The McDonald Diagnostic Criteria for multiple sclerosis (MS), the guidelines used by healthcare professionals worldwide to diagnose the disease, have been updated and published in The Lancet Neurology.
The revisions, developed by the International Advisory Committee on Clinical Trials in Multiple Sclerosis, introduce new approaches to evaluating evidence of MS, expand considerations for children and patients over 50, and integrate diagnostic methods that are more accessible, affordable, and less invasive.
MS is often difficult to diagnose, and many patients have historically endured years of testing before receiving confirmation. Earlier diagnosis is critical, as it enables patients to begin treatment sooner and improve long-term health outcomes.
“Decades ago, it could take years to diagnose MS. Today it is down to months. And soon, we expect it to get even easier and faster,” says Timothy Coetzee, President and CEO, National MS Society.
Since their introduction in 2001, the McDonald criteria have been periodically revised to reflect advances in research and technology. The average time to diagnosis has been reduced from four years to about one year following the last update in 2017. The 2024 revision is expected to further shorten this timeframe.
The updates were developed through global collaboration among researchers, clinicians, and patient advocacy groups. According to Coetzee, the effort reflects the ongoing commitment to equip healthcare professionals with the tools needed for earlier and more precise diagnosis.
The criteria changes will not affect individuals already diagnosed with MS. However, for those undergoing evaluation, the enhanced guidelines may provide a clearer and faster pathway to diagnosis.
In Mexico, over 20,000 people live with MS, with a higher prevalence among women aged 20 to 40. Irene Treviño, Academic at the Faculty of Medicine, UNAM, notes that MS is the second leading cause of disability in this age group. “Unfortunately, MS is common, and early intervention significantly influences its progression,” says Jhali Hernández, Co-Founder, Otium Physiotherapy and Wellness, to MBN.
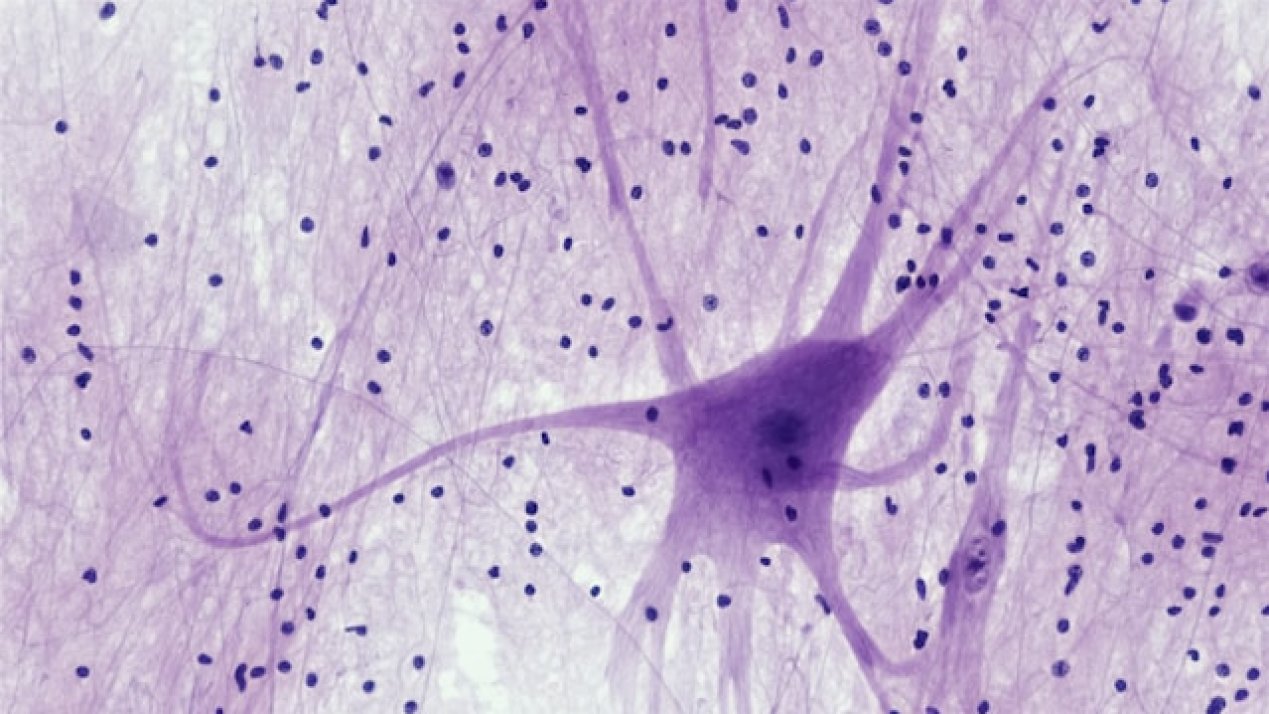
MS is an autoimmune disorder in which the immune system mistakenly attacks the body’s own nerve coverings, according to John Hopkins Medicine. Its symptoms and progression vary widely among patients, complicating diagnosis and treatment. This heterogeneity makes individualized care critical.
Treatment of MS generally consists of three components, which include managing acute attacks or relapses, modifying the disease course, and addressing symptoms, explains Mariana Marcín, Neurologist, ABC Medical Center. Acute relapses are often treated with high doses of corticosteroids such as methylprednisolone to reduce inflammation, she adds. Disease-modifying therapies aim to slow the progression and reduce the frequency and severity of relapses. Symptomatic treatments address specific issues reported by patients, such as fatigue or mobility difficulties, which may not always be apparent during clinical examinations.
Despite advances, MS remains a progressive disease, often leading to brain atrophy over time, says Marcín. Untreated patients typically experience faster loss of brain volume compared to healthy individuals of the same age. The goal of treatment is to delay this progression and maintain patients’ independence and quality of life for as long as possible.