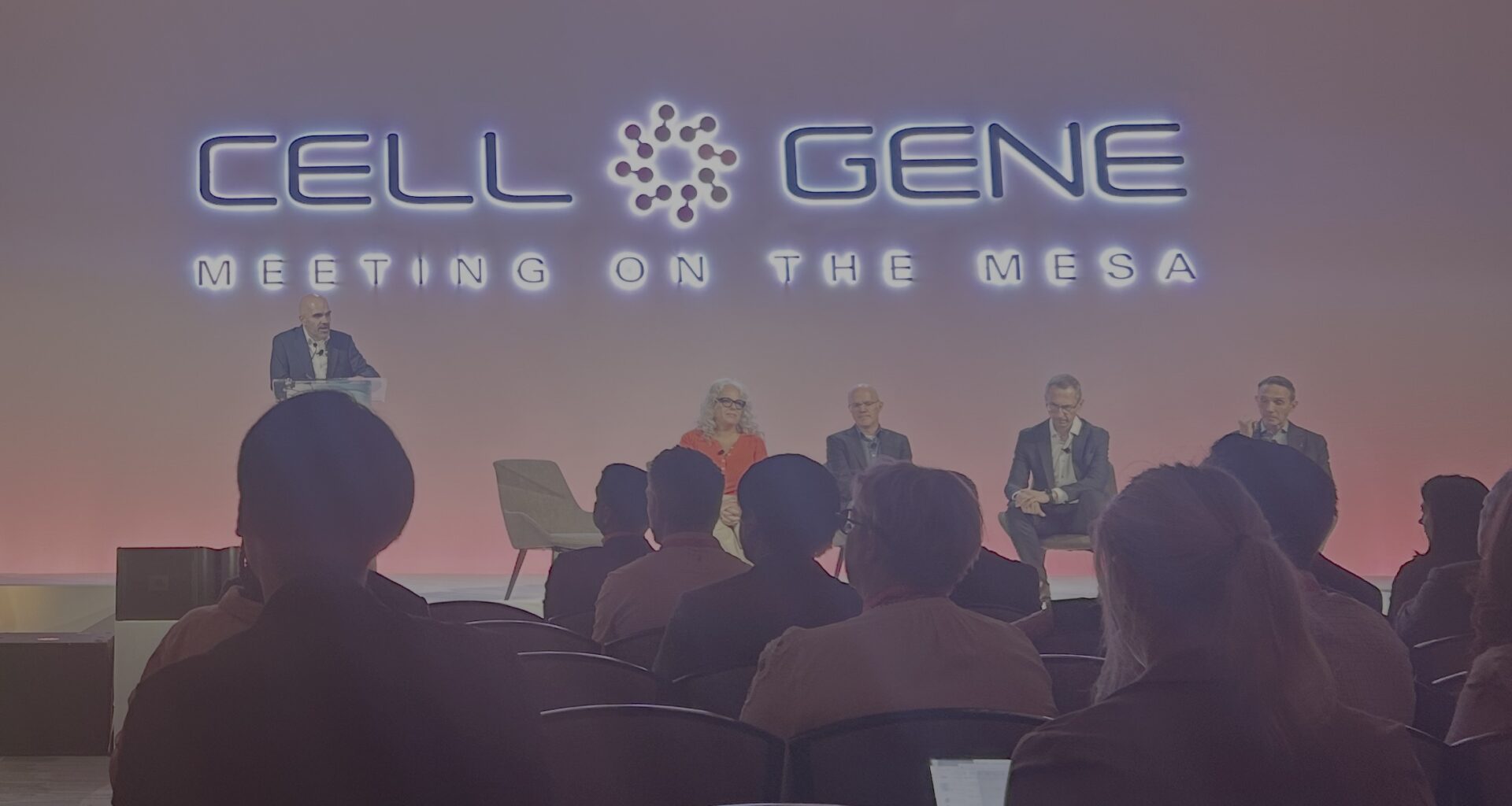
As gene editing enters a new era, leaders discuss Baby KJ’s implications for families, science, and industry. (Left to right): Sadik Kassim, PhD, Chief Scientific Officer and Chief Technology Officer, Danaher Genomic Medicines; Maria Kefalas, PhD, Founder, MLD Voices and The Callope Joy Foundation; Devyn Smith, PhD, CEO, Arbor Biotechnologies; Fyodor Urnov, PhD, Director, Technology and Translation, Innovative Genomics Institute and Professor, MCB Department, University of California, Berkeley; Tom Wilton, Senior Vice President, Innovation Ventures, Children’s Hospital of Philadelphia (Credit: Jonathan D. Grinstein)
As gene editing enters a new era, leaders discuss Baby KJ’s implications for families, science, and industry. (Left to right): Sadik Kassim, PhD, Chief Scientific Officer and Chief Technology Officer, Danaher Genomic Medicines; Maria Kefalas, PhD, Founder, MLD Voices and The Callope Joy Foundation; Devyn Smith, PhD, CEO, Arbor Biotechnologies; Fyodor Urnov, PhD, Director, Technology and Translation, Innovative Genomics Institute and Professor, MCB Department, University of California, Berkeley; Tom Wilton, Senior Vice President, Innovation Ventures, Children’s Hospital of Philadelphia (Credit: Jonathan D. Grinstein)
 Jonathan D. Grinstein, PhD, North American Editor, Inside Precision Medicine
Jonathan D. Grinstein, PhD, North American Editor, Inside Precision Medicine
PHOENIX – At last year’s Cell and Gene Meeting on the Mesa in Phoenix, people were sweating, and it wasn’t just because of the 100°F heat in October. Following Vertex’s Casgevy for sickle cell’s approval as the first CRISPR-based medicine in December 2023, the field had been quiet. There was desperation to move from cell and gene therapy concepts to the new clinical standard of treatment.
Investors were taking notice. The stock market trends for many cell and gene therapy companies have been going downhill since late 2023. For example, the week following the Casgevy approval, gene editing companies Intellia and Editas had stock prices of $30.78 and $10.93, respectively. By summer 2025, Intellia would drop to $5.90, and Editas would reach a low of $0.91—or less than 10% of its value in a year and a half. Until a few weeks ago, many cellular and genetic medicine companies’ stocks had reached their lowest point ever.
For cellular and genetic medicine developers, creating the bridge from chalkboard ideas and promising preclinical glimmer to the next generation of clinical standards was beginning to feel like an insurmountable feat, at least with the amount of cash left. The focus of the 2024 meeting became less about the science and more about survival. The decimation of the leadership at the Center for Biologics Evaluation and Research (CBER) surely hasn’t helped.
Market conditions aside, this year, there was a different mood over a three-day stretch at the 2025 Cell and Gene Meeting on the Mesa. From the moment I stepped foot into the five-star Arizona Biltmore for a second time, there was a calm simmer of earnest optimism among the 2,000 attendees, about a third of whom were C-level executives. Unlike last year, when most interviews seemed to revolve around developing iterations of CAR T and NK cells, this year’s discussions were based on innovation in delivery technology and the strategies and frameworks to bring cellular and genetic medicines to those who need them. The individuals who persevered with ingenuity and rigor appeared to be on the verge of a clinical breakthrough.
Here are my highlights from presentations and interviews at the 2025 Cell and Gene Meeting on the Mesa.
A gust of tailwinds
If the financial market wasn’t tough enough already, a year with several widely reported patient deaths linked to gene therapy has caused additional investor angst. Yet, Edinburgh-based Trogenix, a clinical-stage genetic medicine company, announced a $95 million Series A financing to support the clinical development of its gene therapies for aggressive cancers. Trogenix’s first products deliver an adeno-associated virus (AAV) directly into solid tumors, expressing a combination of immune payloads—essentially a viral immunotherapy—as opposed to the gene replacement or modification strategies often used to treat monogenic diseases.
Trogenix’s secret sauce addresses a fundamental challenge to genetic medicine approaches—safe and specific cell targeting. To do so, Trogenix uses synthetic super enhancers (SSEs), large clusters of enhancers densely occupied by regulatory proteins to drive robust expression of specific genes, often those that define cell identity. Trogenix CEO Ken Macnamara, PhD, explained to Inside Precision Medicine, “The unique precision comes from SSEs—a genomic ‘switch’ that’s selective not just for a cell type, but for the most aggressive cancer stem cell state.”
The company’s Odysseus platform maps transcriptional networks defining disease states and engineers SSEs only 160 bp in length to turn on the right immune payloads only in those cells. By integrating AI-driven discovery with synthetic biology, Trogenix can rapidly design, test, and iterate candidate therapeutic AAVs. “We can build and test hundreds of vectors in a living tissue context, showing selectivity against patient-derived tumor samples,” said Macnamara. “We’re not just hitting the tumor core—we’re clearing infiltrating cells in the surrounding margin while sparing healthy neurons and astrocytes.”
That selectivity allows Trogenix to target the “apex of the tumor hierarchy”—the master transcriptional networks that drive cancer’s self-renewal and resistance. “To truly achieve curative responses, we need to tackle multiple hallmarks of cancer simultaneously,” Macbanara said. Trogenix’s name reflects its philosophy: the “Trojan horse” strategy of slipping therapeutic genes into the tumor to trigger an immune assault from within. “We’re not trying to kill every cancer cell directly,” Macnamara said. “We’re opening the gates to the immune system.”
Preclinical studies using Trogenix’s SSEs have shown long-lasting immune memory, no off-target toxicity, and full tumor clearance at higher doses. “At low doses, we saw residual tumors surrounded by lymphocytes—evidence that the immune system had been re-educated to keep the cancer in check,” he said. “At higher doses, we saw complete responses.”
Trogenix’s lead program targets glioblastoma (GBM), supported by extensive patient-derived cell lines developed through Cancer Research UK. A Phase I/II clinical trial is already designed to identify an optimal biological dose and expand to newly diagnosed and recurrent GBM patients. “By 29 weeks, we expect registration-quality data,” Macnamara said. “It’s a model for how gene therapies could reach patients faster.”
Getting to the finish line
When Alain Reine, MD, joined Prime Medicine in early 2024—initially as CFO—he wasn’t seeking a young, preclinical platform company. But the science of prime editing changed his mind. “As I dug in, I was blown away,” Reine told Inside Precision Medicine. “This technology isn’t just another version of CRISPR—it can fix mutations that no other editing tool can touch.”
Still, the company needed direction. When Reine arrived, Prime had roughly 18 active programs and was spread too thin. “We had brilliant scientists, but we needed focus,” he said. Over his first four months, he led what he called a “value framework exercise”—a deep review of every program across technical feasibility, clinical tractability, competition, and commercial potential.
The result was a major refocus around liver-targeted diseases, where the biology, delivery, and regulatory precedent offer the best chance of near-term success. “We know we can safely and effectively dose the liver—others have proven it,” Reine explained. “So we’re starting where the probability of both clinical and commercial success is highest.”
The company’s lead program is for Wilson’s disease, a rare genetic disorder of copper metabolism. “There’s an unmet need here—existing treatments are difficult, patients struggle with compliance, and life expectancy remains shortened,” he said. “What excites us is that prime editing is the only technology that can truly fix the transversion mutations behind this disease.” With an estimated 20,000+ treatable patients worldwide, the market is meaningful by rare disease standards—and potentially transformative for patients.
Following Wilson’s, Prime plans to move into alpha-1 antitrypsin deficiency (AATD) in 2025, leveraging shared delivery and manufacturing platforms to lower cost and accelerate development. “It’s faster and cheaper because it’s modular,” Reine said. “We can reuse the same lipid nanoparticle system and much of the toxicology data.”
 Bob Smith (left), Venture Partner, OrbiMed and Chairman, Alliance for Regenerative Medicine (ARM), and Allan Reine (right), MD, CEO, Prime Medicine, discuss how strategic funding and collaboration can accelerate gene editing technology development. [Jonathan D. Grinstein]The company also recently made a tough call to wind down its chronic granulomatous disease (CGD) program, despite strong early data. “It was an emotional decision,” Reine said. “We may have effectively cured two patients, but the market is simply too small to sustain a company of our size. We’re exploring regulatory paths to bring that data to patients without losing financial discipline.”
Bob Smith (left), Venture Partner, OrbiMed and Chairman, Alliance for Regenerative Medicine (ARM), and Allan Reine (right), MD, CEO, Prime Medicine, discuss how strategic funding and collaboration can accelerate gene editing technology development. [Jonathan D. Grinstein]The company also recently made a tough call to wind down its chronic granulomatous disease (CGD) program, despite strong early data. “It was an emotional decision,” Reine said. “We may have effectively cured two patients, but the market is simply too small to sustain a company of our size. We’re exploring regulatory paths to bring that data to patients without losing financial discipline.”
Prime continues to invest in cystic fibrosis, supported by the Cystic Fibrosis Foundation, and is exploring future opportunities in neurological disorders—though Reine says the company will wait until delivery technologies mature. “We’ll get there,” he said. “It’s not if, but when.”
Looking more broadly, Reine sees the gene-editing sector stabilizing after years of hype and volatility. “Five years ago, valuations were unsustainable. Then everything crashed—companies were trading below cash,” he said. “Now, sentiment is improving for the right reasons. We’re seeing real clinical data, real approvals, and pharma partnerships that validate the space. The dream is becoming reality.”
Reine believes Prime’s discipline—focusing on tractable, high-impact diseases—will keep it strong through the next wave of consolidation. “This sector is growing up,” he said. “It’s no longer about who has the flashiest platform, but who can turn groundbreaking science into real medicines. That’s the mission we’re executing on.”
No more excuses
During a panel discussing the monumental Baby KJ story that unfolded earlier this year, when it comes to making gene editing therapies a reality for patients with rare diseases, Fyodor Urnov, PhD, scientific director at UC Berkeley’s Innovative Genomics Institute (IGI), said, “There are no more excuses.” Not only has the field now demonstrated that developing an on-demand personalized gene editing therapeutic is possible, but Urnov believes that the Baby KJ story has led to a rare moment of alignment between science and regulation—one that could accelerate a new era of personalized CRISPR-based cures.
Later in the afternoon in a one-on-one conversation, Urnov, describing what he sees as a transformative shift in how the agency approaches gene-editing therapies, told Inside Precision Medicine, “We have to leverage the momentum of the FDA. Urnov recalled hearing senior officials speak with unprecedented enthusiasm—one declaring that “CRISPR gives the gift of life,” another assuring him, “We’re on your team; we just want to get out of your way.” Even the FDA’s biologics division, he noted, is exploring new approval pathways for ultra-small, bespoke trials that could bring lifesaving treatments to children with rare genetic diseases far more quickly than before.
That shift, Urnov argued, opens two powerful opportunities. The first lies with the biotech industry, where many companies have quietly shelved rare-disease programs because small patient populations made large pivotal trials financially unfeasible. With regulators signaling a willingness to rethink trial design, Urnov believes firms like Intellia, Editas, CRISPR Therapeutics, Beam, and Prime Medicine could “de-mothball” these programs and pursue accelerated routes to approval. “Anyone not taking advantage of this regulatory moment,” he warned, “will spend the rest of their lives kicking themselves.”
The second opportunity, he said, is to expand CRISPR-on-demand—customized editing therapies designed for individual patients—beyond the few centers currently pioneering the approach. Groups at St. Jude, Boston Children’s, and Seattle Children’s are well-positioned to join UCSF and the Innovative Genomics Institute in treating critically ill children. “We should aim for dozens of ‘Kyle Juniors’ across the country in the next few years,” Urnov said, referencing the now-famous child who became one of the first to receive an FDA-cleared personalized CRISPR therapy.
But the science can’t move without manufacturing support. Urnov called on contract manufacturers like Danaher, Synthego, Agilent, and BioNTech to “raise their flags” and enter the gene-editing supply chain. Scaling production of CRISPR-based medicines, he said, is just as vital as designing them.
Ultimately, Urnov emphasized, data—not theory—must lead the way. Urnov applauded the guts and planning that it took for Becca Ahrens-Nicklas, MD, PhD, and Kiran Musunuru, MD, PhD, to lead the teams at the Children’s Hospital of Philadelphia and the University of Pennsylvania to be the first to try. He pointed to the bravery of Victoria Gray, the first patient to receive a CRISPR cure for sickle cell disease. “Nobody knew if her cells would survive,” he said, “and they did.” The trial, run by Vertex, transformed uncertainty into evidence and set the benchmark for what gene editing can achieve.
For Urnov, the moral imperative is clear. “Children still die waiting for therapies we could already be testing,” Urnov said. “We can’t keep building safety assays for medicines they’ll never receive.” Urnov called on regulators, academics, and companies to share insights more freely—a call to end the “siloing of regulatory learning” that slows progress.
The science, he said, is ready. The question now is whether those in the cell and gene therapy field can move fast enough to match it.