This retrospective cohort study of 4,523 critically ill patients with type 2 diabetes and severe heart failure establishes the TyG-BMI index as a robust predictor of all-cause mortality across multiple time horizons. A key innovation of this work lies in its comprehensive temporal analysis. Whereas earlier research limited focus to single time points, our multi-timepoint design elucidates TyG-BMI’s evolving prognostic role—from early risk discrimination at 60 days to robust long-term survival associations at 365 days—providing novel insights into its clinical relevance across the care continuum. Our findings demonstrate a graded inverse relationship between TyG-BMI and mortality risk, with the lowest quartile (Q1) exhibiting significantly elevated mortality versus higher quartiles at all endpoints: 60-day (Q1 vs Q4 adjusted HR 0.74, 95% CI 0.69–0.77) and 365-day (adjusted HR 0.74, 95% CI 0.68–0.93). Threshold effects identified via restricted cubic splines revealed inflection points at TyG-BMI = 148.73 for 60-day mortality and 163.38 for 365-day mortality, where values below these thresholds were associated with a greater mortality risk reduction per unit increase. These associations persisted after rigorous adjustment for illness severity scores (APACHE III, SOFA, SAPS II), biochemical markers (troponin, BNP, CK-MB), and cardiac function. Critically, subgroup analyses confirmed universal elevation of mortality risk in heart failure with reduced ejection fraction (HFrEF, LVEF ≤ 40%) across all timepoints (HR >1, p < 0.05), contrasting with non-significant associations in HFmrEF and HFpEF subgroups. Collectively, these results underscore TyG-BMI’s utility as a metabolic-body composition composite marker for risk stratification in high-acuity cardiometabolic populations.
T2DM and HF are widespread chronic conditions that significantly impact public health worldwide. T2DM is characterized by insulin resistance and impaired glucose metabolism, leading to long-term complications affecting various organ systems, particularly the cardiovascular system. HF, on the other hand, is a complex clinical syndrome resulting from structural or functional cardiac disorders, which can further exacerbate the complications associated with T2DM. The coexistence of these two conditions is alarming, as they often lead to increased morbidity, mortality, and healthcare costs. Studies have shown that patients with T2DM are at a higher risk of developing HF, and conversely, individuals with HF frequently exhibit impaired glucose tolerance, highlighting the intricate relationship between these diseases, with the elderly subgroup disproportionately affected, as demonstrated by Spanish data showing HF prevalence of 4.3–20.1% in T2DM patients, where older adults constitute a majority [20, 21]. This cohort faces significantly elevated mortality, with diabetes conferring a 2- to fourfold higher cardiovascular risk [22], and in-hospital cardiovascular mortality reaching 5.6–10.8% in diabetic populations, further exacerbated by HF comorbidity in older adults [20]. These converging factors– high prevalence and excess mortality underscore the clinical urgency and societal relevance of focusing research on this vulnerable demographic despite specific inclusion criteria.
Based on prior researches focusing specifically on diabetes and HF, the TyG index demonstrates significant prognostic value in patients with comorbid conditions, with emerging evidence highlighting its particular relevance in elderly populations. For instance, longitudinal cohort studies have consistently shown that higher TyG index values correlate with increased risks of myocardial infarction, stroke, and cardiovascular mortality, independent of traditional risk factors [23,24,25]. Recent findings indicate that the TyG index is associated with an increased risk of both all-cause and non-cardiovascular mortality in younger T2DM patients (< 65 years), though this association is not observed in older patients (≥ 65 years). This suggests that age may modify the relationship between the TyG index and mortality risk in this cohort [26]. Current evidence confirms that an elevated TyG index is significantly associated with increased long-term all-cause mortality in elderly HF patients with diabetes. A 2025 cohort study of 466 patients aged ≥ 60 years (covering the ≥ 65-year subgroup) with chronic HF and type 2 diabetes demonstrated that those in the highest baseline TyG quartile had a 99% higher risk of 10-year all-cause mortality (adjusted HR = 1.99, 95% CI: 1.56–3.14) and an 87% increased risk over the entire follow-up period (aHR = 1.87, 95% CI: 1.22–2.88) compared to the lowest quartile group, independent of conventional cardiovascular risk factors [27]. Notably, longitudinal trajectory analysis further revealed that patients with a high-declining TyG pattern (indicating persistently elevated insulin resistance burden) faced a 116% greater 10-year mortality risk (aHR = 2.16, 95% CI: 1.39–3.35) relative to those with low-declining trajectories [27]. This prognostic value extends beyond diabetes status, as corroborated by a 2023 systematic review of 30 studies (n = 772,809), which established TyG as an independent predictor of adverse outcomes, including mortality, in HF populations irrespective of comorbid diabetes or coronary artery disease [12]. Mechanistically, the TyG index reflects underlying insulin resistance that exacerbates cardiometabolic dysfunction—such as dyslipidemia, hypertension, and impaired myocardial metabolism—which collectively accelerates HF progression in elderly diabetic patients [15]. Consequently, these findings validate the TyG index as a practical, non-invasive biomarker for mortality risk stratification in this vulnerable demographic and support its integration into routine clinical assessment protocols.
The TyG index’s predictive superiority over isolated glucose or triglyceride measurements stems from its ability to capture insulin resistance severity, a key driver of cardiometabolic dysfunction [28]. However, the biological interplay between metabolic dysregulation and adiposity in HF progression remains incompletely understood. While several studies have investigated TyG-BMI in general populations [29, 30], its specific relationship with outcomes in HF patients—particularly those with concurrent diabetes requiring intensive care—constitutes a critical knowledge gap. This is noteworthy because the dual burden of insulin resistance (reflected by TyG) and obesity (reflected by BMI) may have distinct implications for cardiac decompensation compared to either condition alone. Our results significantly advance this field by demonstrating that elevated TyG-BMI is independently associated with reduced mortality risk in critically ill patients with diabetes and heart failure. The graded reduction in mortality risk across increasing TyG-BMI quartiles persisted after comprehensive adjustment for disease severity scores and biochemical markers. This observation aligns with emerging evidence suggesting that obesity may confer survival advantages in critical illness, particularly when accompanied by preserved metabolic reserve as reflected in the TyG-BMI composite [18, 31, 32]. In contrast, only one study has demonstrated that the TyG-BMI index, reflecting both insulin resistance and obesity, is a significant predictor of adverse renal outcomes in patients with stage 1–4 chronic kidney disease (CKD) [33]. Given this, it remains unclear whether the TyG-BMI index is also related to the obesity paradox in patients with heart failure and diabetes. Unlike Dou et al.’s landmark analysis in broad HF cohorts [15], our study addresses critical gaps in diabetic HF—a high-risk phenotype where synergistic insulin resistance and lipotoxicity accelerate mortality. The identification of TyG-BMI thresholds (148.73–163.38) provides clinicians with actionable targets for metabolic-nutritional intervention, directly addressing guideline priorities for this population. Our multi-timepoint design further demonstrates TyG-BMI’s evolving prognostic utility: early risk discrimination at 60 days solidifies into a robust long-term association with improved survival by 365 days—a dynamic pattern unreported in previous research.
Several interrelated biological mechanisms may underlie the observed association between elevated TyG-BMI and improved survival in critically ill patients with diabetes and heart failure. Higher TyG-BMI values likely indicate enhanced energy substrate availability during acute catabolic stress. In critical illness, the body prioritizes gluconeogenesis and lipolysis to meet heightened energy demands [34]. Elevated fasting triglycerides and glucose (components of the TyG index) may provide readily mobilizable substrates for ATP production in vital organs, particularly the heart. Adipose tissue-derived free fatty acids (FFAs) serve as a critical energy source for cardiomyocytes during stress [35], while hepatic glycogenolysis maintains systemic glucose availability [36]. Adipose tissue exerts pleiotropic effects beyond energy storage. In acute illness, visceral fat may act as a “sink” for pro-inflammatory cytokines [37]. Adipose tissue may also buffer inflammatory mediators and provide endocrine protection during acute illness [38]. The TyG index component reflects preserved insulin sensitivity, which facilitates glucose uptake in energy-starved cardiomyocytes during acute decompensation. Insulin enhances pyruvate dehydrogenase activity, optimizing glucose oxidation while reducing toxic lipid intermediate accumulation. Concurrently, BMI-associated nutritional reserves provide amino acids for protein synthesis and glutathione precursors to counteract oxidative stress. This synergy may promote myocardial structural repair, as evidenced by studies showing accelerated sarcomere regeneration in obese heart failure patients with adequate nutritional status [39].
Subgroup analyses revealed critical nuances in the TyG-BMI-mortality relationship. Most notably, patients with HFrEF demonstrated universal elevation of mortality risk across all timepoints. This contrasted sharply with HFmrEF (40–50%) and HFpEF (≥ 50%), which showed no consistent mortality associations except for transient significance in HFmrEF at 90 days (HR 1.21, p < 0.05). Importantly, the inverse TyG-BMI-mortality relationship persisted robustly across all LVEF categories, indicating that the survival advantage associated with higher TyG-BMI operates independently of cardiac systolic function. Age stratification (cutoff: 77.91 years) further modified risk profiles. Patients aged >77.91 years consistently exhibited elevated mortality risk (60-day HR 1.20, 90-day HR 1.16, 180-day HR 1.23, 365-day HR 1.16; all p < 0.05), while younger patients (≤ 77.91 years) showed similar but attenuated effects. BNP levels revealed a striking dose–response relationship: values >500 pg/mL conferred progressively higher mortality risk (365-day HR 3.09, 95% CI 2.58–3.61; p < 0.05), with intermediate levels (100–500 pg/mL) showing variable significance across timepoints. The favorable association between higher TyG-BMI and improved survival was significantly attenuated in patients with prior MI (365-day adjusted HR 0.81, 95% CI 0.72–0.91) compared to those without infarction history (adjusted HR 0.69, 95% CI 0.58–0.82), suggesting established ischemic cardiomyopathy may constrain metabolic reserve benefits. This pattern aligns with studies reporting modified cardiometabolic protection in established coronary disease. The consistency of TyG-BMI’s inverse mortality association across all subgroups—including disease severity (APSIII >53 vs ≤ 53), cerebrovascular comorbidity, and biomarker thresholds—reinforces its broad applicability in critical cardiometabolic populations.
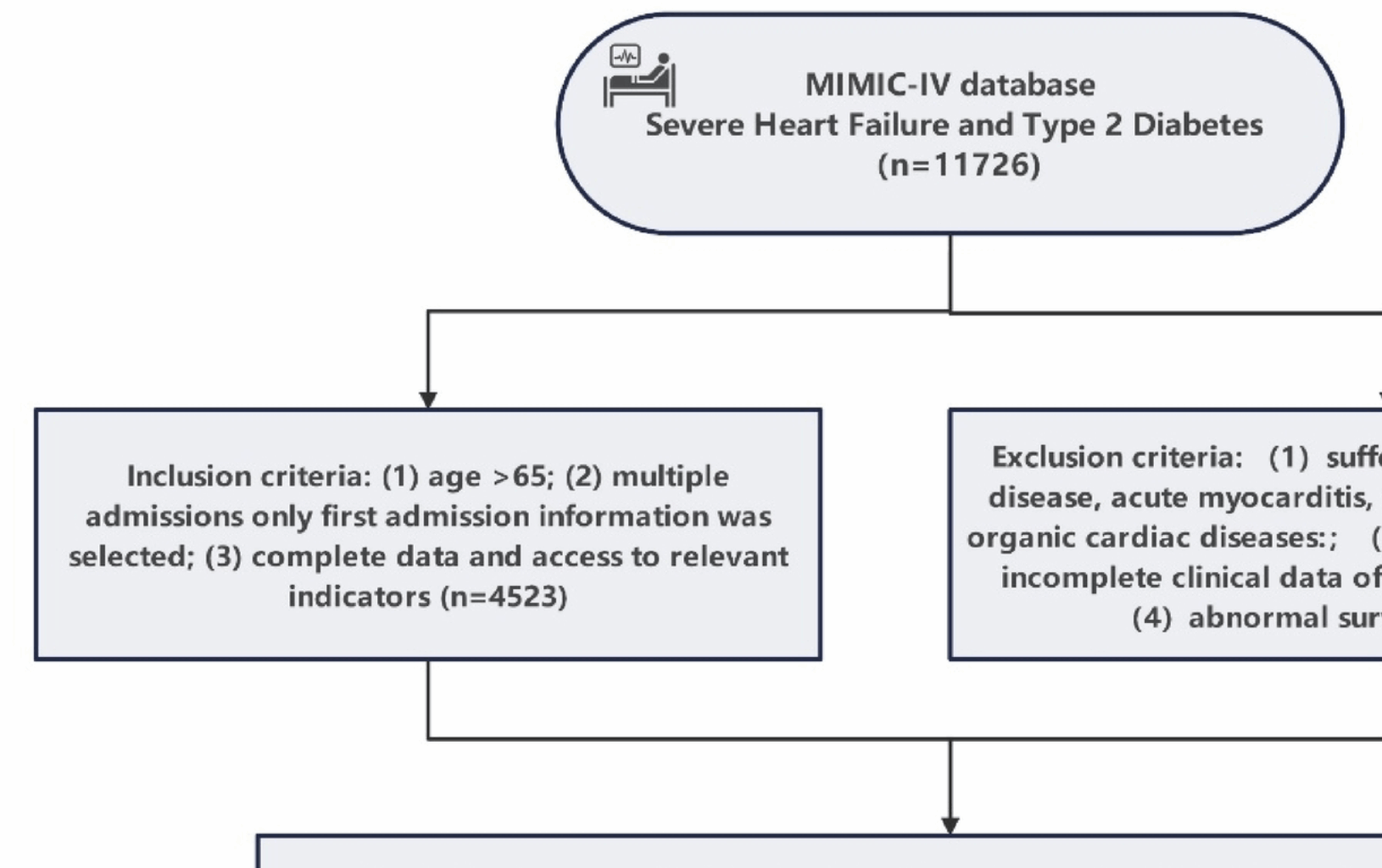
Methodologically, our study extends prior work through three key contributions: (1) adjustment for APACHE III severity score as a comprehensive metric of illness acuity, reducing physiological confounding; (2) extended mortality follow-up to 365 days, capturing long-term prognostic implications; and (3) rigorous evaluation of nonlinear relationships using restricted cubic splines, which revealed threshold effects critical for clinical translation. The large, well-characterized MIMIC-IV cohort enhances the reliability of these findings.
Clinically, TyG-BMI offers a pragmatic bedside tool for risk stratification in diabetic heart failure patients. The identified thresholds may guide nutritional interventions—for instance, targeting TyG-BMI values above 145.82 to optimize metabolic reserve without exceeding inflection points where benefits diminish. Furthermore, our findings advocate for personalized approaches in patients with prior myocardial infarction, where TyG-BMI’s prognostic utility may be limited.
Several limitations warrant careful consideration. First, despite comprehensive multivariable adjustment, residual confounding from unmeasured variables persists—particularly body composition details (i.e., visceral vs. subcutaneous fat distribution), socioeconomic factors (i.e., income/education affecting treatment access), and outpatient treatment adherence patterns. Second, our exclusive reliance on ICU admission measurements of TyG-BMI components (glucose, triglycerides, BMI) introduces information bias, as pre-admission metabolic trajectories and post-discharge dynamics remain unaccounted for, potentially misclassifying long-term risk. Third, the observational design inherently precludes causal inference; while we identified robust associations between TyG-BMI and mortality, unmeasured confounders may partially explain these relationships. Fourth, selection biases merit emphasis: (a) exclusion of pre-ICU deaths may attenuate mortality estimates, and (b) geographic transfer delays (i.e., rural-to-urban hospitals) could limit generalizability to early-presenting populations. Fifth, while our analysis assumes fixed baseline TyG-BMI exposure, we acknowledge potential immortal time bias as patients must survive to ICU admission for biomarker measurement. We mitigated this by excluding early deaths (< 24 h) and initiating mortality assessment at 60 days—a timeframe where HF prognosis stabilizes. Nevertheless, future studies with serial TyG-BMI measurements should implement time-dependent analyses to definitively address this limitation. Finally, our ICU-based cohort inherently represents the severest HF spectrum, restricting extrapolation to ambulatory or community-managed populations.
Future research should validate these findings in prospective cohorts, particularly in non-ICU settings, and explore whether TyG-BMI-guided interventions improve survival. Mechanistic studies are needed to disentangle the roles of adipose-derived cytokines, substrate utilization, and insulin signaling in heart failure progression. Additionally, interactions between TyG-BMI and specific heart failure phenotypes (i.e., preserved vs. reduced ejection fraction) warrant investigation.