In this real-world large data-base retrospective cohort study of more than 6 million people worldwide was the first one to described the patient infected with SARS-CoV-2 virus have higher incidence of neurologic complication with ATM. Those correlations were observed as early as within three months after infection, but no differences between gender or age. In addition, Alpha strained virus dominant period 2020/1/1 ~ 2021/6/30 has been noticed with higher association with ATM. Finally, no statistical significance between patients with and without SARS-CoV-2 infection after received different SARS-CoV-2 Vaccines.
According to Paterson et al. the probable mechanisms causing ATM and the various neurological syndromes associated with SARS-CoV-2 were either individually or in combination, direct viral neuronal injury and the host’s secondary hyperinflammation syndrome [10, 11, 12]. Blackburn and Wang et al. also indicated post-infectious neurological disorders may arise through several mechanisms: molecular mimicry, epitope spreading, bystander activation, and polyclonal B-cell activation [13, 14, 15]. The most relative one, molecular mimicry occurs when microorganisms possess epitopes that closely resemble the host’s antigens. As a result, lymphocytes activated by the infection may mistakenly target self-antigens. And the second most related one, autoreactive lymphocytes may be activated during the inflammatory cascade resulting in autoimmune response to highly virulent pathogen by “bystander activation”. In subsequent molecular level, SARS-CoV-2 enables interleukin-1 (IL-1), IL-2, IL-6 and interferon release or synthesis, affect the innate and acquired immunity result by inflammation and immune system suppression [16, 17]. These immune factors may lead to the so-called “cytokine storm syndrome” that trigger coagulopathy and thrombosis, and immune-mediated neurologic disorders like Guillain-Barré syndrome (GBS), acute disseminated encephalomyelitis (ADEM) and ATM [13, 14, 15]. The other possible mechanism for myelitis in the context of SARS-CoV-2 infection is the direct invasion of and replication in spinal cord neurons by the virus itself [18]. The presence of angiotensin-converting enzyme 2, SARS-CoV-2’s primary entry receptor, on membranes of spinal cord neurons further renders this possible [19].
By the fact of timing correlation could be another way to demonstrate its pathogenesis. In a clinical case series study of 43 patients, most cases (68%) had latency periods ranged from 10 days to 6 weeks, and the remaining 32% (11/34 cases) the latency period ranged from hours to 5 days. The shorter latency period may indicate a direct neurotropic effect of SARS-CoV- 2 during the initial infection causing para-infectious myelitis. Longer latency periods may indicate a post-infectious neurological complication resulting from the host response to the virus. No particular geographic origin, distribution by sex or age group, nor clinical picture were associated with shorter or longer latency periods [5]. The other systemic cases reviews showed the latency of on average 11 days from the onset of the first COVID-19 symptoms to the first signs of myelitis from 20 patients. Affected individuals were of all different ages and ancestries and had a slight predominance for males with median age 56, unlikely with other CNS autoimmune disorder predominantly female and much younger [7]. Our study showed similar results as increasing incidence of ATM within three months after SARS-Cov-2 infection, and even had longer follow up time up to one year period. Even though no clear definition of timeframe about para- or postinfection, SARS-Cov-2 could be the driver of ATM with most likely mechanism as immune-mediated response.
Another aspect of SARS-Cov-2 infection related to ATM would be incidence rate during and before pandemic. In a prospective study of 4,491 patients with COVID-19 hospitalized conducted in New York revealed no ATM, meningitis or cephalitis identified caused by inadequate patient number [6]. According to previous literature, ATM has been reported from 1 to 32 per one million population per year, if including later diagnosed autoimmune disorder [1, 20]. However, our result showed both increasing incidence rate in Covid and non-COVID group with 97 and 65 per one million population, despite of Covid cases still had significant higher incidence than second. Another large population-base vaccine registry study revealed 40 cases per one million of ATM, encephalitis and meningitis in 56 days observation period. The incidence was based on the population of vaccinated people, 2,005,280 (~ 6%) had a SARS-CoV-2-positive test. Of those with a positive test, 1,838,628 (~ 91%) had their SARS-CoV-2 test prior to vaccination [21]. The phenomenon of increased ATM incidence was observed from above and our study, and it could be probable related to hidden SARS-Cov-2 Infection among general population. Even though non-COVID-19 group laboratory data was confirmed by negative lab tests, the time correlation between ICD-10 Coding and laboratory confirmation was not clear.
Regarding to vaccine issue, National board in United Kingdom has received reports like 22 cases of myelitis following the Pfizer-BioNtech Vaccine and 72 cases after AstraZeneca [2]. The Vaccine Adverse Effect Reporting System (VAERS) database in United States reported so far total of 9 cases of transverse myelitis until 2022 [22]. In a previous brief review study, vaccine-related myelitis was ever reported due to influenza vaccine (H1N7) (7 out of 20 cases), followed by hepatitis B, SARS-Cov-2 vaccine, Japanese encephalitis and Measles, Mumps, Rubella (MMR), in which the predominant patient population affected were males (13 M, 7 F) with an average age of 45.3 years old with age range 7 months to 70 years [2]. Additionally, a separate systematic review identified 60 ATM cases associated with SARS-CoV-2 infection and 23 cases occurring post-SARS-CoV-2 vaccination. The SARS-Cov-2 infection group had total of 55% (33) of them are longitudinally extensive TM (LETM), compared to vaccine group only 4 cases (17%) were reported as LETM. And 5 cases (21%) had symptom onset within a week after vaccination [8]. All above literature described vaccine related ATM specific pattern, including younger age, male dominant and less longitudinally extensive type. However, 285 cases of Encephalitis, meningitis and myelitis were investigated in more than 32 million registry databases, The English National Immunization (NIMS). The mean average age of patients was 58.9–66.6 in vaccine group, which is older than 57.4 in SARS-Cov-2 group. In the 1–28 days post-exposure period, an association wasn’t observed with ChAdOx1nCoV-19 or with BNT162b2, but an association with SARS-CoV-2 infection was identified, the number was around 12.3 excess cases per 1 million exposed. Similarity also found in Guillain-Barre disease over three times higher incidence in comparison between SARS-CoV-2 and ChAdOx1nCoV-19 vaccine group. Further investigate our result that three major types of SARS-CoV-2 vaccine had no obvious association with myelitis after exposure between Covid-19 and non-COVID-19 groups. In assumption, SARS-Cov-2 infection itself may have more relevant effect to myelitis than vaccine, which was considered especially as fighting strategy during pandemic period. Although neurological complications from above condition still rare, but it could cause lifelong disability requiring long-term care for young people [21]. With so many people infected, the overall number of neurological patients, and their associated health burden and social and economic costs might be large, especially Covid infection still going on with different variant of virus and so as vaccination policy. Health-care planners and policy makers must prepare for this eventuality, while the many ongoing studies investigating neurological associations increase our knowledge base [9]. It will be very important to continue to survey the situation of myelitis in COVID-19 by systematically neurological manifestations in Neuro-COVID-19 registries [23] as well as resource allocation for health-care provision.
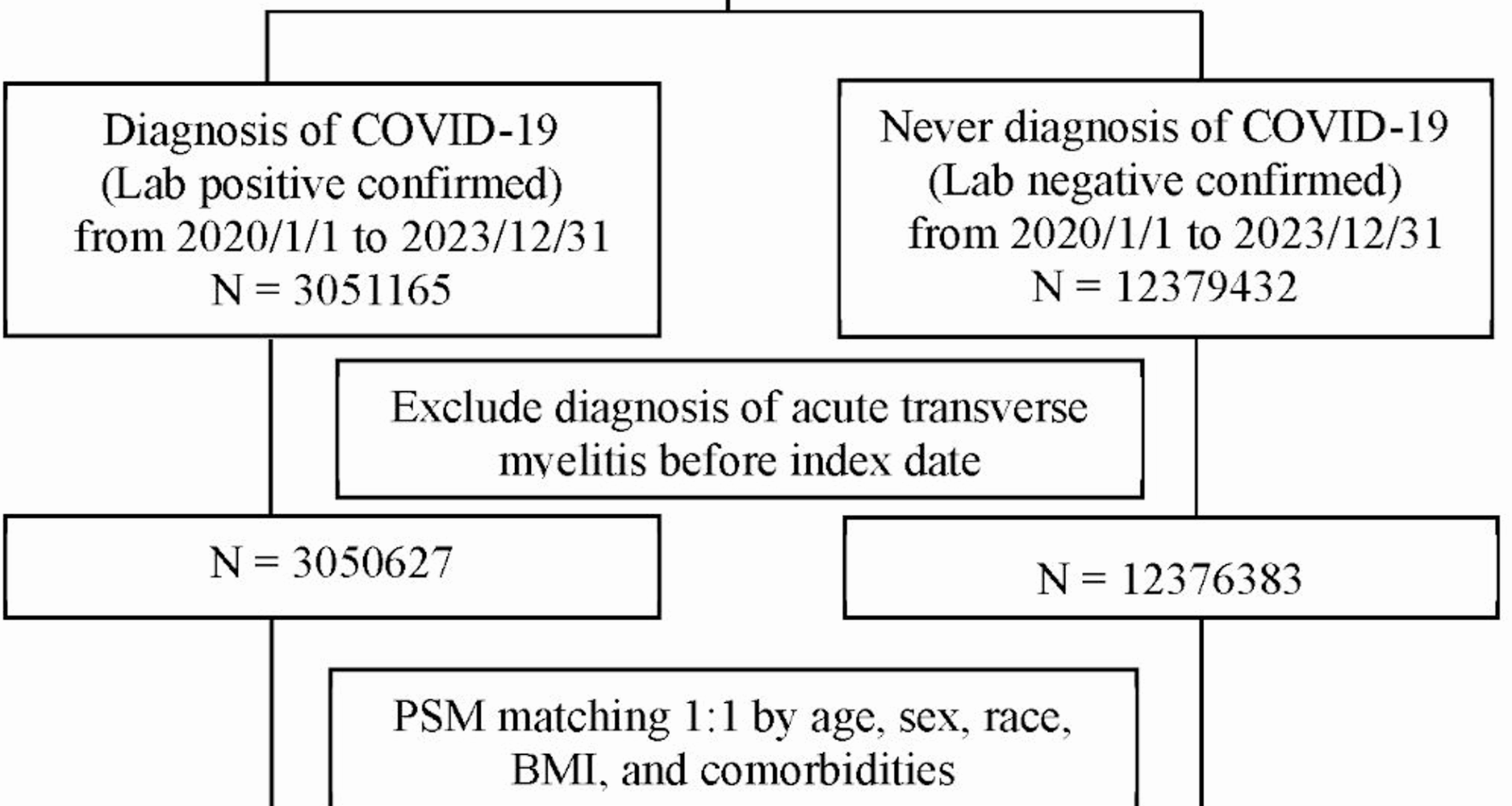
This study has several strengths. First, the data investigated were based from worldwide registry health database, which provided sufficient power to asses extremely rare neurologic diseases like ATM instead of cases series. Second, virus variant duration and SARS-Cov-2 vaccine correlation were first analyzed in our study, which showed likely various aspect of disease. Third, longer follow-up period showed real-world incidence number higher than previous case-control studies. Several limitations have been listed as below. First, SARS-Cov-2 infection diagnosis could be misinterpreted during pandemic period, hidden numbers can’t be avoided in difficult circumstances. Even we used International Classification of Diseases, Tenth Revision, Clinical Modification. (ICD-10-CM) and Logical Observation Identifiers Names and Codes (LOINC) to identify real number of patients. And setting strategy includes patient who were never diagnosed with COVID-19, confirmed by negative lab tests during the same experimental period in comparison group. Second, Analysis of risk of ATM among different vaccines were based from patient with and without SARS-Cov-2 infection, instead of direct comparism betweens patient received any kind of SARS-Cov-2 vaccines or not. The reason leads to extreme small numbner after stratified subanalysis, which numbner indicate 10 if the count is 1–10 in TriNetX system. Future studies should focus on vaccinated recipients. Third, the proportion of vaccinated individuals in our study appears lower than expected, primarily due to limitations within the TriNetXdatabase. Vaccination data may not be consistently captured, especially if vaccinations were administered outside the par-ticipating Health Care Operationss, such as at pharmacies, mass vaccination sites, or community clinics. This underreporting could lead to misclassification of vaccinated individuals as unvaccinated in ourcontrol group. Such misclassification would bias our resultstoward the null hypothesis, potentially underestimating the trueprotective effect of vaccination. Fourth, while the associations observed are significant, they do not establish causality. Although we employed propensity score matching to balance known baseline characteristics between the vaccinated and unvaccinated groups, residual confounding factors may still be present. These factors, which were not captured in our analysis, could include socioeconomic status, healthcare access, pre-existing health behaviors, or other unmeasured variables.