Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Herr I, Buchler MW. Dietary constituents of broccoli and other cruciferous vegetables: implications for prevention and therapy of cancer. Cancer Treat Rev. 2010;36:377–83.
Willett WC. Diet and cancer: One view at the start of the millennium. Cancer Epidem Biomar. 2001;10:3–8.
Murillo G, Mehta RG. Cruciferous vegetables and cancer prevention. Nutr Cancer. 2001;41(1–2):17–28.
Higdon JV, Delage B, Williams DE, Dashwood RH. Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. Pharmacol Res. 2007;55:224–36.
Zhang Y, Yao S, Li J. Vegetable-derived isothiocyanates: antiproliferative activity and mechanism of action. Proc Nutr Soc. 2006;65:68–75.
Tse G, Eslick GD. Cruciferous vegetables and risk of colorectal neoplasms: a systematic review and meta-analysis. Nutr Cancer. 2014;66(1):128–39.
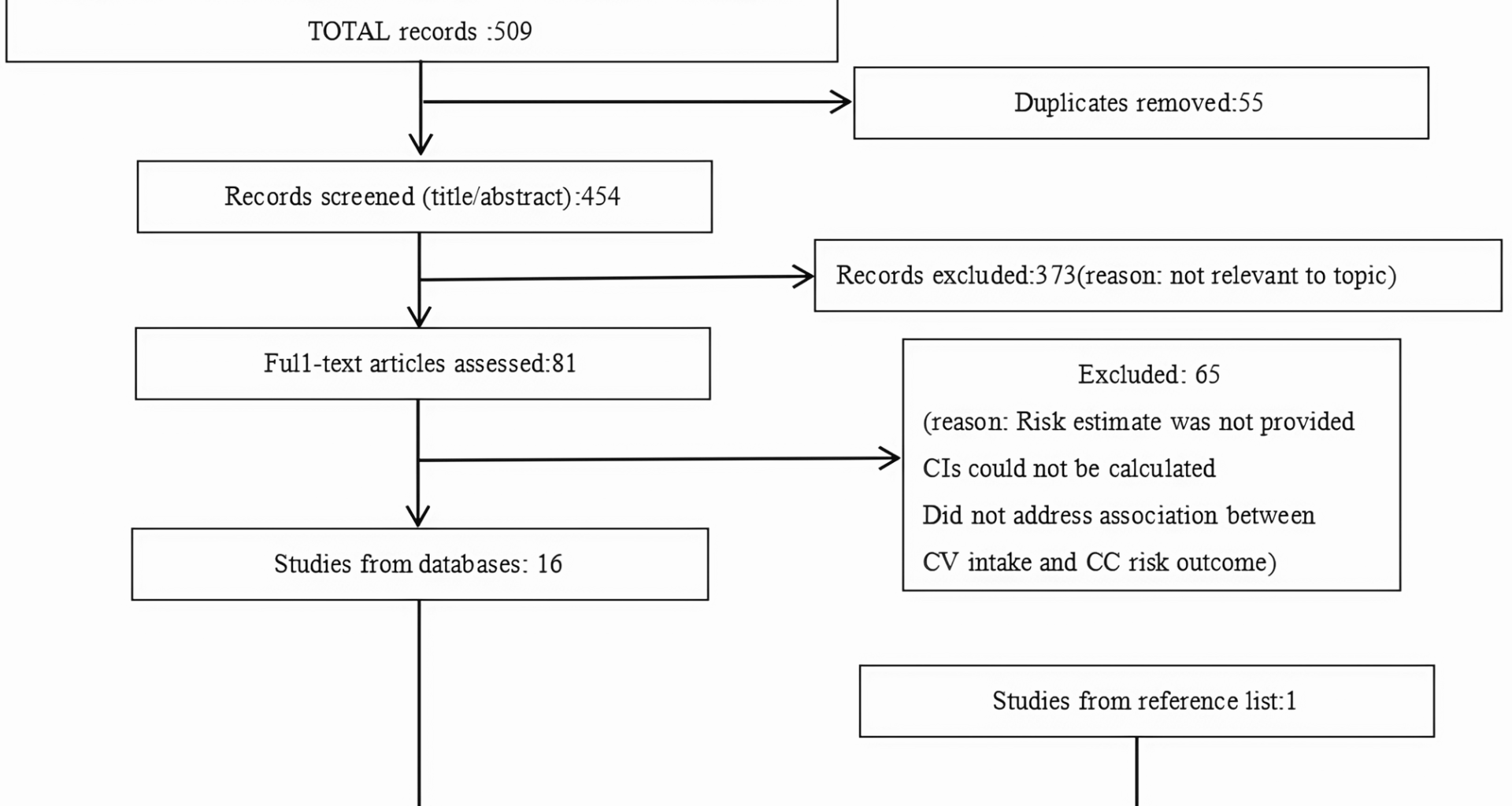
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89. https://doi.org/10.1016/j.jclinepi.2021.03.001.
Stang A. Critical evaluation of the Newcastle Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ. 1997;315(7121):1533–7.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med. 2009;29(12):1282–97.
Chen H, Manning AK, Dupuis J. A method of moments estimator for random effect multivariate meta-analysis. Biometrics. 2012;68(4):1278–84.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemp Clin Trials. 2015;45(Pt A):130–8. https://doi.org/10.1016/j.cct.2015.05.009.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Orsini N, Li R, Wolk A, et al. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73.
Harrell FE Jr, Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. 1988;80:1198–202.
Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med. 2010;29:1282–97.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH, Tetzlaff J, Deeks JJ, Peters J, Macaskill P, Schwarzer G, Duval S, Altman DG, Moher D, Higgins JP. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;22(343): d4002. https://doi.org/10.1136/bmj.d4002.
Leenders M, Siersema PD, Overvad K, Tjønneland A, Olsen A, Boutron-Ruault MC, Bastide N, Fagherazzi G, Katzke V, Kühn T, Boeing H, Aleksandrova K, Trichopoulou A, Lagiou P, Klinaki E, Masala G, Grioni S, Santucci De Magistris M, Tumino R, Ricceri F, Peeters PH, Lund E, Skeie G, Weiderpass E, Quirós JR, Agudo A, Sánchez MJ, Dorronsoro M, Navarro C, Ardanaz E, Ohlsson B, Jirström K, Van Guelpen B, Wennberg M, Khaw KT, Wareham N, Key TJ, Romieu I, Huybrechts I, Cross AJ, Murphy N, Riboli E, Bueno-de-Mesquita HB. Subtypes of fruit and vegetables, variety in consumption and risk of colon and rectal cancer in the European prospective investigation into cancer and nutrition. Int J Cancer. 2015;137(11):2705–14. https://doi.org/10.1002/ijc.29640.
Vogtmann E, Xiang YB, Li HL, Cai Q, Wu QJ, Xie L, Li GL, Yang G, Waterbor JW, Levitan EB, Zhang B, Zheng W, Shu XO. Cruciferous vegetables, glutathione S-transferase polymorphisms, and the risk of colorectal cancer among Chinese men. Ann Epidemiol. 2014;24(1):44–9. https://doi.org/10.1016/j.annepidem.2013.10.003.
Mori N, Sawada N, Shimazu T, Yamaji T, Goto A, Takachi R, Ishihara J, Iwasaki M, Inoue M, Tsugane S and JPHC Study Group. Cruciferous vegetable intake and colorectal cancer risk: Japan public health center-based prospective study. Eur J Cancer Prev. 2019;28(5):420–7. https://doi.org/10.1097/CEJ.0000000000000491.
Flood A, Velie EM, Chaterjee N, Subar AF, Thompson FE, Lacey JV Jr, Schairer C, Troisi R, Schatzkin A. Fruit and vegetable intakes and the risk of colorectal cancer in the breast cancer detection demonstration project follow-up cohort. Am J Clin Nutr. 2002;75(5):936–43. https://doi.org/10.1093/ajcn/75.5.936.
Steinmetz KA, Potter JD. Food-group consumption and colon cancer in the adelaide case-control study. I. Vegetables and fruit. Int J Cancer. 1993;53(5):711–9.
Voorrips LE, Goldbohm RA, van Poppel G, Sturmans F, Hermus RJ, van den Brandt PA. Vegetable and fruit consumption and risks of colon and rectal cancer in a prospective cohort study: The Netherlands cohort study on diet and cancer. Am J Epidemiol. 2000;152(11):1081–92.
Michels KB, Edward Giovannucci, Joshipura KJ, Rosner BA, Stampfer MJ, Fuchs CS, Colditz GA, Speizer FE, Willett WC. Prospective study of fruit and vegetable consumption and incidence of colon and rectal cancers. J Natl Cancer Inst. 2000;92(21):1740–52. https://doi.org/10.1093/jnci/92.21.1740. Erratum in: J Natl Cancer Inst 2001;93(11):879.
Peters RK, Pike MC, Garabrant D, Mack TM. Diet and colon cancer in Los Angeles county. California Cancer Causes Control. 1992;3(5):457–73.
Hara M, Hanaoka T, Kobayashi M, Otani T, Adachi HY, Montani A, Natsukawa S, Shaura K, Koizumi Y, Kasuga Y, Matsuzawa T, Ikekawa T, Sasaki S, Tsugane S. Cruciferous vegetables, mushrooms, and gastrointestinal cancer risks in a multicenter, hospital-based case-control study in Japan. Nutr Cancer. 2003;46(2):138–47. https://doi.org/10.1207/S15327914NC4602_06.
Hu J, Mery L, Desmeules M, Macleod M and Canadian Cancer Registries Epidemiology Research Group. Diet and vitamin or mineral supplementation and risk of rectal cancer in Canada. Acta Oncol. 2007;46(3):342–54.
Fang W, Qu X, Shi J, Li H, Guo X, Wu X, Liu Y, Li Z. Cruciferous vegetables and colorectal cancer risk: a hospital-based matched case-control study in Northeast China. Eur J Clin Nutr. 2019;73(3):450–7. https://doi.org/10.1038/s41430-018-0341-5.
Lee HP, Gourley L, Duffy SW, Estève J, Lee J, Day NE. Colorectal cancer and diet in an Asian population–a case-control study among Singapore Chinese. Int J Cancer. 1989;43(6):1007–16.
Young TB, Wolf DA. Case-control study of proximal and distal colon cancer and diet in Wisconsin. Int J Cancer. 1988;42(2):167–75.
Steinmetz KA, Kushi LH, Bostick RM, Folsom AR, Potter JD. Vegetables, fruit, and colon cancer in the Iowa Women’s Health Study. Am J Epidemiol. 1994;139(1):1–15.
Ramadas A, Kandiah M. Food intake and colorectal adenomas: a case-control study in Malaysia. Asian Pac J Cancer Prev. 2009;10(5):925–32.
West DW, Slattery ML, Robison LM, Schuman KL, Ford MH, Mahoney AW, Lyon JL, Sorensen AW. Dietary intake and colon cancer: sex- and anatomic site-specific associations. Am J Epidemiol. 1989;130(5):883–94. https://doi.org/10.1093/oxfordjournals.aje.a115421.
Chiu BC, Ji BT, Dai Q, Gridley G, McLaughlin JK, Gao YT, Fraumeni JF Jr, Chow WH. Dietary factors and risk of colon cancer in Shanghai, China. Cancer Epidemiol Biomarkers Prev. 2003;12(3):201–8.
Lee S, Meyerhardt JA. Impact of diet and exercise on colorectal cancer. Hematol Oncol Clin North Am. 2022;36:471–89.
Slattery ML, Boucher KM, Caan BJ, Potter JD, Ma KN. Eating patterns and risk of colon cancer. Am J Epidemiol. 1998;148:4–16.
Khayami R, Goltzman D, Rabbani SA, Kerachian MA. Epigenomic effects of vitamin D in colorectal cancer. Epigenomics. 2022;14:1213–28.
Duffy MJ, Mullooly M, Bennett K, Crown J. Vitamin D supplementation: Does it have a preventative or therapeutic role in cancer? Nutr Cancer. 2023;75:450–60.
Van BEL, Fuchs CS, Niedzwiecki D, Zhang S, Saltz LB, Mayer RJ, Mowat RB, Whittom R, Hantel A, Benson A, Atienza D, Messino M, Kindler H, Venook A, Ogino S, Giovannucci EL, Meyerhardt JA. Association of survival with adherence to the American cancer society nutrition and physical activity guidelines for cancer survivors after colon cancer diagnosis: the CALGB 89803/alliance trial. JAMA Oncol. 2018;4:783–90.
Fenwick GR, Heaney RK, Mullin WJ, VanEt-ten CH. Glucosinolates and their breakdown products in food and food plants. Crit Rev Food Sci Nutr. 1983;18(2):123–201.
Brooks JD, Paton VG, Vidanes G. Potent induction of phase 2 enzymes in human prostate cells by sulforaphane. Cancer Epidem Biomar. 2001;10(9):949–54.
Meeran SM, Ahmed A, Tollefsbol TO. Epigenetic targets of bioactive dietary components for cancer prevention and therapy. Clin Epigenetics. 2010;1(3–4):101–16. https://doi.org/10.1007/s13148-010-0011-5.PMID:21258631;PMCID:PMC3024548.
Chen Y, Tang L, Ye X, Chen Y, Shan E, Han H, Zhong C. Regulation of ZO-1 on β-catenin mediates sulforaphane suppressed colorectal cancer stem cell properties in colorectal cancer. Food Funct. 2022;13(23):12363–70. https://doi.org/10.1039/d2fo02932d.