Mirghani H, Amen F, Tao YG, et al. Increased radiosensitivity of HPV-positive head and neck cancers: molecular basis and therapeutic perspectives. Cancer Treat Rev. 2015;41(10):844–52.
Egawa N, Doorbar J. The low-risk papillomaviruses. Virus Res. 2017;231:119–27.
Dareng EO, Ma B, Famooto AO, et al. Prevalent high-risk HPV infection and vaginal microbiota in Nigerian women. Epidemiol Infect. 2016;144(1):123–37.
Wu M, Li HR, Yu HF, et al. Disturbances of Vaginal Microbiome Composition in Human Papillomavirus Infection and Cervical Carcinogenesis: A Qualitative Systematic Review. Front Oncol. 2022;12: e941741.
Xu X, Rao H, Fan X, et al. HPV-related cervical diseases: alteration of vaginal microbiotas and promising potential for diagnosis. J Med Virol. 2023;95(1): e28351.
Castanheira CP, Sallas ML, Nunes RAL, et al. Microbiome and cervical cancer. Pathobiology. 2021;88(2):187–97.
Li YP, Cao L, Han X, et al. Altered vaginal eukaryotic virome is associated with different cervical disease status. Virol Sin. 2023;38(2):184–97.
Younes JA, Lievens E, Hummelen R, et al. Women and their microbes: the unexpected friendship. Trends Microbiol. 2018;26(1):16–32.
Lee JE, Lee SH, Lee HT, et al. Association of the vaginal microbiota with human papillomavirus infection in a Korean twin cohort. PLoS One. 2013;8(5): e63514.
Cheng WY, Xu F, Gao LL, et al. The correlation between the determination of vaginal micro-ecological composition and the outcome of HPV infection by high-throughput metagene sequencing information technology on the Illumina platform. J Infect Public Health. 2020;13(12):1961–6.
Liu S, Li Y, Song Y, et al. The diversity of vaginal microbiome in women infected with single HPV and multiple genotype HPV infections in China. Front Cell Infect Microbiol. 2022;12: e642074.
Norenhag J, Du J, Olovsson M, et al. The vaginal microbiota, human papillomavirus and cervical dysplasia: a systematic review and network meta-analysis. BJOG. 2019;127(2):171–80.
Zhang Z, Ma Q, Zhang L, et al. Human papillomavirus and cervical cancer in the microbial world: exploring the vaginal microecology. Front Cell Infect Microbiol. 2024;14: e1325500.
Ravel J, Gajer P, Abdo Z, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A. 2010;108:4680–7.
Di Paola M, Sani C, Clemente AM, et al. Characterization of Cervico-Vaginal Microbiota in Women Developing Persistent High-Risk Human Papillomavirus Infection. Scientific Reports. 2017;7. Article No. 10200.
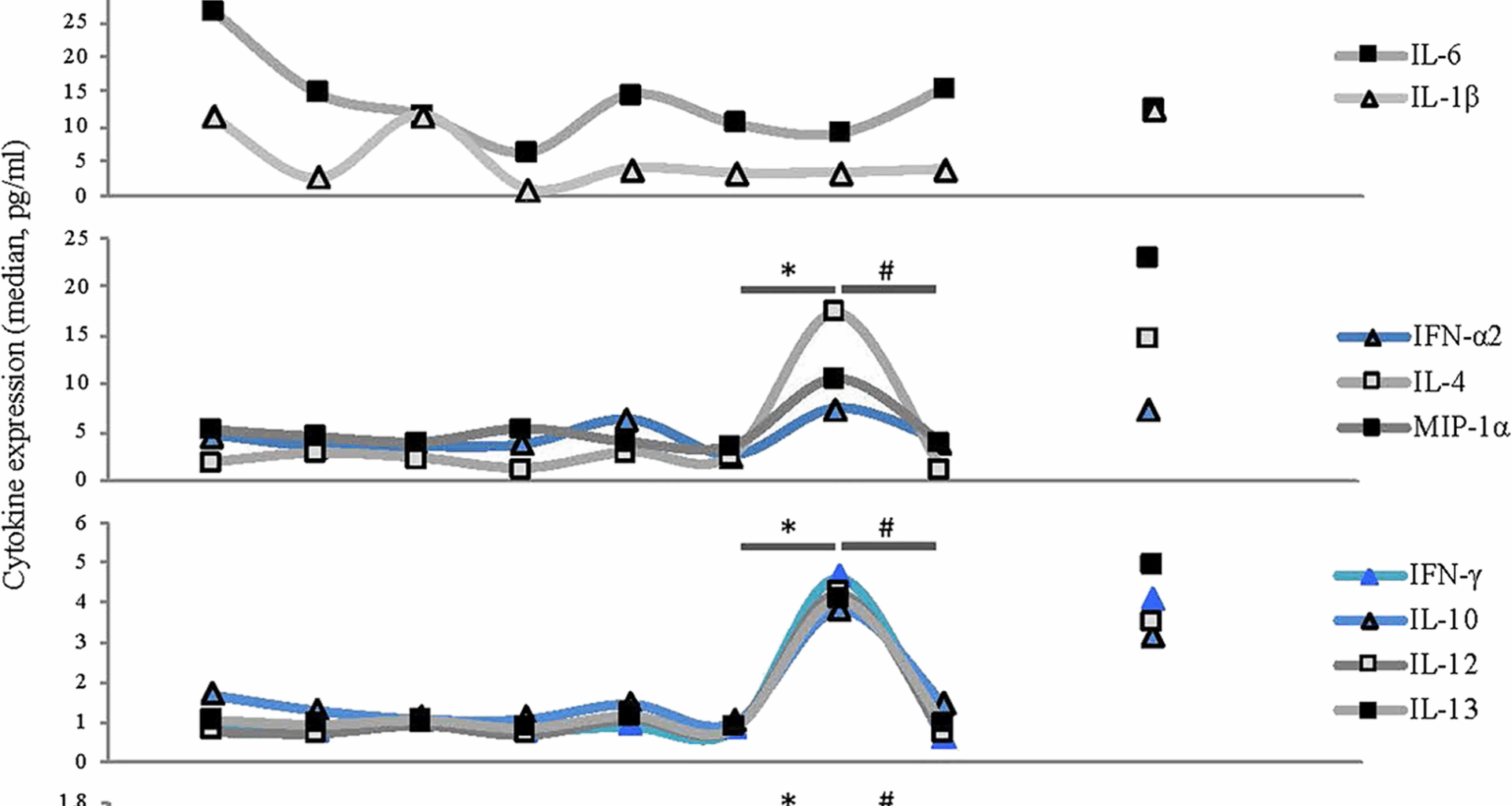
Moscicki AB, Shi B, Huang H, et al. Cervical-Vaginal Microbiome and Associated Cytokine Profiles in a Prospective Study of HPV 16 Acquisition, Persistence, and Clearance. Front Cell Infect Microbiol. 2020;10: e569022.
Łaniewski P, Barnes D, Goulder A, et al. Linking cervicovaginal immune signatures, HPV, and microbiota composition in cervical carcinogenesis in non-Hispanic and Hispanic women. Sci Rep. 2018;8(1):e00064-e122.
Li C, Zhang Z, Yang Y, et al. Changes in the cervicovaginal microbiota composition of HPV16-infected patients after clinical treatment. Cancer Med. 2022;11(24):5037–49.
Fan Q J, Wu Y H, Li M C, et al. Lactobacillus spp. Create a protective micro-ecological environment through regulating the core fucosylation of vaginal epithelial cells against cervical cancer. Cell Death & Disease, 2021, 12(12): e1094.
Wang YY, Thakur R, Shen QL, et al. Influences of vaginal microbiota on human papillomavirus infection and host immune regulation: What we have learned? Decoding Infection and Transmission. 2023;1: e100002.
Frąszczak K, Barczyński B, Kondracka A. Does Lactobacillus exert a protective effect on the development of cervical and endometrial cancer in women? Cancers (Basel). 2022;14(19): e4909.
Dong MT, Dong YL, Bai JY, et al. Interactions between microbiota and cervical epithelial, immune, and mucus barrier. Front Cell Infect Microbiol. 2023;13: e1124591.
Gao Q, Fan T, Luo SY, et al. Lactobacillus gasseri LGV03 isolated from the cervico-vagina of HPV-cleared women modulates epithelial innate immune responses and suppresses the growth of HPV-positive human cervical cancer cells. Translational Oncology. 2023;35: e101714.
Nicolò S, Tanturli M, Mattiuz G, et al. Vaginal lactobacilli and vaginal dysbiosis-associated bacteria differently affect cervical epithelial and immune homeostasis and anti-viral defenses. Int J Mol Sci. 2021;22(12): e6487.
Chen R, Peng C, Wang Z, et al. Effects of vaginal microbiota on human papillomavirus infection and its related diseases. Microb Pathog. 2024;193: e106761.
Lin WY, Zhang QY, Chen YJ, et al. Changes of the vaginal microbiota in HPV infection and cervical intraepithelial neoplasia: a cross-sectional analysis. Sci Rep. 2022;12(1): e2812.
Bai B, Tuerxun G, Tuerdi A, et al. Analysis of vaginal flora diversity and study on the role of Porphyromonas asaccharolytica in promoting IL-1β in regulating cervical cancer. Sci Rep. 2024;14(1): e21731.
Yang CY, Chang TC, Lee YT, et al. Exploring the interplay between cervicovaginal microbiome, HPV infection, and cervical intraepithelial neoplasia in Taiwanese women. J Med Virol. 2025;97(2): e70190.
Tam K, Torres V J, Fischetti V A, et al. Staphylococcus aureus Secreted Toxins and Extracellular Enzymes. Microbiology Spectrum. 2019;7(2): 10.1128.
Britto AMA, Siqueira JD, Curty G, et al. Microbiome analysis of Brazilian women cervix reveals specific bacterial abundance correlation to RIG-like receptor gene expression. Front Immunol. 2023;14: e1147950.
Reimers LL, Mehta SD, Massad LS, et al. The cervicovaginal microbiota and its associations with human papillomavirus detection in HIV-infected and HIV-uninfected women. J Infect Dis. 2016;214(9):1361–9.
Chávez-Torres M, Gómez-Palacio-Schjetnan M, Reyes-Terán G, et al. The vaginal microbiota of women living with HIV on suppressive antiretroviral therapy and its relation to high-risk human papillomavirus infection. BMC Microbiol. 2023;23(1): e21.
Ntuli L, Mtshali A, Mzobe G, et al. Role of Immunity and Vaginal Microbiome in Clearance and Persistence of Human Papillomavirus Infection[J]. Front Cell Infect Microbiol. 2022;12: e927131.
Zhang W, Yin Y, Jiang Y, et al. Relationship between vaginal and oral microbiome in patients of human papillomavirus (HPV) infection and cervical cancer. J Transl Med. 2024;22(1): e396.
Lebeau A, Bruyere D, Roncarati P, et al. HPV infection alters vaginal microbiome through down-regulating host mucosal innate peptides used by Lactobacilli as amino acid sources. Nat Commun. 2022;13(1): e1076.
Verhoeven V, Renard N, Makar A, et al. Probiotics enhance the clearance of human papillomavirus-related cervical lesions. Eur J Cancer Prev. 2013;22(1):46–51.
Palma E, Recine N, Domenici L, et al. Long-term Lactobacillus rhamnosus BMX 54 application to restore a balanced vaginal ecosystem: a promising solution against HPV-infection. BMC Infect Dis. 2018;18(1): e13.
Liu Y, Zhao X, Wu F, et al. Effectiveness of vaginal probiotics Lactobacillus crispatus chen-01 in women with high-risk HPV infection: a prospective controlled pilot study. Aging (Albany NY). 2024;16(14):11446–59.
He N, Song L, Lu ZX, et al. Clinical efficacy analysis of the Chinese medicine Paiteling applied to human papillomavirus infection: a retrospective study. PLoS One. 2024;19(12): e0315376.
Li X, Ning L, Zhao HT, et al. Jiawei Ermiao Granules (JWEMGs) clear persistent HR-HPV infection though improving vaginal microecology. J Ethnopharmacol. 2025;341: e119342.
Smith JA, Gaikwad AA, Mathew L, et al. AHCC® Supplementation to Support Immune Function to Clear Persistent Human Papillomavirus Infections. Front Oncol. 2022;12: e881902.
Supriya Y, Sivamalar S, Nallusamy D, et al. Application of probiotics in cervical cancer infections to enhance the immune response. Microb Pathog. 2024;193: e106764.
Baarlen PV, Troost F, Meer CVD, et al. Human mucosal in vivo transcriptome responses to three lactobacilli indicate how probiotics may modulate human cellular pathways. Proc Natl Acad Sci U S A. 2010;108:4562–9.
Kahouli L, Tomaro-Duchesneau C, Prakash S. Probiotics in colorectal cancer (CRC) with emphasis on mechanisms of action and current perspectives. J Med Microbiol. 2013;62(8):1107–23.
Yang Q, Wang YP, Wei XY, et al. The Alterations of Vaginal Microbiome in HPV16 Infection as Identified by Shotgun Metagenomic Sequencing. Front Cell Infect Microbiol. 2020;10: e00286.