Goodwin RD, Weinberger AH, Kim JH, Wu M, Galea S. Trends in anxiety among adults in the United States, 2008–2018: rapid increases among young adults. J Psychiatr Res. 2020;130:441. https://doi.org/10.1016/J.JPSYCHIRES.2020.08.014
Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among U.S. undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. 2019;65:590–8. https://doi.org/10.1016/J.JADOHEALTH.2019.04.033
Choi KW, Kim YK, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment. Adv Exp Med Biol. 2020;1191:219–35. https://doi.org/10.1007/978-981-32-9705-0_14/TABLES/1
Essau CA, Lewinsohn PM, Olaya B, Seeley JR. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J Affect Disord. 2014;163:125–32. https://doi.org/10.1016/j.jad.2013.12.033
Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, et al. Mental health problems in college freshmen: prevalence and academic functioning. J Affect Disord. 2018;225:97–103. https://doi.org/10.1016/J.JAD.2017.07.044
Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40:1086–93. https://doi.org/10.1097/00004583-200109000-00018
Krzyzaniak N, Greenwood H, Scott AM, Peiris R, Cardona M, Clark J, et al. The effectiveness of telehealth versus face-to face interventions for anxiety disorders: a systematic review and meta-analysis. J Telemed Telecare. 2024;30:250–61. https://doi.org/10.1177/1357633X211053738/ASSET/IMAGES/LARGE/10.1177_1357633X211053738-FIG8.JPEG
Adams SH, Schaub JP, Nagata JM, Park MJ, Brindis CD, Irwin CE. Young adult anxiety or depressive symptoms and mental health service utilization during the COVID-19 pandemic. J Adolesc Health. 2022;70:985–98. https://doi.org/10.1016/J.JADOHEALTH.2022.02.023
Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G, Waite P. Why do children and adolescents (not) seek and access professional help for their mental health problems? a systematic review of quantitative and qualitative studies. Eur Child Adolesc Psychiatry. 2021;30:183–211. https://doi.org/10.1007/S00787-019-01469-4
Goldsmith ES, Koffel E, Ackland PE, Hill J, Landsteiner A, Miller W, et al. Evaluation of implementation strategies for cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based stress reduction (MBSR): a systematic review. J Gen Intern Med. 2023;38:2782. https://doi.org/10.1007/S11606-023-08140-4
Wu A, Scult MA, Barnes ED, Betancourt JA, Falk A, Gunning FM. Smartphone apps for depression and anxiety: a systematic review and meta-analysis of techniques to increase engagement. NPJ Digital Medicine. 2021;4:1–9. https://doi.org/10.1038/s41746-021-00386-8
Chandrashekar P. Do mental health mobile apps work: evidence and recommendations for designing high-efficacy mental health mobile apps. Mhealth. 2018;4:6–6. https://doi.org/10.21037/MHEALTH.2018.03.02
Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? a meta-analysis of randomized controlled trials. J Affect Disord. 2017;218:15–22. https://doi.org/10.1016/J.JAD.2017.04.046
Andersson G, Carlbring P, Rozental A. Response and remission rates in internet-based cognitive behavior therapy: an individual patient data meta-analysis. Front Psychiatry. 2019;10. https://doi.org/10.3389/FPSYT.2019.00749/FULL
Weems CF, Hayward C, Killen J, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. J Abnorm Psychol. 2002;111:471–7. https://doi.org/10.1037/0021-843X.111.3.471
Moggia D, Lutz W, Kazantzis N, Schwartz B, Bakker D. Symptom reduction and engagement in a cognitive-behavioral mobile phone app: a study of user profiling to determine prognostic indicators. Behav Ther. 2024;55:217–32. https://doi.org/10.1016/J.BETH.2023.05.014
Mahon C, Howard E, O’Reilly A, Dooley B, Fitzgerald A. A cluster analysis of health behaviours and their relationship to mental health difficulties, life satisfaction and functioning in adolescents. Prev Med. 2022;164. https://doi.org/10.1016/J.YPMED.2022.107332
Shukla M, Pandey R. Identifying the transdiagnostic and unique domains of emotion regulation difficulties in subclinical conditions of anxiety and co-occurring anxiety-depression. Curr Psychol. 2021;40:2896–909. https://doi.org/10.1007/S12144-019-00224-X/FIGURES/3
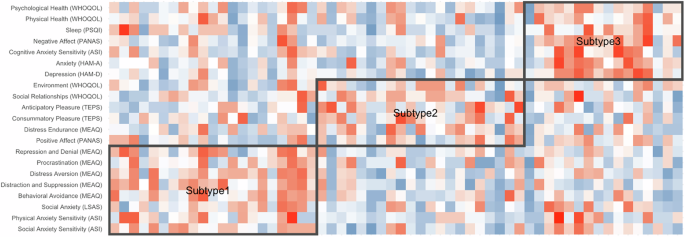
Taylor VA, Roy A, Brewer JA. Cluster-based psychological phenotyping and differences in anxiety treatment outcomes. Sci Rep. 2023;13:1–14. https://doi.org/10.1038/s41598-023-28660-7
Doron J, Thomas-Ollivier V, Vachon H, Fortes-Bourbousson M. Relationships between cognitive coping, self-esteem, anxiety and depression: a cluster-analysis approach. Pers Individ Dif. 2013;55:515–20. https://doi.org/10.1016/J.PAID.2013.04.017
Contardi A, Farina B, Fabbricatore M, Tamburello S. Difficulties in emotion regulation and personal distress in young adults with social anxiety. Riv Psichiatr. 2013;48:155–61. https://doi.org/10.1708/1272.14040
Solomonov N, Lee J, Banerjee S, Chen SZ, Sirey JA, Gunning FM, et al. Course of subtypes of late-life depression identified by bipartite network analysis during psychosocial interventions. JAMA Psychiatry. 2023;80:621–9. https://doi.org/10.1001/JAMAPSYCHIATRY.2023.0815
Bress JN, Falk A, Schier MM, Jaywant A, Moroney E, Dargis M, et al. Efficacy of a mobile app-based intervention for young adults with anxiety disorders: a randomized clinical trial. JAMA Netw Open. 2024;7:e2428372. https://doi.org/10.1001/JAMANETWORKOPEN.2024.28372
Brown TA, Barlow DH. Anxiety and related disorders interview schedule for DSM-5 (ADIS-5) – adult and lifetime version. 2014. https://books.google.com/books?hl=en&lr=&id=8fhQEAAAQBAJ&oi=fnd&pg=PP1&dq=adis+brown+barlow&ots=9eq7VdJLEe&sig=una-QUX6eZuvmxjO_uqd4C0aJz8#v=onepage&q=adis%20brown%20barlow&f=false. Accessed Aug 6 2024
WHO Collaborating Centre for Drug Statistics Methodology. ATCDDD. 2025. https://atcddd.fhi.no/?. Accessed Feb 3 2025
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. https://doi.org/10.1111/J.2044-8341.1959.TB00467.X
Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14:61–68. https://doi.org/10.1016/0165-0327(88)90072-9
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. https://doi.org/10.1136/JNNP.23.1.56
Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am J Psychiatry. 2004;161:2163–77. https://doi.org/10.1176/APPI.AJP.161.12.2163
Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial a report from the WHOQOL Group. Qual Life Res. 2004;13:299–310. https://doi.org/10.1023/B:QURE.0000018486.91360.00/METRICS
Gámez W, Chmielewski M, Kotov R, Ruggero C, Watson D. Development of a measure of experiential avoidance: the Multidimensional Experiential Avoidance Questionnaire. Psychol Assess. 2011;23:692–713. https://doi.org/10.1037/A0023242
Carpenter JS, Andrykowski MA. Psychometric evaluation of the pittsburgh sleep quality index. J Psychosom Res. 1998;45:5–13. https://doi.org/10.1016/S0022-3999(97)00298-5
Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. 2007;19:176–88. https://doi.org/10.1037/1040-3590.19.2.176
Watson D, Clark LA, Tellegen A. Development and Validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–70. https://doi.org/10.1037/0022-3514.54.6.1063
Heubeck BG, Wilkinson R. Is all fit that glitters gold? comparisons of two, three and bi-factor models for Watson, Clark & Tellegen’s 20-item state and trait PANAS. Pers Individ Dif. 2019;144:132–40. https://doi.org/10.1016/J.PAID.2019.03.002
Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. 2004;43:245–65. https://doi.org/10.1348/0144665031752934
Gard DE, Gard MG, Kring AM, John OP. Anticipatory and consummatory components of the experience of pleasure: a scale development study. J Res Pers. 2006;40:1086–102. https://doi.org/10.1016/J.JRP.2005.11.001
Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987;22:141–73. https://doi.org/10.1159/000414022
Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, et al. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychol Med. 1999;29:199–212. https://doi.org/10.1017/S0033291798007879
Goldberg SB, Baldwin SA, Riordan KM, Torous J, Dahl CD, Davidson RJ, et al. Alliance with an unguided smartphone app: validation of the digital working alliance inventory. Assessment. 2022;29:1331–45. https://doi.org/10.1177/10731911211015310
Stoyanov SR, Hides L, Kavanagh DJ, Wilson H. Development and validation of the user version of the mobile application rating scale (uMARS). JMIR Mhealth Uhealth. 2016;4:e5849. https://doi.org/10.2196/mhealth.5849
Fern XZ, Brodley CE. Solving cluster ensemble problems by bipartite graph partitioning. In: Proceedings of the 21st International conference on machine learning. (Guruswami V. et al.) (ACM Digital Library, 2004)
Jordano P. ggbipart: An R package for plotting bipartite networks. (Version 2.18). (2025). Accessed August 6, 2024. Available from https://pedroj.github.io/bipartite_plots/.
Beckett SJ. Improved community detection in weighted bipartite networks. R Soc Open Sci. 2016;3. https://doi.org/10.1098/rsos.140536
Dormann CF, Gruber B, Fründ J. Introducing the bipartite package: analysing ecological networks. 2008. Accessed Aug 6 2024. http://erzuli.ss.uci.edu/R.stuff
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. 2023. https://www.R-project.org/ Accessed Feb 3 2025
Csardi G, Nepusz T. The igraph software package for complex network research. InterJournal, complex systems. 2006. https://igraph.org. Accessed Feb 3 2025
Dormann CF, Gruber B, Fründ J. Introducing the bipartite package: analysing Ecological Networks. 2008. http://erzuli.ss.uci.edu/R.stuff. Accessed Feb 3 2025
Solomonov N. Improving social reward responsivity and social connectedness in psychotherapies for late-life depression: engage & connect as an example. Psychiatry Res. 2023;329:115469. https://doi.org/10.1016/J.PSYCHRES.2023.115469
Khazanov GK, Xu C, Dunn BD, Cohen ZD, DeRubeis RJ, Hollon SD. Distress and anhedonia as predictors of depression treatment outcome: a secondary analysis of a randomized clinical trial. Behav Res Ther. 2020;125:103507. https://doi.org/10.1016/J.BRAT.2019.103507
Renna ME, Quintero JM, Fresco DM, Mennin DS. Emotion regulation therapy: a mechanism-targeted treatment for disorders of distress. Front Psychol. 2017;8:6. https://doi.org/10.3389/FPSYG.2017.00098
Stein AT, Carl E, Cuijpers P, Karyotaki E, Smits JAJ. Looking beyond depression: a meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychol Med. 2021;51:1491–504. https://doi.org/10.1017/S0033291720000239
Moberg C, Niles A, Beermann D. Guided self-help works: randomized waitlist controlled trial of pacifica, a mobile app integrating cognitive behavioral therapy and mindfulness for stress, anxiety, and depression. J Med Internet Res. 2019;21. https://doi.org/10.2196/12556
Stjerneklar S, Hougaard E, Thastum M. Guided internet-based cognitive behavioral therapy for adolescent anxiety: predictors of treatment response. Internet Interv. 2019;15:116. https://doi.org/10.1016/J.INVENT.2019.01.003
Webb CA, Hirshberg MJ, Davidson RJ, Goldberg SB. Personalized prediction of response to smartphone-delivered meditation training: randomized controlled trial. J Med Internet Res. 2022;24:e41566. https://doi.org/10.2196/41566
Webb CA, Swords CM, Lawrence HR, Hilt LM. Which adolescents are well-suited to app-based mindfulness training? a randomized clinical trial and data-driven approach for personalized recommendations HHS Public Access. J Consult Clin Psychol. 2022;90:655–69. https://doi.org/10.1037/ccp0000763
Kooiman BEAM, Robberegt SJ, Albers CJ, Bockting CLH, Stikkelbroek YAJ, Nauta MH. Congruency of multimodal data-driven personalization with shared decision-making for StayFine: individualized app-based relapse prevention for anxiety and depression in young people. Front Psychiatry. 2023;14:1229713. https://doi.org/10.3389/FPSYT.2023.1229713/BIBTEX
Bell I, Arnold C, Gilbertson T, D’Alfonso S, Castagnini E, Chen N, et al. A personalized, transdiagnostic smartphone intervention (Mello) targeting repetitive negative thinking in young people with depression and anxiety: pilot randomized controlled trial. J Med Internet Res. 2023;25. https://doi.org/10.2196/47860.
Scott AJ, Bisby MA, Heriseanu AI, Hathway T, Karin E, Gandy M, et al. Understanding the untreated course of anxiety disorders in treatment-seeking samples: a systematic review and meta-analysis. J Anxiety Disord. 2022;89. https://doi.org/10.1016/J.JANXDIS.2022.102590