DM is a frequently used over-the-counter cough suppressant that is available as a single-entity product or in multiple-ingredient formulations. Allergic reactions have been reported following the ingestion of DM [6,7,8].
To date, there have been three reports of anaphylaxis after the ingestion of a DM-containing compound. The first reaction was described in a 40-year-old female who experienced the immediate onset of hives, lip swelling, and shortness of breath following the ingestion of a combination cough and cold preparations that contained DM. The patient declined skin testing and underwent a two-step graded oral challenge to DM where she developed hives, nasal and conjunctival congestion following the full dose. Importantly, this patient later tolerated hydrocodone and codeine [6]. The second report describes a 24-year-old female who developed anaphylaxis immediately following ingestion of Romilar® (dextromethorphan hydrobromide). She was positive on skin prick testing to Romilar®, as were 3 of 10 control subjects. She went on to receive an oral challenge to DM syrup and developed generalized erythema, pruritus and hypotension, requiring epinephrine. This patient subsequently tolerated codeine and tramadol [7].
The third report details a case of a 14-year-old female who experienced anaphylaxis following exposure to DM. Although skin prick testing and the Basophil Activation Test (BAT) were negative, the patient developed generalized erythema and hives during drug provocation testing with DM [8].
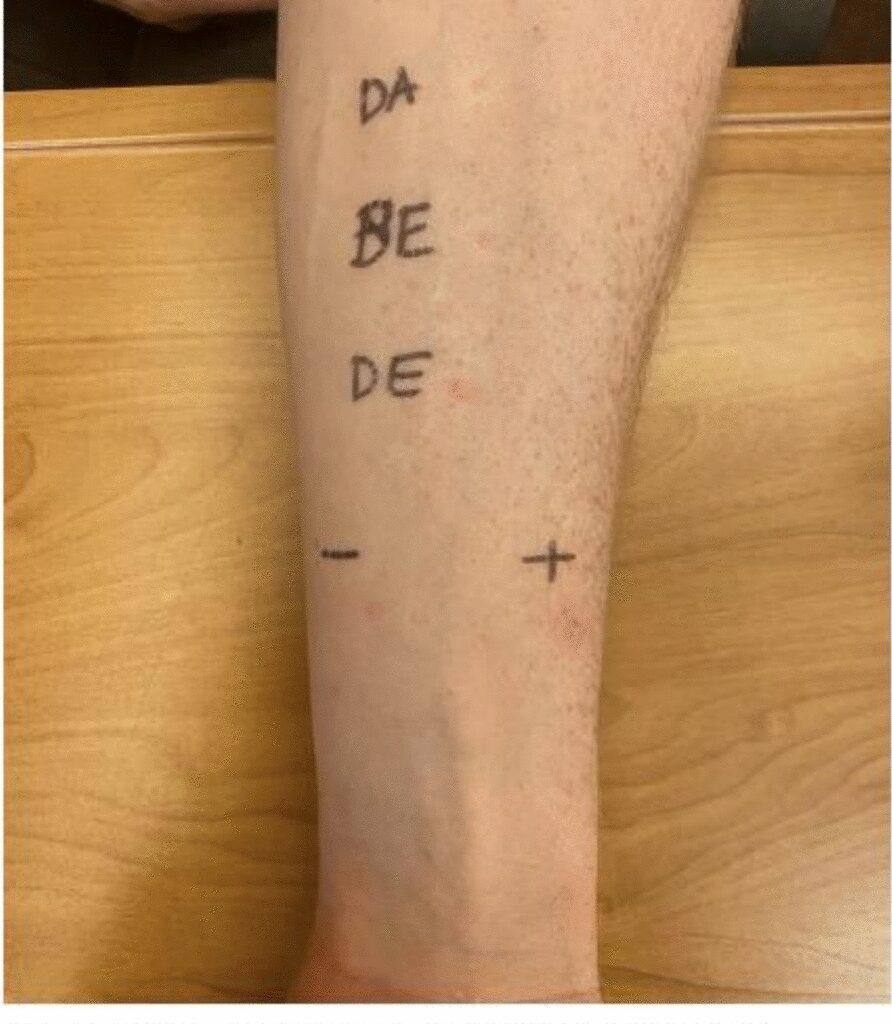
At our clinic, we initially performed skin prick testing to several drugs as our patient reported ingestion of multi-ingredient products prior to his reactions, making identification of the culprit agent challenging. Owing to inconsistent skin prick testing results, the test was repeated three times. DM was positive in both the first and third testing attempts. This variation in skin prick results may be related to the difference in the number of mast cells present at a body site even within the same limb [10].
Skin prick testing with DM at full concentration was performed on two healthy individuals. Both tests were negative, with no immediate hypersensitivity reactions observed.
We expected that our patient would have a positive skin test to the formulation of Benylin® that contains DM, but his testing result was indeterminate, which could be due to the low concentration of the culprit allergen in the mixture, resulting in a weakly positive reaction on skin testing.
Our case has several diagnostic limitations. The exact brand of Vicks DayQuil Complete® was unavailable. Hypersensitivity to excipients or dyes was considered but could not be tested due to lack of isolated forms. However, the patient had previously tolerated other medications with the same ingredients, such as those in Vicks DayQuil and Tylenol. Basophil activation testing was not pursued due to lack of a validated assay for DM [8] and drug provocation was avoided given the severity of the initial reaction. Skin prick testing was performed using undiluted formulations, which may carry a risk of irritant responses.
Anaphylaxis may result from classical IgE-mediated mechanisms or through non-IgE pathways such as direct mast cell activation [11]. One such pathway involves activation of the MRGPRX2 receptor, a G protein–coupled receptor expressed on mast cells. MRGPRX2-mediated activation has been implicated in hypersensitivity reactions to several small-molecule drugs, including opioids such as morphine, codeine and DM [12].
While clinical features of MRGPRX2-mediated reactions can mimic IgE-mediated anaphylaxis, certain features may favor the former—such as reactions occurring on first exposure, the need for higher doses to trigger symptoms, and shorter symptom duration [13].
The diagnostic distinction can be difficult, as both pathways may produce similar clinical presentations. Additionally, positive responses on skin testing can occur due to direct mast cell activation, complicating interpretation. As such, the positive skin test to DM observed in our patient does not definitively indicate an IgE-mediated mechanism, and alternative pathways, including MRGPRX2 involvement, should be considered in the differential diagnosis.
A recently published pediatric report of DM-induced anaphylaxis, confirmed by drug provocation despite negative skin prick and BAT results, further underscores the potential involvement of non-IgE mechanisms and the diagnostic limitations of current testing methods [8]. These observations highlight the need for greater awareness and further research into the clinical implications of MRGPRX2-mediated hypersensitivity.
Although DM is structurally related to phenanthrene opioids, cross-reactivity has not been clearly demonstrated [7, 14]. Therefore, the patient was advised to avoid DM specifically, rather than all chemically related opioids. However, as DM is structurally related to pholcodine, a cough medication used in Europe for many years that was implicated in perioperative anaphylaxis through cross-sensitization with neuromuscular blocking agents, the potential for cross-reactivity within this chemical class cannot be excluded [15].
Skin testing to phenanthrene opioids like morphine and codeine is not performed due to the irritant effect of these agents and the high risk of false positive results [16]. Nor did we offer challenge doses to these drugs, although such evaluation may have provided additional insight into potential cross-allergenicity. This represents a limitation of our study and highlights the need for further investigation into immunologic cross-reactivity among structurally related compounds.