Flynn, K. E. et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of US adults. J. Sex Med. 13(1642), 1650 (2016).
Tański, W., Dudek, K., Tomasiewicz, A. & Świątoniowska-Lonc, N. Sexual Dysfunction and quality of life in patients with rheumatoid arthritis. IJERPH 19, 3088 (2022).
Katz, H., Newton-John, T. R. O. & Shires, A. Sexual difficulties in the population with musculoskeletal chronic pain: A systematic review. Pain Med. 22, 1982–1992 (2021).
Kifle, Z. D. et al. Associations between endogenous sex hormones and multisite chronic musculoskeletal pain. Br. J. Anaesth. 134, 793–803 (2025).
Maurer, A. J., Lissounov, A., Knezevic, I., Candido, K. D. & Knezevic, N. N. Pain and Sex Hormones: A review of current understanding. Pain Manag. 6, 285–296 (2016).
Koechlin, H., Coakley, R., Schechter, N., Werner, C. & Kossowsky, J. The role of emotion regulation in chronic pain: A systematic literature review. J. Psychosom. Res. 107, 38–45 (2018).
Edlund, S. M., Carlsson, M. L., Linton, S. J., Fruzzetti, A. E. & Tillfors, M. I see you’re in pain – The effects of partner validation on emotions in people with chronic pain. Scand J. Pain 6, 16–21 (2015).
Antony, T., Alzaharani, S. Y. & El-Ghaiesh, S. H. Opioid-induced hypogonadism: Pathophysiology, clinical and therapeutics review. Clin. Exp. Pharma. Physio. 47, 741–750 (2020).
Rothmore, J. Antidepressant-induced sexual dysfunction. Med. J. Aust. 212, 329–334 (2020).
Flegge, L. G., Barr, A. & Craner, J. R. Sexual Functioning Among Adults with chronic pain: Prevalence and association with pain-related outcomes. Pain Med. 24, 197–206 (2023).
Finn, E., Morrison, T. G. & McGuire, B. E. Correlates of sexual functioning and relationship satisfaction among men and women experiencing chronic pain. Pain Med. 19, 942–954 (2018).
Bahouq, H., Allali, F., Rkain, H. & Hajjaj-Hassouni, N. Discussing sexual concerns with chronic low back pain patients: barriers and patients’ expectations. Clin. Rheumatol. 32, 1487–1492 (2013).
Odole, A. C. & Olugbenga-Alfred, A. A. Sexual Functioning and Selected Clinical and Psychosocial Factors Among Individuals with Chronic Non-specific Low Back Pain in Ibadan. Nigeria. Sex. Disability 36, 185–194 (2018).
Coates, R. & Ferroni, P. A. Sexual dysfunction and marital disharmony as a consequence of chronic lumbar spinal pain. Sex. Marital Therapy 6, 65–69 (1991).
Aaron, R. V. et al. Prevalence of depression and anxiety among adults with chronic pain: A systematic review and meta-analysis. JAMA Netw Open 8, e250268 (2025).
Evans-Durán, B., Tripp, D. A., Campbell, J., Doiron, R. C. & Nickel, J. C. Chronic prostatitis/chronic pelvic pain syndrome-related pain symptoms and their impact on sexual functioning. Can Urol. Assoc. J. 16, 222–227 (2022).
Tran, C. N. & Shoskes, D. A. Sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. World J. Urol. 31, 741–746 (2013).
Howard, H. S. Sexual adjustment counseling for women with chronic pelvic pain. J. Obstet Gynecol. Neonatal. Nurs. 41, 692–702 (2012).
Bergeron, S., Reed, B. D., Wesselmann, U. & Bohm-Starke, N. Vulvodynia. Nat Rev Dis Primers 6, 36 (2020).
Hill, D. A. & Taylor, C. A. Dyspareunia in Women. Am Fam Physician 103, 597–604 (2021).
Linton, S. J., Lardén, M. & Gillow, Å. -M. Sexual abuse and chronic musculoskeletal pain: Prevalence and psychological factors. Clin. J. Pain 12, 215–221 (1996).
Toomey, T. C., Seville, J. L., Mann, J. D., Abashian, S. W. & Grant, J. R. Relatinship of sexual and physical abuse to pain description, coping, psychlological distress, and health-care utilization in a chronic pain sample. Clin. J. Pain 11, 307–315 (1995).
Hart-Johnson, T. & Green, C. R. The impact of sexual or physical abuse history on pain-related outcomes among blacks and whites with chronic pain: Gender influence. Pain Med. 13, 229–242 (2012).
Tidmarsh, L. V., Harrison, R., Ravindran, D., Matthews, S. L. & Finlay, K. A. The Influence of adverse childhood experiences in pain management: mechanisms, processes, and trauma-informed care. Front. Pain Res. (Lausanne). 10(3), 923866. https://doi.org/10.3389/fpain.2022.923866 (2022).
Manninen, S.-M., Polo-Kantola, P., Vahlberg, T. & Kero, K. Patients with chronic diseases: Is sexual health brought up by general practitioners during appointments?. A web-based study. Maturitas 160, 16–22 (2022).
Porst, H. et al. The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: prevalence, comorbidities, and professional help-seeking. Eur Urol 51, 816–823; discussion 824 (2007).
Hägglund, D. & Wadensten, B. Fear of humiliation inhibits women’s care-seeking behaviour for long-term urinary incontinence. Scand J. Caring Sci. 21, 305–312 (2007).
Ghaderi, F., Bastani, P., Hajebrahimi, S., Jafarabadi, M. A. & Berghmans, B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: a randomized controlled clinical trial. Int. Urogynecol. J. 30(11), 1849–1855. https://doi.org/10.1007/s00192-019-04019-3 (2019).
Sharifipour, F. et al. Impact of Cognitive Behavior Therapy on Sexual Dysfunction of Women in Reproductive Age: A Systematic Review. Int. J. Sex. Health 36, 287–301 (2024).
Nusbaum, M. R., Hamilton, C. & Lenahan, P. Chronic illness and sexual functioning. Am. Fam. Physician. 67(2), 347–354 (2003) (PMID: 12562156).
Arends, S. A. M. et al. Feasibility and effectiveness of communication tools for addressing intimacy and sexuality in patients with cancer: a systematic review. Support Care Cancer. 32(2), 109. https://doi.org/10.1007/s00520-024-08308-6 (2024).
Managing Sexual Pain in Primary Care. Dorsey, Sarah M. et al. Advances in Family Practice Nursing, Volume 6, Issue 1, 97 – 116
Edwards, S. et al. ‘ReConnect’: a model for working with persistent pain patients on improving sexual relationships. Br. J. Pain. 14(2), 82–91. https://doi.org/10.1177/2049463719854972 (2020).
Manninen, S.-M., Kero, K., Perkonoja, K., Vahlberg, T. & Polo-Kantola, P. General practitioners’ self-reported competence in the management of sexual health issues – a web-based questionnaire study from Finland. Scand. J. Prim. Health Care 39, 279–287 (2021).
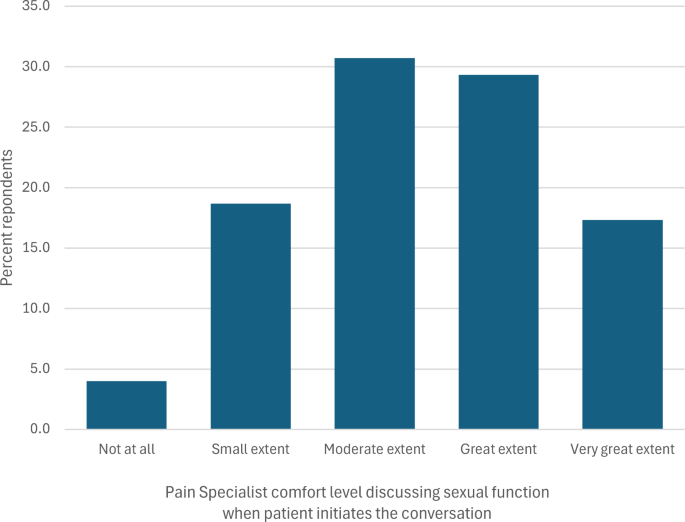
Goudman, L., van Schaik, D., Jager, T., Moens, M. & Scheerlinck, T. Discussing sexual health with patients eligible for spine surgery: An online survey in spine surgeon and pain physicians. Brain Spine 4, 102776 (2024).
Bilika, P. et al. Applying nociplastic pain criteria in chronic musculoskeletal conditions: A vignette study. J. Clin Med. 14(4), 1179. https://doi.org/10.3390/jcm14041179.PMID:40004711;PMCID:PMC11856051 (2025).
Heelas, L., Nicholas, J., Wiltshire, S. & Barker, K. Evaluation of patient reported outcomes following pain management programmes delivered via video conferencing during the Covid-19 pandemic. Physiotherapy 114, e8–e9. https://doi.org/10.1016/j.physio.2021.12.249 (2022).
Demori I, Molinari E, Rapallo F, et al. Online Questionnaire with Fibromyalgia Patients Reveals Correlations among Type of Pain, Psychological Alterations, and Effectiveness of Non-Pharmacological Therapies. Healthcare (Basel). 2022;10(10):1975. Published 2022 Oct 9. https://doi.org/10.3390/healthcare10101975
Hochberg, U., Sharon, H., Bahir, I. & Brill, S. Pain management – A decade’s perspective of a new subspecialty. J. Pain Res. 14, 923–930 (2021).
Linnemørken, L. T. B., Granan, L.-P. & Reme, S. E. Prevalence of posttraumatic stress symptoms and associated characteristics among patients with chronic pain conditions in a norwegian university hospital outpatient pain clinic. Front. Psychol 11, 749 (2020).
Meystre-Agustoni, G. et al. Talking about sexuality with the physician: are patients receiving what they wish?. Swiss Med. Wkly 141, w13178 (2011).
Zhang, L., Sherman, K. A. & Foster, M. Patient–provider communication and decision-making about sexual health in the context of chronic illness: A systematic review. Patient Educ. Couns. 103(7), 1342–1353 (2020).
Hendler, N. Why Chronic Pain Patients are Misdiagnosed 40 to 80% of the Time? 2, 94–98 (2016).
Bonica’s Management of Pain. (Wolters Kluwer Health, Philadelphia, 2019).
Wall and Melzack’s Textbook of Pain. (Elsevier/Saunders, Philadelphia, PA, 2013).
Hochberg, U., Ojeda, A., Brill, S. & Perez, J. An Internet-Based Survey to Assess Clinicians’ Knowledge and Attitudes Towards Opioid-Induced Hypogonadism. Pain Pract. 19, 176–182 (2019).
Rosen, R., Kountz, D., Post-Zwicker, T., Leiblum, S. & Wiegel, M. Sexual Communication Skills in Residency Training: The Robert Wood Johnson Model. J. Sex. Med. 3, 37–46 (2006).
Caldwell, L. et al. Surgeon Counseling Regarding Return to Sexual Activity After Pelvic Reconstructive Surgery. UROGC 29, 725–731 (2023).
Cano, A., Corley, A. M., Clark, S. M. & Martinez, S. C. A Couple-Based Psychological Treatment for Chronic Pain and Relationship Distress. Cogn. Behav. Pract. 25, 119–134 (2018).
Taylor, B. & Davis, S. The Extended PLISSIT model for addressing the sexual wellbeing of individuals with an acquired disability or chronic illness. Sex Disabil 25, 135–139. https://doi.org/10.1007/s11195-007-9044-x (2007).
Ozdemir, S., Gangal, A. D. & Erenel, A. S. The effect of sexual counseling based on PLISSIT and EX-PLISSIT models on sexual function, satisfaction, and quality of life: A systematic review and meta-analysis. Arch. Sex. Behav. 53(9), 3485–3513. https://doi.org/10.1007/s10508-024-02898-2 (2024).
Zohreh Khakbazan, Fatemeh Daneshfar , Zahra Behboodi-Moghadam, Seyed Massood Nabavi, Sogand Ghasemzadeh, Abbas Mehran. The effectiveness of the Permission, Limited Information, Specific suggestions, Intensive Therapy (PLISSIT) model based sexual counseling on the sexual function of women with Multiple Sclerosis who are sexually active. Mult Scler Relat Disord. 2016 Jul:8:113–9