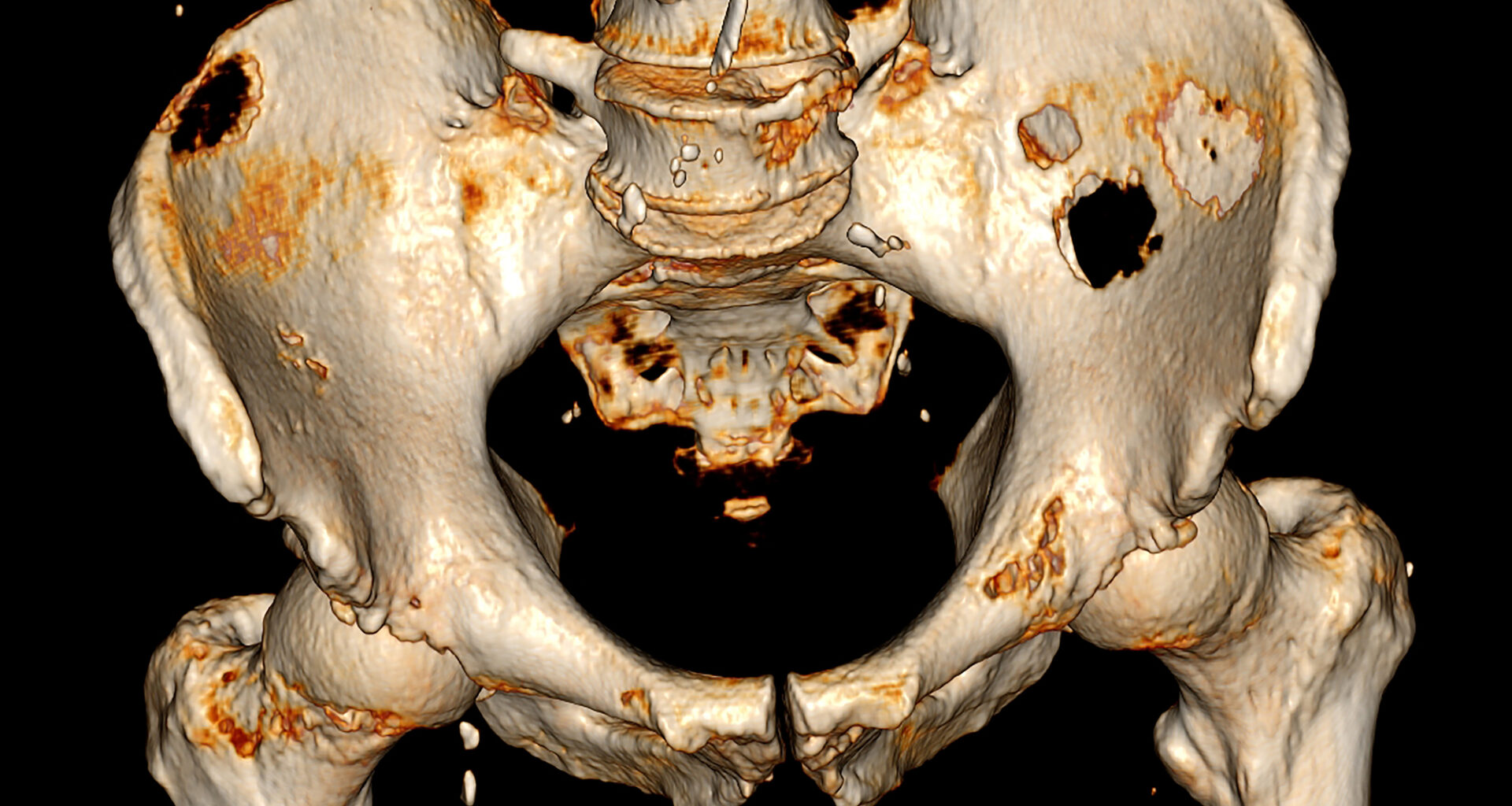
 Credit: Paul Biris/Getty Images
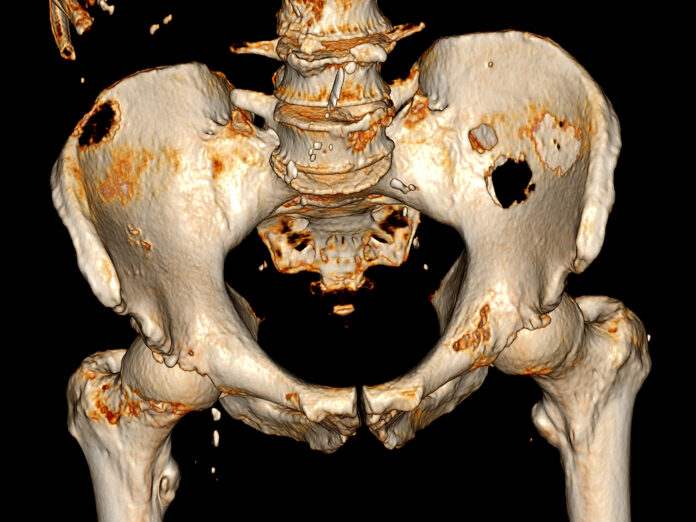
Credit: Paul Biris/Getty Images
Bone metastases in cancer patients resist immune checkpoint blockade (ICB) therapies by hijacking key immune cells and converting them into agents of immune suppression, according to a new study by researchers from the Ludwig Collaborative Laboratory at Weill Cornell Medicine and Nanjing University. The study, published in Cancer Cell, identifies immature neutrophils that are reprogrammed by the DKK1 protein as central players in creating an immunosuppressive state in the tumor microenvironment that helps promote metastatic tumor growth.
“This study uncovers a key reason why immunotherapy often fails in patients with bone metastases,” said study co-leader Taha Merghoub, PhD, deputy director of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. “That failure is caused by the accumulation within the metastases of large numbers of immature, immunosuppressive neutrophils induced by DKK1 that cultivate a profoundly immunosuppressive tumor microenvironment.”
Neutrophils are an important component of the innate immune system and were once thought to play mainly short-lived roles in fighting infection and inflammation. But emerging evidence in the past decade is finding that their role in cancer is far more complex. The current study looked to build on these findings, including earlier work by many of the same researchers, to better understand the role of neutrophils in suppressing immune response.
Bone is a frequent site of metastasis in advanced cancers, with rates ranging from 40% to 90% in lung, breast, and prostate cancers, and increasingly in gastrointestinal cancers. Bone metastases are currently incurable. While ICB therapies, including anti-PD-1 and anti-CTLA-4 agents, have been transformative in many primary tumors, they exhibit poor efficacy in bone metastases. The reasons for this disparity have been poorly understood.
“We aimed to address…knowledge gaps by exploring the role, modulation, and functional pattern of immature neutrophils in the tumor immune microenvironment (TIME), especially in bone metastases,” the researchers wrote.
The new research points to a molecule called Dickkopf-1 (DKK1), found in high levels in both mouse models and human bone metastases. DKK1 reprograms neutrophils into a functionally immature state marked by the suppression of cytotoxic (CD8+) T cells, which are critical to the efficacy of immunotherapies. In this dysfunctional state, neutrophils release CHI3L3, a protein that inhibits T cell activation and tumor-killing activity.
The research team then showed that DKK1 has strong potential as a therapeutic target to aid immunotherapies.
“We tested what would happen if we blocked the effects of DKK1 in mice with bone metastases of triple-negative breast cancer using an antibody to the molecule,” said study co-leader Tao Shi, PhD, a postdoctoral researcher at Weill Cornell. “The results were dramatic. Neutrophils matured into a healthier and more helpful form in which they stopped producing CHI3L3 and no longer suppressed cytotoxic T cell function. As a result, bone tumors shrank and immune checkpoint blockade immunotherapy—specifically anti-PD-1 treatment—started working effectively again, even eliminating tumors in some cases.”
The mechanism by which DKK1 suppresses the immune system involves the CKAP4-STAT6 signaling pathway which drives the expression of CHI3L3. The researchers used RNA sequencing, immune profiling, and imaging techniques such as micro-CT and MRI to track tumor progression and immune activity. In a 2023 study published in the Journal for ImmunoTherapy of Cancer, also led by Shi, the researchers reported that immature neutrophils comprised up to 80% of the neutrophil population in bone metastases by day 14 post-tumor inoculation in mice. Blocking DKK1 not only reduced tumor burden but also enhanced both innate and adaptive immunity in the bone tumor microenvironment.
“These findings suggest that DKK1-blockade could be used as a combination treatment to improve the efficacy of immune checkpoint blockade therapies against bone tumors, for which there are no currently effective therapies,” Shi said. The research also suggests that CHI3L3 and its associated gene expression profile could serve as biomarkers to identify patients likely to benefit from therapies targeting neutrophil reprogramming.
A major strength of the study is its use of multiple bone metastasis mouse models across cancer types including breast, gastric, and lung cancers, and the validation of these findings in patient samples. The use of in vivo imaging and immune assays provided a detailed picture of the immune microenvironment and the effects of DKK1 on neutrophil maturation.
Future research will likely focus on integrating DKK1 blockade with existing immunotherapies, identifying biomarkers for patient stratification, and testing combination strategies in clinical trials. The study also broadens the scope of cancer immunotherapy research by highlighting the role of innate immune modulation. In more general terms, the study highlights the importance of targeting and reprogramming innate immune cells like neutrophils—not just T cells—for cancer therapy.
A DKK1-blocking antibody (DKN-01) is already being tested in clinical trials for other cancers, suggesting a potentially rapid translation to clinical use. “That could significantly hasten progress in translating these findings into patient care,” Shi said.