Limitations and strengths
The present study had several limitations and strengths. One limitation was associated with the MAR method, which is effective only on selected non-absorbent surfaces10. Consequently, the study was conducted exclusively on flat, non-absorbent surfaces. Furthermore, the study did not include estimates for all potential blood loss volumes. A 150 ml scenario was added to the existing scenarios of 75 ml and 750 ml from the study by Merlin et al., which limited the generalizability of the findings. The quality indicators related to the MAR method (such as ideal application time and ideal fist height from the ground) are not yet clear. Therefore, the participants’ practices could not be standardized. Finally, the inclusion of only clinically inexperienced students as participants in the study provided valuable insights into the use of the MAR method as a clinical education tool; however, it limited the generalizability of the findings to the clinical practice of experienced professionals.
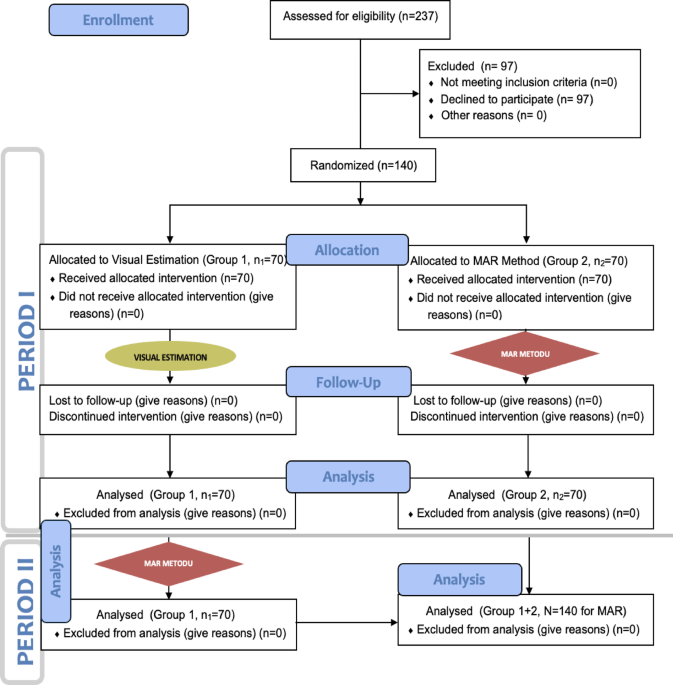
The primary strength of this study lies in its randomized controlled trial design, which enhances the reliability of the findings. Unlike the study by Merlin et al., this research analyzed both blood loss volume estimates and the time required for these estimations, addressing previously identified limitations. Furthermore, it explored the relationship between MAR estimates and physical variables such as gender, height, and weight, offering a more comprehensive understanding of the factors influencing estimation accuracy.
Interpretation
According to previous studies2,3,4,5,6,7,8,9,10,11, healthcare students and professionals have struggled to accurately predict external blood loss using the VE method due to its inherent limitations. Consistent with findings in the literature, the present study demonstrated that the VE method tended to overestimate simulated blood volumes in small (Station 1) and medium (Station 2) blood pools, while underestimating them in large blood pools (Station 3)2,3,7,15,16. Additionally, the VE method displayed higher standard deviations and more extreme minimum and maximum values, again in line with the literature10,19,20. In our study, both the extreme estimation values and the standard deviations obtained using the VE method were higher, consistent with findings in the existing literature.
In this study, the standard deviations of mean and extreme blood loss estimates with the MAR method decreased at Station 3 by 51% (intergroup) and 59% (intragroup); at Station 2 by 59% and 74%; and at Station 1 by 76% and 80%, respectively. These reductions were classified as moderate for Stations 2 and 3, and as maximum for Station 1. These findings were also consistent with the study by Merlin et al., in which they proposed the MAR method10. These results support Hypothesis 1 of this study. In intragroup analyses based on successive VE and MAR estimates from the same participants, the reduction observed in extreme estimates was greater than that in intergroup analyses based on single-method estimates from different participants. Similar to pre-post study designs, this may reflect a method effect; however, the potential impact of repeated measurements should not be overlooked. Therefore, the F1 LD F1 model, a nonparametric alternative to Repeated Measures Mixed ANOVA, was used for intergroup analyses, and the F2 LD F1 model, a nonparametric equivalent of Repeated Measures Two-way ANOVA, was applied for intragroup analyses, taking into account the repeated measures structure.
From a statistical perspective, a higher standard deviation indicates greater dispersion around the mean and reflects inconsistency in estimates across clinically comparable cases. The presence of extreme values further underscores the susceptibility of the VE method to both underestimation and overestimation errors. These findings suggest that the VE method exhibits considerable variability and reduced accuracy in quantifying blood loss during external bleeding.
Clinically, such variability has significant implications for the reliability and practical utility of the VE method in real-world scenarios. Accurate estimation of blood loss is essential for guiding timely and appropriate clinical interventions, particularly in emergency care, prehospital settings, trauma management, and surgical procedures. Overestimation may result in unnecessary interventions—such as fluid resuscitation or blood transfusion—whereas underestimation can delay critical treatment, increasing the risk of hypovolemic shock and other adverse outcomes. Therefore, the wide range and high variability inherent in VE outputs undermine its reliability as a standalone tool in clinical decision-making. These findings emphasize the need to complement VE with more objective, standardized, and validated methods when accurate blood loss assessment is required. On the other hand, the lower standard deviations and reduced number of outliers associated with the MAR method indicate that it may serve as a more reliable and consistent tool than the VE method for use in clinical settings.
When considering raw estimations of blood loss, there were no statistically significant differences between the two methods in either intergroup or intragroup analyses. However, based on error metrics such as mean difference, median differences, and percent error in Tables 5 ad 6, the MAR method enabled participants to estimate actual blood volumes in the stations more accurately. Improvements in estimations were evidenced by a reduction in differences (errors) relative to the actual blood volumes, and this was statistically significant. Furthermore, the MAR method minimized extreme values of blood loss estimates by reducing the interquartile ranges and standard deviations of differences (errors), thereby improving precision. The MAR method demonstrated greater accuracy in blood loss estimations than the VE method, regardless of whether the analysis was intergroup or intragroup, particularly on flat and nonabsorbent surfaces. These results support Hypothesis 1 of this study. These findings were also consistent with the study by Merlin et al.10.
Larger volumes, in particular, appear to cause greater estimation errors. At Station 3, where a volume of 750 ml was simulated, both the MAR and VE methods showed a tendency to underestimate the actual blood loss. The underestimation of higher blood loss volumes can be related to the difficulties inherent in both methods.
In the Visual Estimation (VE) method, large blood pools may cause perceptual saturation, making the volume appear smaller. Uniform color and blurred edges reduce contrast, and the absence of a reference object further impairs accuracy21. In the MAR method, the algorithm may have difficulty segmenting large, homogeneous blood areas, especially with unclear edges or low contrast10. Additionally, at higher volumes, blood may pool vertically, which the MAR method—based on two-dimensional surface area—does not capture, leading to further underestimation10.
To improve VE accuracy, training with reference images showing various volumes has been shown to significantly improve visual estimation skills22. The use of standardized reference objects as calibration tools (e.g., hand, paper, or ruler) also enhances estimation reliability23. In our study, the VE method served as the control group, whereas the MAR method, which utilizes the fist as a reference object, was designated as the experimental group.
For the MAR method, improved training and standardization are recommended to enhance its application and improve its accuracy10. Educational materials featuring varied blood loss scenarios across different surfaces can reduce user error. Furthermore, since blood behaves differently depending on the material (e.g., fabric, vinyl, wood), surface-specific calibration models that account for these properties could improve accuracy24. The estimation of blood loss should consider the non-linear behavior of fluid spreading24. As the volume of blood increases, the surface area covered does not expand proportionally. Beyond a certain threshold, blood begins to accumulate in depth rather than spreading uniformly, resulting in more prominent blood pooling rather than extended coverage. Moreover, surface-related factors—such as slope, texture, and absorbency—further influence the spreading pattern. The same amount of blood may form pools of different sizes (larger or smaller) depending on the characteristics of the surface. This variability highlights the importance of surface calibration and contextual interpretation in all visual, manual (like the MAR method), or algorithm-based blood loss estimation methods24.
In both intergroup and intragroup analyses, median estimation durations at Station 1 were similar for both methods. However, at Stations 2 and 3—where simulated blood loss was higher—the MAR method significantly increased estimation durations. Specifically, the mean estimation time with the MAR method increased by 270% (intergroup) and 290% (intragroup) at Station 3, by 87% and 96% at Station 2, and showed a slight change at Station 1 (a 3% decrease and 5% increase), respectively. Especially at Stations 2 and 3, the increases were classified as the maximum. The MAR method was associated with significantly longer estimation durations as compared with those using the VE method. The findings related to estimation durations supported this study’s Hypothesis 2. In the literature, no data could be found regarding the blood loss estimation times for either the VE method or the MAR method.
The MAR method required a longer estimation time, particularly in the high-volume scenario at Station 3. This may limit its practicality in time-sensitive clinical environments. While the MAR method enhances the accuracy of blood loss estimation by reducing estimation errors, outliers, and standard deviations, its time-related burden should be considered in the context of a trade-off analysis.
At Station 3, the average estimation time was approximately 34 s. In prehospital settings—especially during the management of patients in or at risk of hypovolemic shock, where rapid decision-making and intervention are critical—an estimation period of half a minute or longer may negatively impact clinical outcomes. Nevertheless, there appear to be no faster and more accurate alternatives to the MAR method in prehospital environments, and existing portable measurement devices may not be cost-effective for many institutions.
In hospital settings, methods such as venous blood gas analysis and complete blood count are frequently used alongside visual estimation to assess blood loss. However, despite variability between institutions, the average turnaround times for venous blood gas and complete blood count are typically 30 min25. Therefore, the MAR method may serve as a practical interim solution for estimating blood loss until more definitive laboratory results become available.
Merlin et al.10 predicted that demographic characteristics would affect blood loss estimations using the MAR method because it was developed based on males weighing over 70 kg and taller than 170 cm. Contrary to this prediction, gender, height, and weight variables did not affect the quantitative estimations using the MAR method in the present study. These findings did not support Hypothesis 3 in this study. In this study, median estimation durations using the MAR method at Station 1 did not differ significantly by demographic variables. However, at Stations 2 and 3, durations were significantly longer—by 23% and 47%, 19% and 21%, and 26% and 35%—for participants who were female, weighed less than 70 kg, and were shorter than 170 cm. These findings supported Hypothesis 4. These differences, observed as an increase in estimation durations, may be explained by the possibility that individuals with smaller body size and smaller fists needed more time to estimate larger blood volumes using the MAR method. However, the clinical significance of these differences remains unclear. No data were found in the literature on the relationship between blood loss estimates obtained using the MAR method and demographic variables such as gender, height, and weight.
Previous reports showed that training programs improved the ability of doctors and paramedics to predict visually the amount of external blood loss11,26,27,28,29. Therefore, incorporating basic MAR method training into clinical education and standardizing all aspects of its instruction appears to be valuable for both healthcare students and professionals. On the other hand, the inclusion of only clinically inexperienced students as participants in the MAR method’s clinical education study limits the generalizability of the findings regarding the MAR method to clinical practice. While the results offer valuable insights into the method’s applicability, predictive accuracy among novices, and using as a clinical skill within undergraduate medical and paramedic education, they should be interpreted within the context of a simulated environment and a non-clinician population.
Clinical settings are typically high-pressure and unpredictable. While experienced professionals are more likely to maintain consistent diagnostic reasoning and effective time management under stress, students may demonstrate greater variability in performance or experience cognitive overload. These differences should be taken into account, as they may lead to divergent outcomes when the MAR method is applied by trained clinicians in real-world conditions. However, in our reference study conducted by Merlin et al.10, the participants were healthcare professionals with an average of 10 years of combined training and clinical experience, and the findings were consistent with the primary results of our study, which was conducted with medical and paramedic students, and supported the effectiveness of the MAR method.
To enhance the external validity of the MAR method, future research should involve healthcare professionals with varying levels of clinical experience. Its application should be assessed in real clinical environments, such as emergency departments or prehospital care settings, with a focus on real patient management and patient-centered outcomes10,30.
Consequently, it seems worthwhile to identify departmental strategies in various health fields that could foster the MAR method’s ability to improve estimation accuracy as part of ongoing training programs and, if necessary, to formulate appropriate training programs (learning objectives, teaching techniques, training, and assessment). Nevertheless, validation of the MAR method under real-time, high-pressure conditions would provide a more robust understanding of its clinical utility, feasibility, and limitations in everyday practice.