In what experts are calling a “dream come true,” scientists used a recent biochemical discovery to help an 8-year-old boy with a rare genetic condition regain mobility.
Researchers from NYU Langone demonstrated, in a study published in Nature on Wednesday, how a chemical precursor to a commonly available enzyme, CoQ10, can help brain cells overcome a rare genetic condition that severely hobbles cells’ energy production process. Without treatment, the boy’s condition is known to deteriorate rapidly and could be fatal.
“That is basic science translating into clinical medicine, a dream come true,” Navdeep Chandel, a professor of medicine at Northwestern University, told STAT. He was not involved in the study.
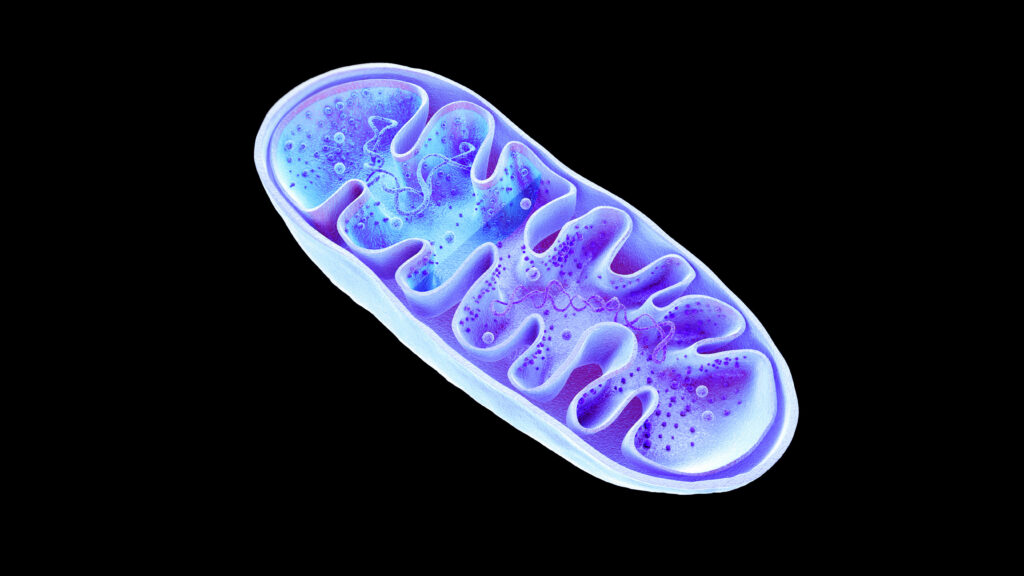
This study revolves around science’s understanding of how cells produce energy — a task performed by the so-called powerhouse of the cell, the mitochondria. To make energy, the mitochondria needs coenzyme Q10 (CoQ10). A rare genetic deficiency could interfere with body’s ability to make the enzyme, causing HPDL deficiency — a fatal condition characterized by spastic movements, neurodevelopmental delays, and even paralysis.
HPDL deficiency can be hereditary — when a child inherits two copies of the mutated HPDL gene, one from each parent. This progressive childhood-onset movement disorder has multiple variants that can result in different ages of onset, clinical presentations, and survival. Children with the most severe clinical presentations of this disease die at a median age of 18 months. In the case of the boy that NYU Langone neurologists treated, he did not have the onset of symptoms until later into his childhood, despite having inherited the mutated HPDL gene.

New study challenges understanding of how age, chronic diseases and inflammation are linked
For years, physicians have been trying to treat such conditions in which mitochondrial function is reduced by supplementing the body with CoQ10 enzyme. Found on most pharmacy shelves, CoQ10 is a wellness supplement that can help with heart health, energy, and brain health, though the Food and Drug Administration has not approved CoQ10 for treating any medical condition.
“It’s safe. It’s reasonably effective at treating symptoms outside of the brain, but almost completely ineffective at treating symptoms within the brain, because it doesn’t get through the blood-brain barrier,” said Michael Pacold, an associate professor of radiation oncology at NYU Langone and one of the study authors.
Think of the blood-brain barrier as the brain’s plastic wrap — keeping harmful chemicals out. But it’s almost too good because many drugs cannot penetrate it. That’s where Pacold’s lab’s earlier discovery helped. In a 2021 study, it discovered one of the first steps to how the cell makes CoQ10. This involves the HPDL gene and its role in making 4-HB — an essential building block cells need to make CoQ10.
Pacold and his team found that 4-HB, the precursor to CoQ10, could not only cross the blood-brain barrier and reach the brain, but it was able to restore standing and walking function in mice that had HPDL gene deficiency.
“Instead of giving CoQ10, we figured, why not give the cell the building blocks, so that the cell can make it itself?” Pacold told STAT.
The boy, who received the treatment, had normal development until August 2023, when he started displaying uncontrollable spastic movements in both of his ankles while playing soccer.
“Our son’s condition changed dramatically in a short period. He went from being the fastest runner in his class and an avid soccer player to struggling just to walk, often limping and experiencing frequent falls,” the boy’s parents said in an emailed response to questions from STAT. The family did not want the boy’s or their name used.
By November 2023, he could not stand on his own and needed a wheelchair. The family, who had lost two other children to the same genetic condition, contacted a physician who specializes in HPDL deficiency, and was connected with doctors and researchers at NYU.
Claire Miller, a pediatric neurologist at NYU Langone, and a team of neurologists met with Pacold to explore the possibility of administering the experimental treatment to the boy. Miller, also an author on the study, said the research data from Pacold’s team was “very convincing.” Researchers then got formal approval from the FDA on compassionate use grounds.

New blood test could predict preeclampsia in the first trimester
Still, it was an experimental treatment that had only ever been tested in mice, and the family knew it could involve unknown risks. “It was one of the hardest decisions we’ve ever made, but doing nothing felt riskier,” the boy’s parents said. “We saw how quickly our son was declining and knew we had to act. After speaking with doctors and doing our research, we got hope and confidence to step into the unknown.”
Nineteen days after the family met with the team of neurologists and scientists, the boy received his first treatment — 4HB dissolved in water and taken orally. He has been tolerating the treatment well for over a year. He has enjoyed long walks, hikes, and even celebrated two birthdays, according to the researchers.
To Miller, who specializes in treating children with movement disorders, the boy’s recovery meant more than how effective the treatment was. “Movement is identity and personality,” she told STAT. “The beautiful thing about movement is that’s how we express our identities and our personalities.”
For researchers, this study is a breakthrough in the so-called bench-to-bedside pipeline — taking a basic biochemical discovery and translating it to a promising treatment for a rare and fatal childhood disease. “We all dream of this as scientists. And every morning I pinch myself … is this really a dream?” said Pacold.
Chandel, the Northwestern professor, pointed to how the fundamental discovery was made using a grant from the National Institute of Health.
“Now more than ever, when the NIH is thinking about cutting and slashing … here’s somebody who took a very basic biochemical approach, and they found the enzyme, and they found what the enzyme does, and they gave that enzyme to people who had genetic mutations. And it made a difference,” said Chandel.

DeepMind launches AlphaGenome, aiming to predict gene regulation from DNA sequence
Even as the researchers remain hopeful, they are cautious that this study reflects the story of just one individual with an HPDL deficiency. There is still much to be discovered when it comes to the onset of this rare HPDL deficiency and the crucial window of symptom development of this disorder during infancy.
“It takes both the discovery, yes, and people who are willing to take the risk,” said Pacold, who along with his team are already working up a larger clinical trial to encompass other HPDL variants, children across a wider age range, and fleshing out the best treatment regimen for 4-HB.
After the first month on the treatment, “a very happy child came into the lab and said, ‘When are you going to get this into a pill form, so it’s easier to take?’” said Pacold, “He’d apparently gone for over a 1-kilometer walk in Central Park the day before that.”