was found between meningiomas with and without venous sinus stenosis and ONSD course, F (3,84) = 6.169, p < 0.001.
In meningiomas with venous sinus invasion or compression, significant changes in ONSD values were noted directly before and after surgery, with F (1,31) = 11.579, p = 0.002, showing a mean difference of 0.381 (95% CI, 0.153 to 0.609) mm. A notable difference was also found between preoperative and last postoperative MRI values, F (1,31) = 17.061, p < 0.001, mean difference of 0.510 (95% CI, 0.258 to 0.762) mm.
In contrast, meningiomas without venous sinus stenosis showed significant differences in ONSD values between the first MRI and preoperative values (F (1,55) = 9.821, p < 0.003, mean difference = 0.193, 95% CI, −0.316 to −0.070), and between postoperative and last follow-up ONSD values (F(1,54) = 9.146, p = 0.004, mean difference = 0.177, 95%CI, 0.060 to 0.294). A significant difference was also observed between preoperative and last MRI ONSD values (F (1,55) = 12.051, p = 0.001, mean difference = 0.279, 95%CI, 0.118 to 0.440). All other comparisons were not statistically significant (p > 0.05).
Signs and symptoms of elevated ICP
ONSD values were normally distributed (p > 0.05) except for patients or tumors without ICP signs at the last MRI (p = 0.022), based on the Shapiro–Wilk test assessing studentized residuals. No outliers were identified, as studentized residuals greater than ± 2 standard deviations indicated. Sphericity was met for the interaction term, as evaluated by Mauchly’s test of sphericity (p > 0.05). A statistically significant interaction between meningiomas with and without increased ICP and the ONSD course was found, F (3,42) = 3.191, p = 0.033.
In the meningioma group with increased ICP signs, ONSD values significantly differed directly before to after surgery, F (1,14) = 5.753, p = 0.031, mean difference = 0.469 (95% CI, 0.05 to 0.89) mm. ONSD values were also statistically significantly different directly before surgery than in the last postoperative MRI, F (1,14) = 11.118, p = 0.005, and the mean difference was 0.689 (95% CI, 0.246 to 1.132) mm.
On the other hand, in the meningioma group without signs of elevated ICP, ONSD values were statistically significantly different directly before surgery compared to the last postoperative MRI, F (1,62) = 7.656, p = 0.007, a mean difference of 0.178 (95% CI, 0.049 to 0.307) mm. All other comparisons were not statistically significant (p > 0.05).
ICP – intracranial pressure; ONSD – optic nerve sheath diameter, in mm.
ONSD Timepoint reflects the mean ONSD at (1) the initial MRI, (2) directly before and (3) after surgery, and (4) at the last follow-up MRI. *P-values of significant comparisons are illustrated. The other comparisons were not statistically significant. Particularly in the long-term course at the last follow-up, a significant decrease compared to the preoperative mean ONSD value was seen in both groups.
In the comparison groups, 32 (36%) of the 90 operated meningiomas exhibited a venous sinus stenosis, while 58 (64%) did not. Among the 80 surgeries performed, 16 (20%) cases presented preoperative intracranial pressure symptoms, with 64 (80%) cases showing no symptoms. Signs/symptoms of increased ICP included headaches, vomiting, nausea, visual impairment, double vision, and papilledema. These signs/symptoms were explicitly distinguished from other common complaints. Signs/symptoms of increased ICP were explicitly differentiated from other common complaints, such as wound pain, known migraine or tension headaches, and potential postoperative complaints like nausea, vomiting, and headaches following surgery in the posterior fossa, which may occur due to temporary loss of cerebrospinal fluid. In tumors causing venous sinus stenosis, the immediate preoperative ONSD values were almost identical to the preoperative ONSD values. This similarity likely occurred because the surgery was performed relatively early and prophylactically to prevent further compression.