To the best of our knowledge, this is the first study in Vietnam to investigate the role of clinical pharmacy services (CPS) in optimizing prescribing for elderly patients with diabetes in a hospital setting. While previous studies have reported the effectiveness of CPS in managing diabetic patients [16], there is a lack of evidence specifically addressing elderly patients with diabetes. This population was selected as the target for CPS because they are particularly vulnerable to drug-related problems (DRPs) and suboptimal prescribing due to multiple risk factors, including polypharmacy, age-related physiological changes, and comorbidities.
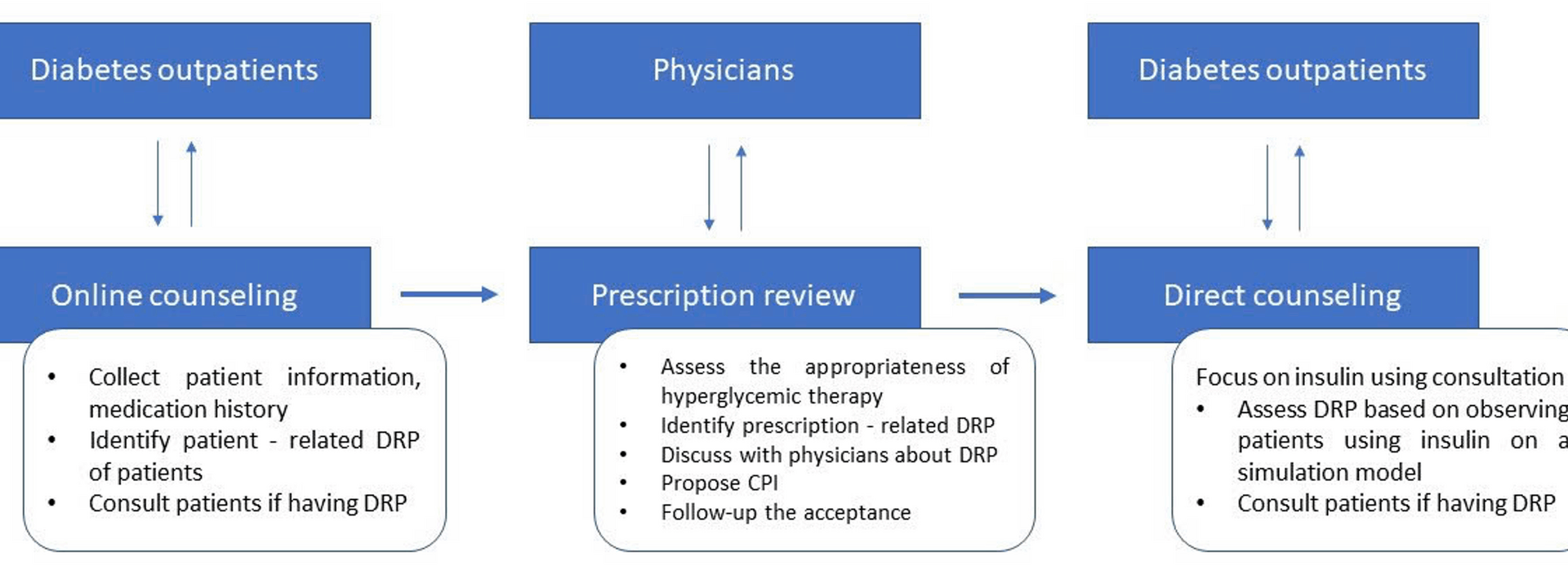
As highlighted in earlier research, pharmaceutical care services for individualized patients have not yet been standardized in Vietnamese hospitals [17,18,19]. In low- and middle-income countries like Vietnam, one of the most significant barriers to implementing CPS in hospitals is the shortage of human resources [17,18,19]. Efforts should focus on tailoring CPS interventions to local needs and ensuring equitable access to these services. In this study, with only 0.5 full-time equivalent (FTE) pharmacist, we developed a structured CPS process for elderly diabetic patients who did not achieve their target HbA1c levels to ensure sustainability, time efficiency, and effectiveness.
Identification and resolution of drug-related problems (DRPs)
A total of 231 drug-related problems (DRPs) were identified in the study population, with the majority classified under patient-related causes (66.2%), followed by issues in drug selection (21.2%) and dose selection (12.6%). Among the patient-related DRPs, the most prevalent issue was unintentional incorrect use of medication, particularly insulin (28.6%), which, although rated as minor in clinical significance in all cases, may indicate a widespread gap in patient understanding or education regarding proper administration techniques. This finding is consistent with prior studies that have reported insulin administration errors to be highly prevalent among elderly patients with diabetes [20, 21], often due to visual impairment, reduced dexterity, or limited caregiver support [22, 23].
Another noteworthy patient-related problem was intentional non-adherence, observed in 14.7% of cases, where patients either took less than the prescribed dose or omitted doses altogether. While most cases were rated as minor or moderate in clinical significance, even low-severity non-adherence can contribute to long-term suboptimal glycemic control, increased risk of complications, and poor quality of life. These patterns of behavior may stem from concerns about adverse effects, medication cost, or misunderstanding of treatment necessity—factors previously documented in elderly populations with chronic conditions [24].
Inappropriate dosing also emerged as a relevant category, with 10.4% of DRPs attributed to doses being too low and 2.2% to excessively high doses of single active ingredients. Although only a portion of these were classified as major in clinical significance, inappropriate dosing in elderly patients poses substantial risks due to age-related changes in pharmacokinetics and pharmacodynamics. Clinical pharmacists, through medication review and dose optimization, play a critical role in preventing these errors and ensuring safe and effective therapy [25].
The most clinically significant DRPs were related to inappropriate drug selection according to guidelines, with 39 out of 49 cases classified as moderate in significance. This highlights the ongoing need for evidence-based prescribing and interdisciplinary collaboration, particularly in elderly patients with multiple comorbidities where therapeutic complexity is high. Studies have shown that pharmacist-led medication reviews contribute significantly to the identification and correction of such prescribing discrepancies [26,27,28,29].
Among 78 interventions proposed by clinical pharmacists, more than half (53.9%) were accepted and implemented by physicians, with an additional 39.7% accepted but not implemented, suggesting a high level of concordance in clinical judgment, even if logistical or patient-related factors may have delayed action. Notably, recommendations to add drugs to meet individualized targets and increase doses accounted for a large proportion of interventions, with acceptance and implementation rates of 51.5% and 54.2%, respectively. This indicates a moderate uptake of pharmacist input in optimizing therapy, yet also reflects the complexity of managing elderly patients, in whom comorbidities and risk of adverse effects may influence prescribing decisions. Importantly, interventions aimed at preventing hypoglycemic adverse drug reactions, such as stopping or adjusting medications, had full acceptance and implementation, emphasizing physician responsiveness to safety-oriented recommendations.
Overall, the clinical significance of the identified DRPs and the high rate of acceptance of CPI underscore the importance of integrating clinical pharmacy services into outpatient diabetes care. Although many DRPs were categorized as minor, the cumulative effect of unresolved issues—especially those involving insulin use and adherence—can substantially affect patient outcomes. These findings support previous research advocating for structured pharmacist interventions, patient counseling, and medication reconciliation as essential components of chronic disease management in elderly populations [30].
Improvement in HbA1c target
A finding of this study was the improvement in glycemic control among elderly outpatients with type 2 diabetes following the implementation of CPS. Notably, the proportion of patients achieving individualized HbA1c targets increased from 0% at baseline to 22.9% after the intervention, a statistically significant improvement (p < 0.05). Although the reduction in the proportion of patients with HbA1c ≥ 8.5%—from 49.2% to 32.2%—did not reach statistical significance, this downward trend remains clinically meaningful, particularly in the context of a high-risk elderly population with complex therapeutic needs.
These findings are consistent with previous international studies demonstrating the positive impact of pharmacist-led interventions on glycemic outcomes [31,32,33,34,35,36,37,38]. A systematic review by Wubben and Vivian reported that clinical pharmacy services were associated with reductions in HbA1c ranging from 0.5% to 1.8% across various outpatient settings [1, 39]. Similarly, a meta-analysis by Bongaerts et al. confirmed that pharmacist-led diabetes care significantly improved HbA1c levels, particularly when interventions incorporated patient education, medication review, and physician collaboration [2, 40]. The observed improvements in our study are particularly notable given the advanced age and high baseline HbA1c levels of the study population, which are often associated with diminished responsiveness to standard interventions.
From a clinical perspective, these improvements are meaningful. The UK Prospective Diabetes Study (UKPDS) demonstrated that every 1% reduction in HbA1c was associated with a 37% decrease in microvascular complications and a 14% reduction in the risk of myocardial infarction [3, 41]. In older adults, who are especially vulnerable to both hyperglycemia-related complications and treatment-related harms such as hypoglycemia, achieving individualized targets—as opposed to strict glycemic control—can help optimize benefit while minimizing risk. In this context, the role of clinical pharmacists in providing tailored education, identifying drug-related problems, and supporting individualized care plans is both clinically valuable and cost-effective.
Importantly, these findings support current international guidelines, including those from the American Diabetes Association (ADA) and the International Diabetes Federation (IDF), which emphasize the importance of setting individualized HbA1c goals in older adults based on comorbidity burden, functional status, and life expectancy [5, 42]. This study demonstrates that such guideline recommendations can be effectively operationalized in low-resource settings through the integration of clinical pharmacy services into routine outpatient care.
Collaboration and interdisciplinary care
The findings from the satisfaction survey indicate a high level of acceptance and perceived value of clinical pharmacy services (CPS) among both physicians and patients. Notably, all participating physicians (100%) expressed satisfaction with the knowledge and skills of the clinical pharmacists, and unanimously agreed that CPS positively influenced prescribing quality and that they would be willing to continue participating in such services in the future. These results underscore the potential of CPS to foster collaborative prescribing practices and enhance physician confidence in pharmaceutical care integration—an essential factor for the sustainability of pharmacist-led interventions in outpatient settings. Similar findings have been reported in previous studies, where physician support was identified as a key facilitator for successful CPS implementation and interprofessional collaboration [43, 44].
Among patients, satisfaction was also remarkably high, with 95.2% expressing overall satisfaction and 85.4.% indicating willingness to continue engaging with CPS in the future. High levels of satisfaction were observed across multiple dimensions, including perceived convenience (85.4%) and pharmacist competence (82.9%). These results are consistent with international literature suggesting that patient satisfaction is strongly influenced by the quality of communication, individualized attention, and perceived improvements in medication understanding and self-management [26, 45]. Moreover, the finding that 68.3% of patients believed CPS had a positive impact on their medication use reflects not only the clinical benefits of pharmacist intervention but also its perceived relevance and credibility from the patient perspective.
However, a notable finding was that less than half of the patients (46.3%) agreed to pay for pharmacist consulting services. This suggests that while CPS is well-received in terms of quality and utility, financial acceptability may pose a barrier to broader implementation, particularly in resource-limited settings. Previous studies in similar contexts have shown that patients’ willingness to pay is influenced by factors such as health insurance coverage, perceived cost-effectiveness, and prior exposure to pharmacist-led care [46]. These insights point to the need for policy-level support, including CPS reimbursement models or integration into national health coverage schemes, to ensure long-term viability.
Overall, the high satisfaction rates from both physicians and patients provide strong justification for the continued expansion of CPS in outpatient diabetes management. In particular, these findings support the role of clinical pharmacists not only as medication experts but also as accessible healthcare providers capable of enhancing care quality, promoting patient engagement, and strengthening interdisciplinary practice.
Study limitations
While the findings of this study are promising, several limitations must be acknowledged. The single-center design and relatively small sample size may limit the generalizability of the results. Given the real-world implementation nature of this study and the lack of a comparator arm, findings should be interpreted cautiously. The number of detected drug-related problems (DRPs) and the physicians’ acceptance rate were significantly influenced by the pharmacist’s expertise, communication skills, and the physicians’ perception of clinical pharmacy services (CPS). Furthermore, the study did not assess the impact of CPS using solid clinical endpoints (e.g., mortality, morbidity) nor did it calculate the costs associated with the service (e.g., healthcare utilization) or the patients’ quality of life. Instead, process parameters, including the number of identified DRPs, the physicians’ acceptance rate, and the clinical significance of DRPs, were employed to demonstrate the benefits of CPS in this preliminary study. The patient and physician surveys also have several limitations. First, they were conducted using convenience sampling with a small number of participants (n = 41 for patients), without formal sample size calculation, which limits the generalizability of findings. Second, the use of self-reported measures introduces potential recall and response bias, particularly for subjective outcomes such as satisfaction.
Despite these limitations, the findings provide valuable evidence suggesting that CPS is likely to bring benefits to patients in Vietnam. Future studies should aim to address these limitations by including larger, multi-center cohorts and objective measures of adherence and satisfaction.
Future research should also explore the long-term sustainability of CPS, its cost-effectiveness, and its application to other chronic conditions beyond diabetes. Policymakers should prioritize the integration of CPS into healthcare systems and allocate resources to expand these services. Additionally, healthcare providers should be encouraged to embrace CPS as a valuable component of chronic disease management.