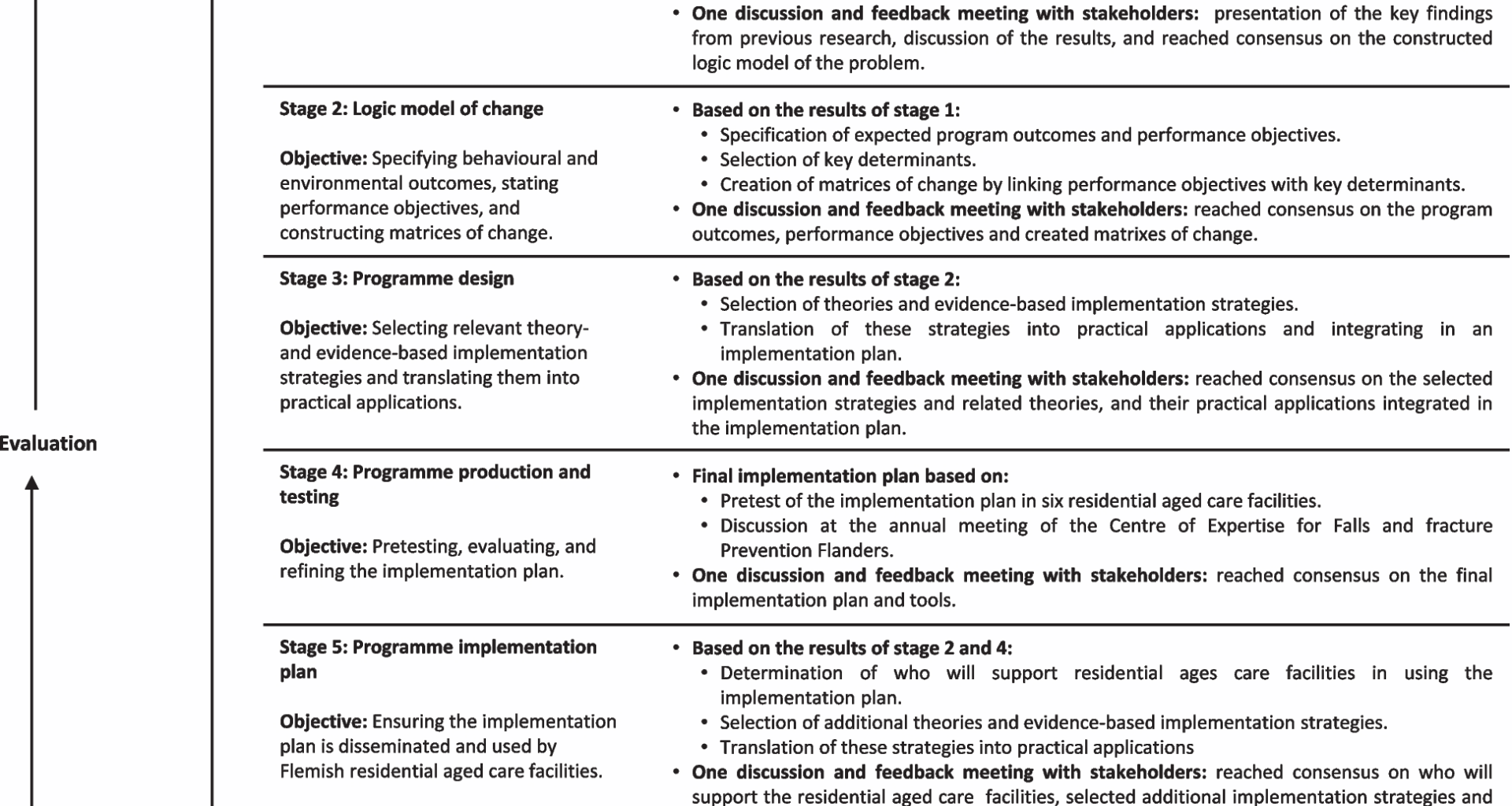
Stage 1: logic model of the problem
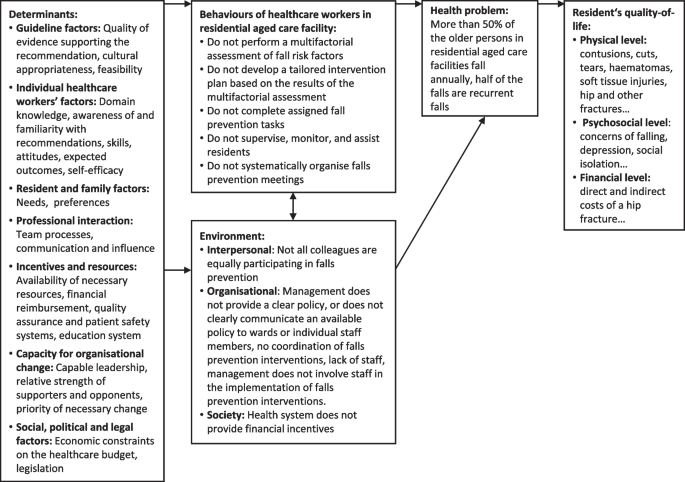
Figure 2 shows the logic model of the problem, consisting of the behaviour of healthcare workers in RACFs and various environmental conditions contributing to residents falling. Findings from the multicentred cross-sectional survey indicated that healthcare workers’ behaviour included the lack of a tailored intervention plan based on the results of the multifactorial falls risk assessment and the absence of regular falls prevention meetings [26]. In addition, environmental conditions were identified at multiple levels, including interpersonal, organisational, community, and societal levels. At the interpersonal level, the survey also found that the unequal participation of colleagues in falls prevention was a key condition [26]. Conditions at the organisational level were, for example, the absence of a clear falls prevention policy supported by the management of the RACF and the lack of staff involvement in the falls prevention implementation. Lastly, at societal level, the absence of financial incentives was found to be an influencing condition [26].
Logic model of the problem [22]
From the systematic review and the multicentred cross-sectional survey, a total of 21 determinants from the TICD checklist could be identified. The most cited determinants were ‘self-efficacy’ (e.g. staff feeling helpless, frustrated, and concerned about their (in)ability to control fall management), ‘priority of necessary change’ (e.g. prioritising other tasks, lack of time), ‘team processes’ (e.g. staff involvement and empowerment, collaboration, teamwork) and ‘communication and influence’ (e.g. failure to communicate falls, (poor) information sharing across shifts/disciplines) [16, 26].
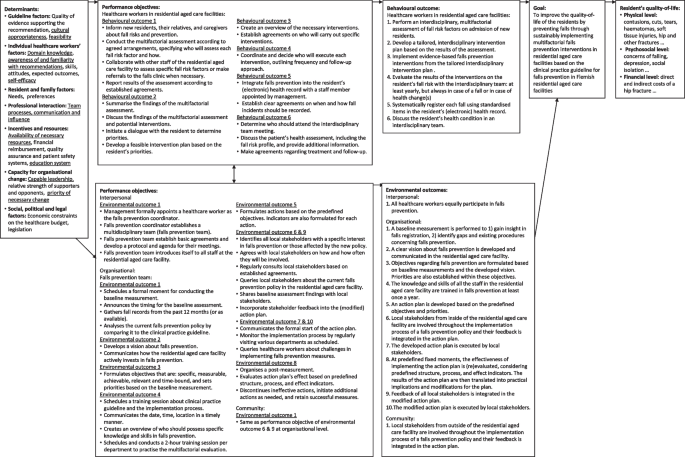
Stage 2: logic model of change
In the logic model of change, six behavioural outcomes (e.g. healthcare workers in the RACF developed a tailored interdisciplinary intervention plan based on the assessment results) and thirteen environmental outcomes (e.g. a clear vision about falls prevention is developed and communicated in the RACF) were stated. For each of these outcomes, performance objectives were formulated. In addition, twelve key determinants (e.g. ‘self-efficacy’, ‘education system’) were identified (see Fig. 3). By combining performance objectives with the key determinants and specifying change objectives, different matrices were created. Additional File 3 shows an example of a matrix of change for the behavioural outcome ‘healthcare workers in RACFs perform an interdisciplinary multifactorial assessment of fall risk factors on admission of new residents’.
Logic model of change [22]
Stage 3: programme design
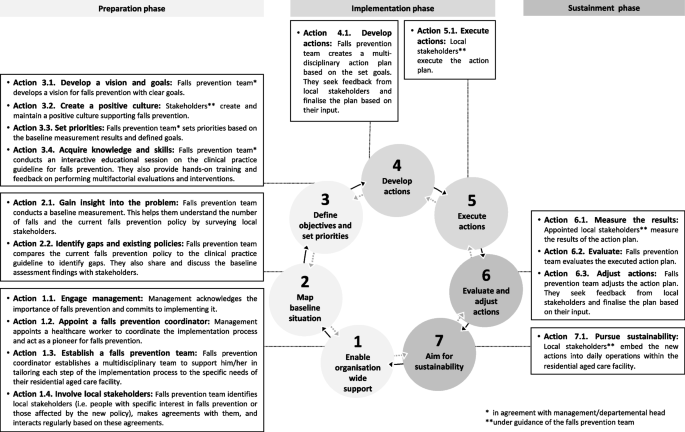
The implementation plan consists of three phases, divided into seven steps (see Fig. 4). These steps are based on the Plan-Do-Study-Act Cycle [29, 30]. The first phase is the preparation, during which RACFs undertake the necessary preparations to start the implementation process. This includes enabling broad support within their organisation, appointing a healthcare worker to coordinate the implementation process (i.e. falls prevention coordinator), establishing a multidisciplinary team to support the falls prevention coordinator (i.e. falls prevention team), mapping the baseline situation, defining objectives, and setting priorities (steps 1 to 3). Subsequently, the actual implementation is performed in the second phase (steps 4 and 5), which outlines the development and performance of implementation actions. Finally, in the last phase, RACFs evaluate and adjust actions, and aim to sustainably anchor the implemented falls prevention policy in their daily practice and quality management system. (steps 6 and 7). More detailed information about these different steps and their actions can be found in Fig. 4.
The seven steps of the implementation plan for residential aged care facilities in Flanders
The main implementation strategies behind the implementation plan are ‘Modelling’, ‘Participation’, and ‘Technical assistance’ from the Diffusion of Innovations Theory; ‘Active learning’, ‘Guided practice’ and ‘Feedback’ from the Social Cognitive Theory; ‘Increasing stakeholders’ influence’ from the Stakeholder Theory; and ‘Tailoring’ from the Trans-Theoretical Model [31,32,33,34]. Table 1 provides an overview of the determinants we aim to influence, along with the selected implementation strategies to address them. It also outlines how these implementation strategies are practically applied within the implementation plan.
Table 1 Implementation strategies and practical applications within the implementation plan [22, 23]
Finally, the implementation plan, along with supporting tools (e.g. knowledge test, meeting protocol template), was made available online via a dedicated platform by the researchers (i.e. online implementation platform). This platform enables the RACF to collaborate within a single document, consolidates all information in one place, and facilitates process tracking. A comprehensive overview of the developed tools, their purposes, and related actions within the implementation plan is provided in Additional File 4.
Stage 4: programme production and testing
The six participating RACFs were located in urban (n = 2), suburban (n = 2) and rural (n = 2) areas. On average, they had 101 high care beds (SD = ± 74.61, range 51–249) and 49 low care beds (SD = ± 19.16, range 35–86). One RACF was public and five were private not-for-profit. During the 12-months implementation process, a total of 70 quality checks were conducted with the falls prevention coordinators of these RACFs, with an average duration of 26 min (range 2–61). From these monthly checks, it was found that one RACF completed all seven steps of the implementation plan. Three RACFs went through six steps, one RACF went through five steps, and one RACF completed two steps of the implementation plan.
In total, 32 determinants from the TICD checklist were identified during the monthly quality checks with the falls prevention coordinators when implementing a CPG on multifactorial falls prevention interventions in the RACFs. This process was supported by the implementation plan and its associated tools. Determinants reported by at least four out of the six falls prevention coordinators were ‘clarity’ (e.g. the implementation plan is perceived as clear, comprehensive and practical), ‘feasibility’ (e.g. multifactorial evaluation is challenging and time-consuming), ‘domain knowledge’ (e.g. lack of knowledge of falls prevention indicators or legislation), ‘awareness and familiarity with the recommendations’ (e.g. the knowledge test increases awareness of falls prevention among staff), ‘residents’ beliefs and knowledge’ (e.g. increasing knowledge on falls prevention among relatives and residents through a flyer), ‘team processes’ (e.g. clear assignments of tasks per discipline regarding falls prevention), ‘availability of necessary resources’ (e.g. lack of time, shortage of staff), and ‘information system’ (e.g. integration of falls prevention into the residents'(electronic) health record). No determinants were reported in the domain ‘Social, political, and legal factors’. A comprehensive overview of the identified barriers and facilitators for each individual RACF can be found in Additional file 5.
Based on the results of the monthly quality checks and the identification of modifiable barriers, adjustments were made to the implementation plan and its supporting tools to better align with the specific context of the RACFs. For example, technical jargon was simplified, and additional details were incorporated, such as the purpose of each step, timing, and specific process of carrying out each step). Additionally, new tools were developed (e.g. an automated falls registration tool ‘Insights into Falls’) or modified (e.g. simplification of the online implementation platform) to facilitate the process (See Additional File 4). Finally, preconditions were added to the implementation plan to foster successful implementation (e.g. ensuring that the managing board of the facility acknowledges falls as a significant health and quality of life issue requiring active intervention, and no simultaneous implementation processes or projects are being conducted concurrently).
These refinements were further shaped by discussions at the annual meeting of the Centre of Expertise for Falls and Fracture Prevention Flanders. The role of the falls prevention coordinator was defined in greater detail, highlighting key competencies such as expertise in falls prevention, motivational skills, and the ability to coordinate implementation processes. Additionally, the ideal composition of the falls prevention team—comprising professionals such as physiotherapists, occupational therapists, and nurses—was outlined, along with essential team member competencies, including teamwork and voluntary engagement, to enhance implementation effectiveness.
Stage 5: programme implementation plan
We identified facilitators as potential support for the implementers. An implementation facilitator is an external falls prevention champion who provides advice and new insights. They coach the falls prevention coordinator and the falls prevention team in successfully implementing the CPG. To prepare them for this role, the implementation facilitators received training focused on coaching skills, the CPG, the implementation plan with emphasis on their role, and the outlined specific tasks they need to undertake. The falls prevention coordinator and falls prevention team of the RACF can rely on them for up to 65 contact hours and for a minimum of two years. This is part of ‘Implementation Guidance’, a large-scale falls prevention implementation initiative in more than 100 RACFs in Flanders, funded by the Flemish Government [35].
Besides their initial training, implementation facilitators receive ongoing support from the research group through biannual peer coaching sessions, promoting sharing experiences and mutual learning. Moreover, every three months they receive assistance and advice from a trained researcher by phone. Finally, implementation facilitators have access to an online platform for asking questions to other facilitators and revisiting training information.
The implementation strategies behind ‘Implementation Guidance’ are ‘Technical assistance’ from the Diffusion of Innovations Theory, ‘Active learning’, ‘Guided practice’ from the Social Cognitive Theory, and ‘Participatory problem solving’ from the Organisational Development Theories [17, 33, 34, 36]. Table 2 provides an overview of the determinants we aim to influence, along with the selected implementation strategies to address them. It also outlines how these implementation strategies are practically applied within ‘Implementation Guidance’.
Table 2 Implementation strategies and practical applications within Implementation Guidance [22, 23]Stage 6: evaluation plan
The implementation plan includes possible indicators for falls prevention, each accompanied by its definition. These indicators are categorised into three different types, as outlined by Mainz (2003) [37]: structural indicators (e.g. presence of a prevention coordinator in the RACF), process indicators (e.g. proportion of residents for whom various fall risk factors were evaluated), and outcome indicators (e.g. number of fall incidents) [37,38,39,40,41,42]. These indicators can be used by the falls prevention team to evaluate whether goals are reached (‘Action 4.1: Develop actions’). The team also determines how this evaluation will take place and by whom data for these indicators will be collected. The results of the evaluation are discussed using the evaluation method: STOP-START-CONTINUE, which indicates actions to stop, start, or continue (‘Action 6.2: Evaluate’ and ‘Action 6.3: Adjust actions’) [43, 44]. In addition, step 7 of the implementation plan includes a list of ten sustainability criteria that the falls prevention team needs to review at least once a year (see Table 3). These criteria evaluate the extent to which the RACF sustains its implemented falls prevention policy and whether additional actions need to be developed.
Table 3 Overview sustainability criteria
The sustainment phase in the implementation plan necessitates the falls prevention team to engage in a cyclical process, wherein steps 4 to 7 are performed at least yearly to ensure sustainability. For example, when it is discovered through the sustainability checklist of the implementation plan (‘Action 7.1. Pursue sustainability’) that criteria are not met, new actions are to be developed in the initial action plan (‘Action 4.1. Develop actions’), executed (‘Action 5.1. Execute actions’), and later evaluated (‘Action 6.2. Evaluate’) and potentially adjusted (‘Action 6.3. Adjust actions’). This enables continuous quality improvement of falls prevention care in RACFs [45].