Main finding
This meta-analysis did not reveal a significant association between AM and all-cause, cardiovascular, or suicide mortality, although significant heterogeneity was observed across studies. According to the sex-specific analysis, AM was associated with a 1.21-fold higher risk of CVD mortality in women, with no statistical heterogeneity. There are some indications that MA increases the risk CVD mortality by 1.25-fold, particularly in women; however, these results were pooled from a small number of studies. Thus, uncertainty persists regarding the true association between AM, including MA and MO, and all-cause mortality as well as specific-cause mortality.
Comparison with previous studies
Our findings are consistent with those of previous studies [5, 7], which also reported that in the general population with AM, there was no significant association of AM with all-cause or cardiovascular mortality, although significant heterogeneity across studies was noted. However, this meta-analysis adds to the existing literature by including more recent studies and conducting detailed subgroup analyses based on the sex, migraine type, region, data source type, migraine diagnosis, medication adjustment, and mean follow-up duration to detect heterogeneity. It was found that the diagnostic method and mean follow-up duration may be sources of heterogeneity in studies on all-cause mortality, which provides new insights compared to previous research. Notably, we observed an association between male patients with AM and a higher risk of cardiovascular mortality, which was characterized by lower heterogeneity. This finding extends previous reports that such a significant association was only observed in female populations [6]. Additionally, this is the first large-scale cohort study to examine the relationship between AM and suicide mortality. Although the number of studies on suicide mortality is limited, our results suggest that AM, particularly in women, is associated with a higher risk of suicide mortality.
Interpretation of findings
The relationship between migraine and all-cause mortality remains unclear. This meta-analysis found no significant association between AM and all-cause mortality, with substantial statistical heterogeneity. This may be attributed to the primary association between migraine and CVD, psychiatric disorders, and neurological conditions [32,33,34]. Consequently, migraine may specifically increase the risk of CVD or suicide-related mortality; however, its impact on other causes of death requires further investigation. To address this high heterogeneity, we conducted meta-regression analyses to explore sex, migraine type, region, data source type, migraine diagnosis, medication adjustment, and mean follow-up duration. Diagnostic approach and mean follow-up duration have been identified as potential sources of heterogeneity. Further subgroup analyses revealed that MA was associated with a higher risk of all-cause mortality; however, this finding was unreliable owing to the inclusion of only two studies. Conversely, a significantly lower all-cause mortality risk and lower heterogeneity were observed in studies using physician diagnoses and in those with a follow-up duration shorter than 12 years. There are several possible explanations for these findings. First, self-reported migraine diagnoses depend on patients’ subjective recall, which increases the likelihood of misclassification and compromises exposure accuracy. By contrast, physician diagnoses based on standardized criteria are generally more accurate and consistent, resulting in reduced heterogeneity in studies employing this method. Second, patients receiving formal physician diagnoses typically have access to more comprehensive clinical management, including systematic evaluation, appropriate medication regimens, and regular follow-up care. Such structured medical interventions may effectively mitigate the burden of migraine itself as well as associated comorbidities, thereby contributing to the observed reduction in mortality risk. The observation that the mortality rate of the AM population is lower than that of the general population in short-term studies stems primarily from two types of bias. First, insufficient accumulation of death events: Mortality is a low-incidence outcome. During short-term follow-up (< 12 years), the small number of death events makes the results vulnerable to random variation, which exaggerates the spurious between-group differences. In contrast, longer follow-up duration leads to more accumulated death events, diluting random errors and yielding more reliable results. Regarding outcomes such as mortality and disease progression, the driving factors are more concentrated for short-term outcomes, while long-term outcomes are influenced by the superposition of multiple etiologies, which expands the differences in results across studies.
In this meta-analysis, we found no evidence linking AM to an increased risk of CVD mortality. However, this result should be interpreted with caution because of the high heterogeneity observed in the pooled estimates. Although the meta-regression analyses failed to identify statistically significant sources of heterogeneity, sources of clinically relevant heterogeneity remained. Interestingly, sex-specific analyses found that women with AM, particularly those with MA, exhibited a significantly higher risk of CVD mortality, with low statistical heterogeneity. The mechanisms underlying the association between migraine and CVD are complex and multifactorial. Potential contributing factors include genetic predisposition, endothelial dysfunction, anatomical abnormalities, and sex hormone dysregulation, particularly in women [35, 36]. Additionally, our meta-analysis revealed that women with AM, particularly those with MA, exhibited a significantly elevated risk of CVD mortality. Female patients are more likely to use oral contraceptives and experience estrogen fluctuations, both of which may exacerbate oxidative stress in endothelial cells, leading to endothelial activation and increased cardiovascular risk [37]. Additionally, men with AM had a higher risk of CVD mortality. This may be associated with the higher prevalence of CVD risk factors, such as hypertension and dyslipidemia, in men [38]. Subgroup analyses revealed that MA was associated with a higher risk of CVD mortality, with reduced heterogeneity compared with AM. This association may be driven by specific factors in patients with MA, such as cortical spreading depression, which can trigger localized inflammation and oxidative stress, impair vascular endothelial function, and contribute to increased cardiovascular events [39]. Furthermore, up to 60% of patients with MA have a patent foramen ovale, which may increase the risk of myocardial infarction and CVD mortality by allowing thrombi to enter the coronary arteries [40]. Although the association between MA and CVD mortality risk in female populations can be explained mechanistically and clinically, the number of studies included in our analysis was limited, typically three to four, and the reliability of these results still requires validation.
Our study suggests a potentially higher suicide mortality risk among patients with migraines, although this association was not statistically significant. Chronic pain, particularly in patients with migraines, may contribute to depressive symptoms and hopelessness compounded by impairments in occupational and social functioning [41]. These factors can precipitate suicidal ideation and behaviors potentially influenced by dysregulated serotonin (5-HT) levels [42, 43]. The inclusion of four cohort studies [14, 15, 21, 24] in this meta-analysis indicated that depression attenuates the relative risk of suicide in patients with migraine compared to non-depressed individuals, suggesting that comorbid depression is a significant driver of suicide risk in patients with migraine. However, the residual risk associated with migraines, independent of depression, warrants further investigation. Furthermore, we observed a significantly higher suicide risk among female patients with migraine; however, the limited number of available studies requires caution when interpreting this result.
Limitations
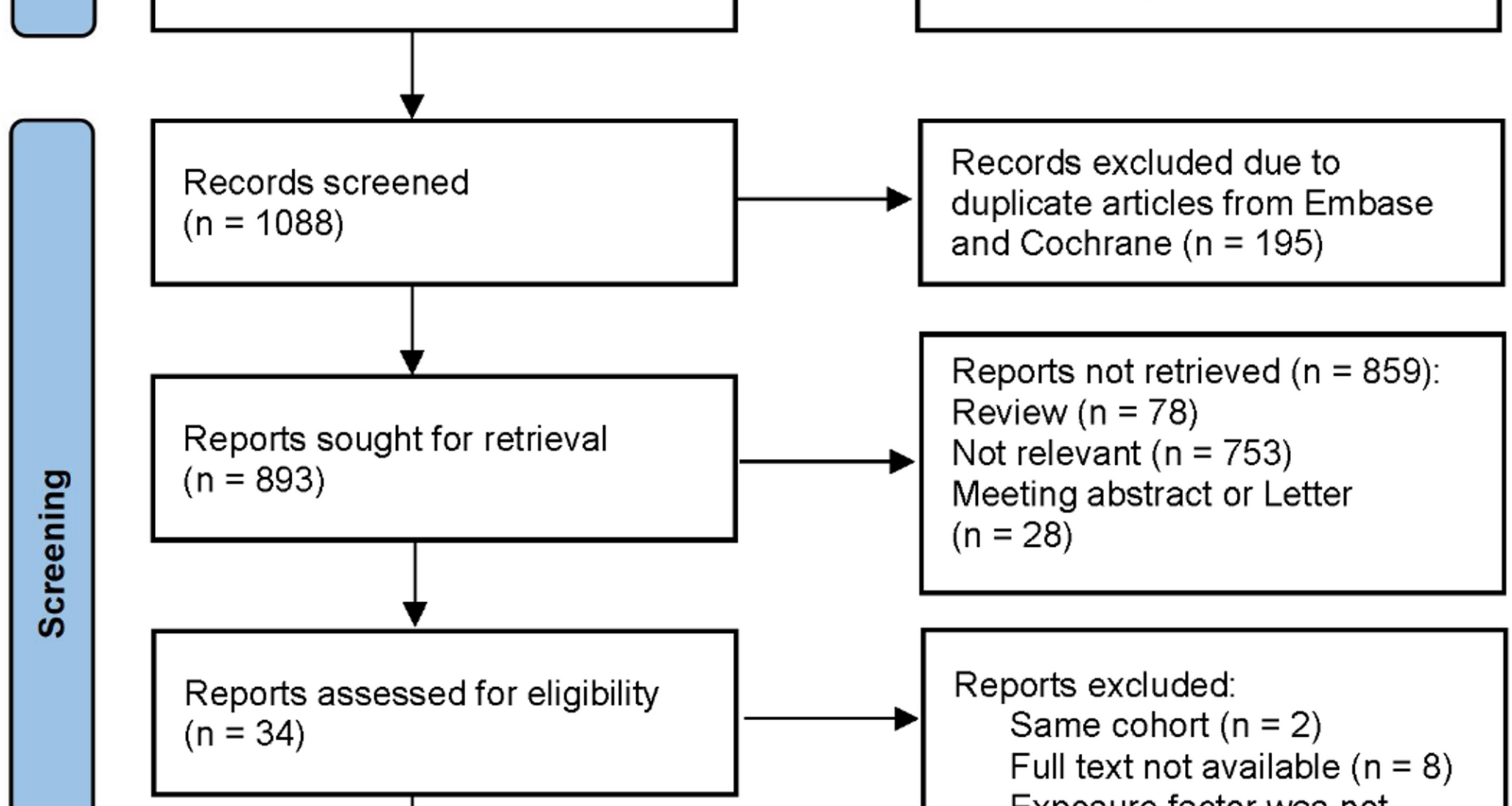
This meta-analysis had several limitations that merit careful consideration. First, the use of all-cause and CVD mortality as outcomes may have been overly broad, contributing to substantial heterogeneity in the pooled results. Only two studies clearly defined all-cause mortality, with notable variability in definitions, and only four studies specified CVD mortality, with similar inconsistencies. This variability is likely to drive the observed heterogeneity. Additionally, the incomplete reporting of migraine diagnoses hindered our ability to fully explore the sources of heterogeneity. Although meta-regression analyses identified diagnostic methods and mean follow-up duration as potential contributors, the limited number of studies warrants cautious interpretation owing to reduced statistical power. Second, the key factors influencing survival, such as age, were not included in the subgroup or meta-regression analyses. This was due to the overlapping age ranges across the studies, compounded by the incomplete reporting of these data, which may have influenced the results. Third, the limited representation of countries and regions, particularly in Asia, restricts the generalizability of our findings. Fourth, although we performed meta-and subgroup analyses based on diagnostic methods and data sources, missing data on the diagnostic criteria precluded further exploration, limiting the depth of our analysis. Fifth, the included studies did not stratify migraine severity or attack frequency, thus preventing an analysis based on these clinically relevant variables. Sixth, although no publication bias was detected, the small number of studies, particularly on suicide-related mortality, reduced the statistical power of Egger’s test, limiting the reliability of this assessment. Finally, although definitive evidence linking migraine medications to mortality is lacking [44], studies, including those in this meta-analysis, suggest that commonly used treatments in patients with migraines, such as triptans [30, 45], calcitonin gene-related peptide inhibitors (CGRP) [46], ergotamines [29], antiepileptic drugs (AEDs) [47], and oral contraceptives [48], may increase the risk of cardiovascular events. Conversely, other frequently used medications such as aspirin [49] and beta-blockers [50] may confer vascular protective effects, potentially influencing mortality outcomes. Furthermore, migraine is frequently comorbid with psychiatric disorders such as depression and anxiety, which may lead to increased antidepressant use and heightened suicide risk [51]. These factors may have compromised the robustness of the findings. Of the studies we included, 7 controlled for drug factors related to migraine prevention and treatment, while 11 did not adjust for such factors—this may have a potential impact on the results.
Implication
Our meta-analysis revealed no association between AM and increased risks of all-cause, CVD, and suicide mortality, with high heterogeneity. However, AM appeared to elevate the risk of suicide mortality, with subgroup analyses suggesting that specific migraine populations, particularly women, may also have a higher risk of CVD mortality. Considering that the Systematic Coronary Risk Evaluation (SCORE) does not yet include migraine as a risk factor, coupled with the elevated suicide risk associated with psychiatric disorders [52, 53], there is an urgent need for interdisciplinary collaboration among headache, stroke, cardiology, and psychiatry centers to conduct long-term follow-up cohort studies, which are essential to investigate whether migraine prevention can reduce specific mortality risks or endpoint events. The American Registry for Migraine Research (ARMR) has taken a significant step forward by integrating multi-institutional data [54]. Future efforts should aim to integrate international migraine cohort data to enhance the generalizability of the research results and further conduct stratified analyses according to age, sex, ethnicity, migraine subtype, and severity to accurately identify high-risk populations. Furthermore, exploring potential mechanisms through which migraine may influence mortality, such as vascular endothelial dysfunction, immune dysregulation, and neurotransmitter imbalances, alongside clinical studies to develop targeted preventive strategies, has profound public health implications.