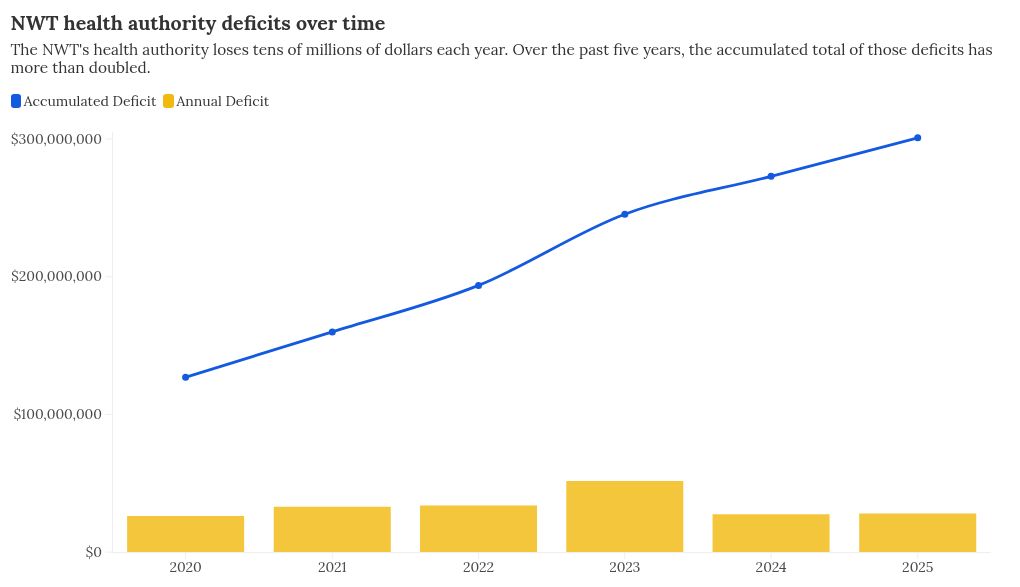
The NWT’s health authority is still spending tens of millions of dollars it doesn’t have each year but things are getting better, leaders said at Wednesday’s annual meeting.
When the territory-wide health authority came into existence in 2016 – through the amalgamation of various regional authorities – it inherited about a $50-million accumulated deficit from those regions. Part of the rationale for the amalgamation was to help control spending.
Financial statements presented on Wednesday show the health authority now has an accumulated deficit of $301 million. It posted a deficit of $27.98 million for 2024-25.
Kim Riles, the health authority’s chief executive officer, said the deficit is driven by issues like underfunding for physician costs, medical travel and increases agreed through collective bargaining.
Unlike some areas of government, the health authority is allowed to set a deficit budget, meaning it can plan each year to spend more than it will receive.
In 2024-25, the authority actually expected to lose more than $60 million, so losing $27.98 million represented – by that measure – a success.
“What we have done over the last number of years is deep dives into programs to articulate our historical trends and what we actually know we require to operate as status quo,” said Riles.
“We’ve had great success over the years, which is in part why we budgeted $61 million but arrived at $28 million [as a deficit] last year. It’s because we were successful in securing new funding to be able to close that gap in a number of key areas.”
About 95 percent of the health authority’s funding comes from the NWT government.
“We continue to work away at the plan throughout the year. We don’t just say, well, it’s a deficit, let’s just run it,” said Dan Florizone, the public administrator who replaced a multiple-person leadership council at the top of the health authority in late 2024.
“We’re actually trying continuously to get ourselves back into balance. It’s just such a significant effort.”
Goal of reducing medical travel
The accumulated deficit of the health authority has worried territorial politicians for years.
When it hit $194 million in 2022, MLAs expressed “alarm” and made a series of recommendations.
Last year, with the accumulated deficit at $273 million, Premier RJ Simpson announced a healthcare system sustainability unit to examine how care in the NWT can meet residents’ needs without resulting in a ballooning deficit.
While that work is ongoing, Florizone’s main target is medical travel.
Medical travel – the act of sending people away from their home community for treatment – costs the territory huge sums each year and is a process most people find joyless and daunting.
Florizone wants to reduce medical travel by offering more services locally so people don’t have to leave home in the first place.
But in a hiring climate where attracting and retaining healthcare staff has been difficult for years, figuring out how to do that is tricky. The health authority is running a pilot project in the Dehcho to see if it can generate some solutions, details of which remain partly under wraps.
“That’s what we can do – look at how we can do that efficiently with the patient at the centre, making sure their care experience is acceptable and culturally safe,” said Riles.
“That’s work we are going to undertake this year, particularly as it pertains to the services in small communities in the Dehcho region.”
 Kim Riles, the NWT health authority’s chief executive officer. Ollie Williams/Cabin Radio
Kim Riles, the NWT health authority’s chief executive officer. Ollie Williams/Cabin Radio
Asked at the annual meeting by a resident how technology factors into the health authority’s plans, Florizone quipped “we’re not going to put a robot in every community and have it take over” – but he does foresee a role for technology in helping to reduce medical travel.
He gave the example of small units that can provide instant results for a variety of tests that might otherwise require travel.
“It’s expensive on a per-unit basis but far less expensive than the trip or flight down the road,” Florizone said.
Another option is evolving virtual care.
“Right now, we have TV screens that are hooked up to cameras. If we can get better and more robust bandwidth, there are adaptations to that technology that allow you to do blood pressure, that allow you to look in people’s ears, allow you to do ultrasounds,” Florizone said.
“We know right now that probably – and this is ‘Dan’s target’ – I can reduce travel by maybe 20 percent from the health cabin communities. But that’s a hypothesis. Now we need to prove that.”
Florizone said medical travel costs in the current financial year are a concern. He wants federal funding to increase so it fully covers costs associated with getting people to the right place for the care they need.
“We have agreements with the federal government around First Nations and Inuit care and service. We need to be fully funded there,” he said.
“So while last year’s shortfall in medical travel may have been $5 million, it could be $20 million, $25 million, it could be as high as $40 million this year.
“This is not sustainable spending. We will be working very, very closely and carefully with government to make sure we get our fiscal house in order … If all of this were within our control, we’d have balanced our budget by now. But there’s a lot of things like travel that I couldn’t say we can control 100 percent of. So we’re trying our best.”
One improvement each week
Elsewhere at the annual meeting, Riles said the health authority is “actively working” to increase Indigenous representation within its workforce.
As of March 31, 2025, she said, the authority had 1,866 employees, of whom 20.3 percent were Indigenous.
Riles said the authority is also trying to develop its organizational culture.
“We want a workforce of problem seekers and problem solvers, and we will ensure investment and training and development as well as culturally safe, welcoming workspaces that are there to support collaboration and effective service delivery,” she told a small audience at Yellowknife’s Chateau Nova Hotel. (Health minister Lesa Semmler sent her regrets as she’s touring the Nunakput district with colleagues this week.)
“We’re focusing on quality and changing the narrative,” Riles said. “We want to shift the focus to one around enabling rapid, continuous quality improvement and making sure that the stories of our many successes are shared and celebrated.”
An example of this “rapid and continuous improvement” approach is an initiative named 52 Improvements in 52 Weeks, which Florizone has said means taking one small change each week – as suggested by employees – and experimenting to see if it works, then rapidly incorporating the change if it’s successful or abandoning it if it isn’t.
The authority has published examples of some changes it has tried so far under this banner.
They include signage indicating staffing levels at the Stanton Territorial Hospital emergency room, better toothbrushes for stroke patients, and an online callback request form for lab services.
“The overarching goal to be reflected in our work during the year ahead is to improve access to care in meaningful ways that are both equitable and sustainable for everyone who needs it,” said Florizone.
‘Where we were five years ago is significantly different today – much improved in terms of the financial controls. the adherence to those financial policies and protocols, and we’re getting better as we move forward.
“There’s more work to be done but we’re on the right path.”
Related Articles