Antimicrobial resistance is a natural phenomenon, but the overuse and misuse of antibiotics has made the problem worse – Copyright Venezuelan Presidency/AFP MARCELO GARCIA
Antimicrobial resistance (AMR) is estimated to kill 10 million people per year by 2050, surpassing the death rate of some of the world’s most deadly diseases such as cancer. In 2021, 4.7 million deaths were associated with AMR, of which 1.14 million deaths were directly attributed to the issue (according to the medical journal, The Lancet).
Antibiotic resistance is a form of drug resistance whereby some sub-populations of a microorganism are able to survive after exposure to one or more antibiotics. In the last two decades, the rate at which bacteria are becoming resistant to current antibiotic treatments has substantially increased.
The emergence of antibiotic resistance is a complex problem that is driven by many interconnected factors, of which the use and misuse of antimicrobial agents (antibiotics, antiseptics, disinfectants, and preservatives) amongst other factors, is the main driving force for the development of resistance
Other factors affecting this phenomenon arise since most clinically used antibiotics are broad-spectrum – and are known to 1) harm our gut bacteria and 2) increase resistance rates rapidly over time due to the same antibiotics being used to treat numerous patient illnesses.
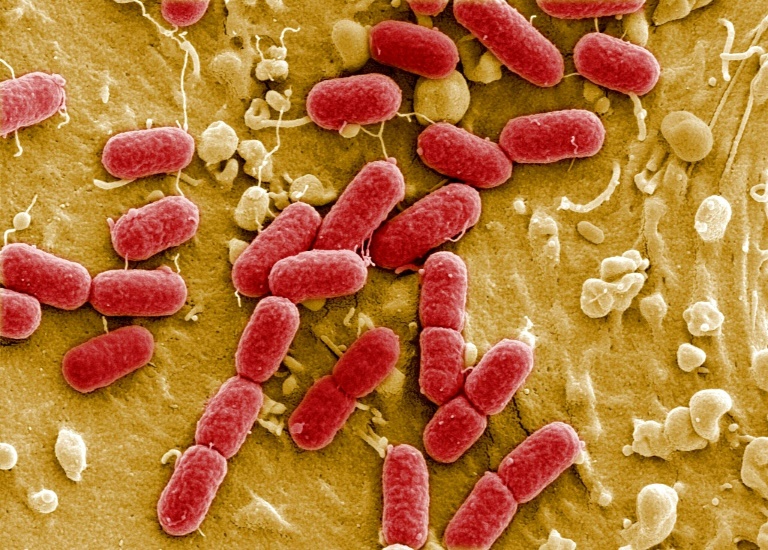
The MIT Jameel Clinic has been conducting research to find solutions to combat this and recently published a paper in Nature. The study focuses on a family of drug-resistant bacteria known as Enterobacteriaceae, which includes Escherichia coli and Salmonella, among other pathogens of concern. These organisms can exacerbate issues associated with an imbalanced gut microbiome.
Is artificial intelligence the answer?
Machine learning is increasingly being seen as the mechanism for finding new antimicrobials. The optimal way to achieve success is through the use of appropriate training data acquisition, as well as the optimal machine-learning model architecture, for a prediction task – finding a new antimicrobial.
By utilising a deep learning algorithm, the Jameel Clinic researchers were able to predict the bindings of an antibiotic to its protein target, determining whether it would be a promising new drug candidate that could treat a range of conditions without harming gut bacteria.
This antibiotic would offer an alternative drug option for patients with chronic inflammatory bowel diseases (IBD), like Crohn’s disease (CD).
“This discovery speaks to a central challenge in antibiotic development,” says Jon Stokes, the lead scienitst and assistant professor of biochemistry and biomedical sciences at McMaster, and research affiliate at MIT’s Abdul Latif Jameel Clinic for Machine Learning in Health.
“The problem isn’t finding molecules that kill bacteria in a dish — we’ve been able to do that for a long time. A major hurdle is figuring out what those molecules actually do inside bacteria. Without that detailed understanding, you can’t develop these early-stage antibiotics into safe and effective therapies for patients.”
The study
The researchers screened 10,747 bioactive small molecules for antibacterial activity against adherent-invasive E. coli (AIEC) and they discovered a compound called enterololin, an antibacterial compound with targeted activity against Enterobacteriaceae species.
The scientists are hopeful that enterololin could overcome intrinsic and acquired resistance mechanisms in clinical isolates when combined with a subinhibitory concentration of SPR741, a polymyxin B analogue used here to increase outer membrane permeability in Gram-negative bacteria.
Subsequent molecular substructure- and deep learning-guided mechanism-of-action investigations revealed that enterololin perturbs lipoprotein trafficking through a mechanism involving a transporter called the LolCDE complex.
Importantly, if the compound is to be become an antimicrobial for humans, enterololin showed low mammalian cytotoxicity in mouse models. It also, in terms of keeping the gut in balance, largely preserved the overall microbiome composition.
In terms of the general importance of the research,the study highlighted the utility of deep learning methods for predicting molecular interactions as well as identifying the promising Enterobacteriaceae-specific antibacterial candidate for further development.
The research appears in the science journal Nature, titled “Discovery and artificial intelligence-guided mechanistic elucidation of a narrow-spectrum antibiotic.”