The updated colonoscopy clinical care standard features new guidance on My Health Record.
An updated clinical care standard for colonoscopy has landed, just as new data paints a picture of growing access inequality across the country.
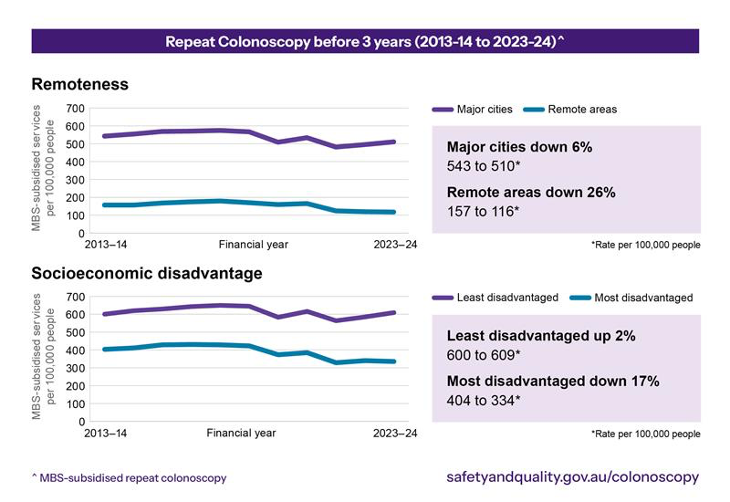
According to an Australian Commission on Safety and Quality in Health Care (ACSQHC) report presented at the World Congress of Gastroenterology and Australian Gastroenterology Week 2025 in Melbourne on Sunday, the past decade has seen an 8% decrease in the number of people receiving MBS-subsidised repeat colonoscopies within three years of their original colonoscopy.
This overall decrease was far more pronounced in areas of socio-economic disadvantage and in rural areas.
Australians living in major cities went from receiving around 543 early repeat colonoscopies per 100,000 people in 2013 to receiving 510 early repeat colonoscopies per 100,000 people in 2023, representing a 6% decrease.
For rural Australians, the rate went from 157 early repeat colonoscopies per 100,000 people in 2013 to 116 early repeat colonoscopies per 100,000 people in 2023, representing a 26% decrease.
Where the proportion of people in Australia’s least disadvantaged regions who received an early repeat colonoscopy increased by 2% over the decade, the proportion of people in Australia’s most disadvantaged regions who received an early repeat colonoscopy decreased by 17%.
While there is no hard number on exactly how many people should be having a repeat colonoscopy within three years, GP and ACSQHC medical advisor Dr Phoebe Holdenson Kimura said the levels of variation between groups were cause for concern.
“There’s so much variation that it does make us wonder whether some people, particularly in affluent areas, might be receiving repeat colonoscopy too early, unnecessarily,” she told The Medical Republic.
“And equally, [are there] people in those geographically more remote or rural areas, or people in less affluent areas that perhaps do need that repeat colonoscopy, but for whatever reason, they’re not having it?
“I think, potentially, we’re seeing both of those things happen.”
The Cancer Council guidelines around surveillance colonoscopy put the interval between initial colonoscopies at either one year, three years, five years or 10 years.
“If we’re really adhering to those guidelines fairly closely, then we would only see a small number of people requiring a repeat colonoscopy before three years,” Dr Holdenson Kimura said.
“For the purpose of this particular analysis, we’ve decided to make it two years and 10 months, just to allow a little bit of leeway so we’re not counting patients who’ve had it a few months early for a logistical reason, which we don’t think is an issue.”
Dr Holdenson Kimura encouraged GPs to use the interactive data map published by the ACSQHC to get a clearer picture of whether people in their immediate area were receiving early repeat colonoscopies.
“You can actually interrogate the data and see how the data compares between where you work or … [look] at the population which you serve, and go, ‘this rate is very similar to the rates around us’, or perhaps it’s quite different,” she said.
“And [you can think about] what are the potential causes for that, but also what are the ways that the service can adapt to try and meet the needs of its population?
“Understanding the problem and articulating the problem is the first step … particularly since we’re seeing that disparity, unfortunately, appears to be widening over the last 10 years.”
While she acknowledged that no one GP could solve the issue of access and affordability, Dr Holdenson Kimura said there was a role for GPs to play in advocating for patients they were concerned about.
“In Australia, only four in 10 eligible people are actually participating in bowel cancer screening,” the GP said.
“We know that when GPs have conversations with their patients about screening, patients trust their advice.
“They want to follow through on it and it, it’s really the thing that makes the biggest difference.
“And then off the back of a positive faecal occult blood test or the screening test, the GP plays a critical role in referring that patient to have a colonoscopy with really a high-quality referral.”
Guidance on comprehensive referrals makes up the first part of the new colonoscopy clinical care standard.
The standards now state that each referral should include an indication, presenting symptoms and the clinical concern, results of previous investigations, all relevant medical and family history, current medicines and previous relevant treatment.
“Those are the sorts of things that can make sure that it’s a safe transition of care for the patient between the primary and the secondary sector,” Dr Holdenson Kimura said.
“And then I think the other big part that GPs can play – looking particularly at this repeat colonoscopy issue – is that we know that for patients who have had their colonoscopies … might be confused or they may not actually know what the plan is for follow up.
“The clinical care standard, in the final quality statement, talks really explicitly about the need for clear communication with the patient and written communication as well, but also for the colonoscopist to be proactively communicating with the GP.”
One of the key additions to the new version of the care standard is a directive to upload the report and results to each patient’s healthcare record and My Health Record.
