A new mRNA approach successfully restored sperm production and led to the birth of viable offspring in a genetic mouse model.
The technique has been developed by the University of Osaka, Japan, in collaboration with Baylor College of Medicine, the US.
This new therapy addresses non-obstructive azoospermia (NOA), a form of genetic male infertility characterized by a complete failure or halt in sperm production. The condition currently has very few available treatment options.
Interestingly, the treatment successfully targeted specific testicular genes in a mouse model, thereby restoring sperm production and leading to the birth of viable offspring.
“It introduces a safer, non-integrating alternative to traditional gene therapies, providing hope for untreatable infertility cases in humans,” the researchers noted in the study.
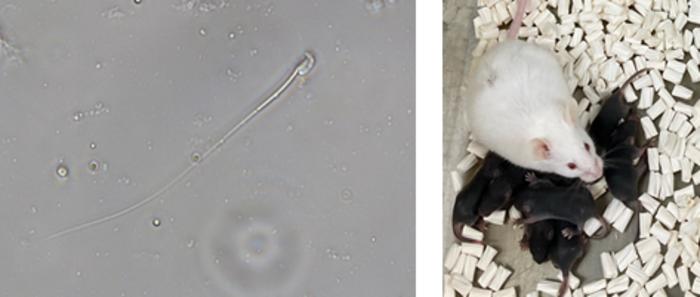 Recovered sperm and offspring obtained via intracytoplasmic sperm injection (ICSI). Mashiko et al., 2025
Recovered sperm and offspring obtained via intracytoplasmic sperm injection (ICSI). Mashiko et al., 2025
Targeting sperm-producing cells in mRNA therapy
Infertility is a major global health issue, affecting one in six couples worldwide, with roughly half of all cases attributed to male factors.
One of the most severe forms of male infertility is NOA, where a man has a complete lack of sperm in his ejaculate despite having normal hormone levels.
This condition is primarily caused by genetic defects that severely disrupt or halt the complex process of sperm production, known as spermatogenesis.
Due to its underlying genetic nature, treatment options for NOA are currently limited, leaving thousands of affected individuals without a biological path to father children.
The new research focused on an NOA mouse model specifically designed to mimic human genetic deficiencies causing meiotic arrest — a stage where sperm production stalls.
The deficiency was caused due to defects in the Pdha2 gene.
The team employed a novel method using lipid nanoparticles (LNPs) to deliver messenger RNA (mRNA) directly to the testes.
The LNPs were injected carrying the Pdha2 mRNA into the rete testis to ensure broad delivery throughout the seminiferous tubules.
A key innovation involved modifying the mRNA with a specific sequence (Dsc1 3’-UTR) to direct its expression predominantly to germ cells, the cells responsible for producing sperm, rather than supporting Sertoli cells.
This targeted delivery proved crucial for the treatment’s success.
“Using fully synthetic LNPs to deliver mRNA minimizes genome-integration concerns and enables us to restore spermatogenesis in a defined genetic model,” said Professor Masahito Ikawa, senior author of the study.
Healthy pups
Within two weeks of treatment, the Pdha2 knockout mice, which initially exhibited meiotic arrest, showed a resumption of meiotic progression.
It led to the formation of round spermatids, and by three weeks, mature sperm were successfully produced.
The ultimate test of the treatment’s efficacy came with fertilization.
Sperm retrieved from the treated mice were used for intracytoplasmic sperm injection (ICSI), resulting in 26 healthy pups from 117 embryos.
These offspring developed normally, were fertile, and showed “no large genomic alterations.” The findings showcase the safety and precision of the LNP-mRNA delivery system.
“These findings clarify how spermatogenesis can be rescued and lay the groundwork for applied research toward treating certain forms of male infertility,” said Professor Martin M. Matzuk.
This study is a major step forward in reproductive medicine. The LNP-mediated mRNA delivery system could offer a hopeful pathway for future human therapies for genetically driven male infertility.