Study setting
This study was conducted at the Acute Stroke Unit of Hospital Seberang Jaya (ASUHSJ), a specialized six-bed unit dedicated to the care of acute stroke patients. ASUHSJ was chosen due to its high patient activity levels and the increased risk of falls among its patients.
SMART AI patient sitter system
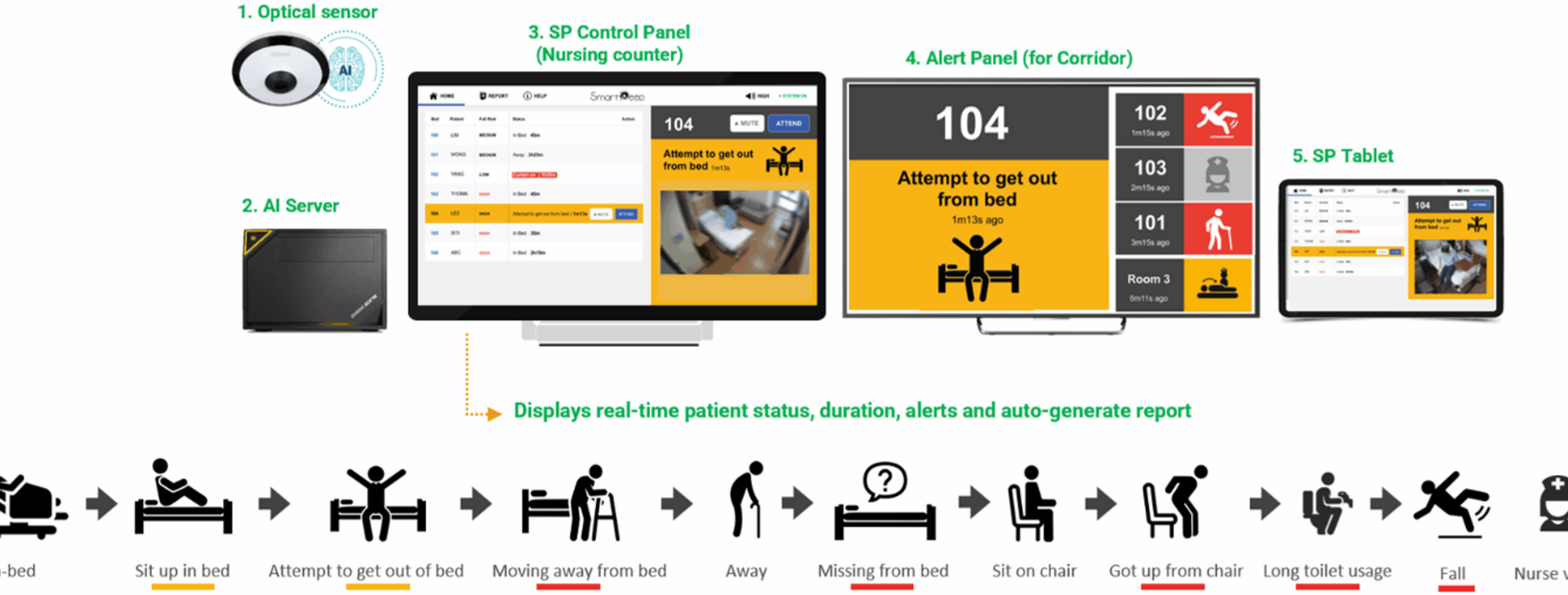
The SMART AI Patient Sitter system, an artificial intelligence-powered solution designed for fall detection and prevention was developed by SmartPeep, a health technology company based in Singapore. The system enables continuous, non-contact monitoring of patients within hospital settings. The system comprises four key components: optical sensors, a centralized AI engine, control and alert panels, and a secure integration interface to support workflows (Fig. 1).
The SMART AI patient sitter system
The optical sensor, typically mounted on the ceiling or high on a wall, captures wide-angle visual data of the patient’s bed area. It supports standard monitoring formats, including fisheye and thermal imaging, and transmits real-time video streams to a local AI server. The sensor is positioned to detect postural changes and movement patterns, such as sitting up or attempting to leave the bed, while limiting the capture of facial details to support patient privacy.
The AI engine, hosted on either a local or centralized server, runs advanced computer vision algorithms to analyze motion in real time. It is capable of detecting high-risk behaviors such as unassisted bed-exits, extended time spent near the bed edge, and potential falls. By learning spatial and temporal movement cues, the system distinguishes between routine activity and actual risk, thereby reducing false alarms. When an anomaly is identified, the AI generates a color-coded alert (for example: red for urgent or amber for warning) to facilitate rapid and prioritized staff response.
The control panel, located at the observation counters, provides a dashboard view of all monitored beds. Blurred preview images are displayed, deliberately anonymized to protect patient identity while preserving key visual indicators such as posture and movement. The interface allows staff to monitor alert history, and to activate or deactivate patient monitoring based on consent and clinical needs.
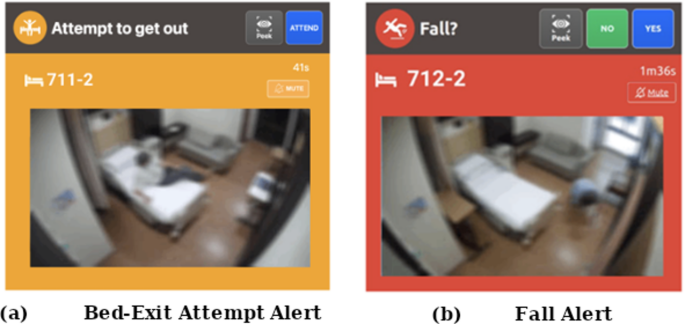
Figure 2 show examples of the image outputs on the control panels for a bed-exit attempt and a fall. The design allows for the capture of essential patient activity data while reducing the visibility of identifiable facial features, supporting both patient safety and data confidentiality.
Blurred visual output displayed on the control panel at the observation counter when a patient (a) attempts to leave the bed, and (b) falls in the room
To further support staff responsiveness, an alert panel is installed outside patient rooms. Mounted on the corridor ceiling, this panel uses visual indicators such as icons and colored lights to signal the priority of alerts and guide staff to the appropriate room, even when they are away from the central monitoring station. This facilitates faster incident localization and decision-making during high-activity periods.
The system also incorporates staff presence recognition by detecting uniformed staffs to automatically acknowledge and dismiss alerts upon arrival, eliminating the need for manual confirmation. This feature enables automated logging of response times, which can support performance evaluation and workflow optimization.
In addition, the system’s secure integration interface ensures compatibility with hospital infrastructure and clinical workflows. This includes adherence to data privacy protocols, compliance with healthcare information technology (IT) standards, and interoperability with existing alert systems and electronic health records.
Collectively, these components contribute to a comprehensive, privacy-conscious AI platform that enhances fall prevention, streamlines response efforts, and enables monitoring of care processes particularly in high-risk settings such as acute stroke or geriatric wards.
Fall risk-based sensitivity configuration
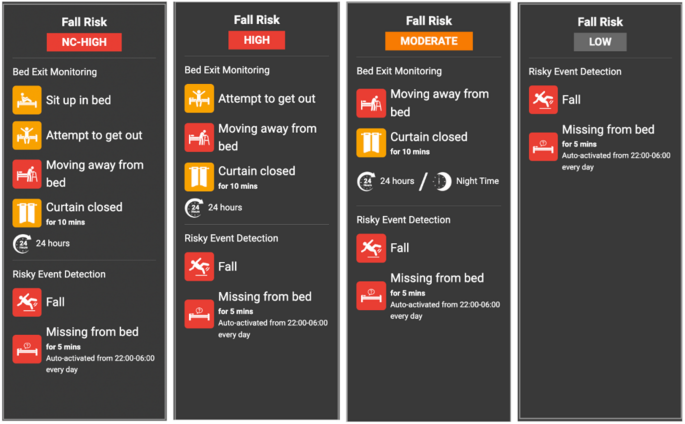
Figure 3 illustrates how the SMART AI Patient Sitter system adjusts its monitoring sensitivity according to each patient’s assessed fall risk level. Patient monitoring is categorized into four category NC-high (non-compliant high), high, moderate, and low, each with its corresponding alert thresholds and event triggers.
Staff register each patient in the system based on their fall risk assessment, allowing for individualized configuration of monitoring parameters. For instance, high-risk patients are monitored for early indicators such as sitting up, attempting to exit the bed, or moving away from the bedside, while low-risk patients are primarily monitored for critical incidents, such as actual falls or prolonged absence from bed during nighttime hours.
This risk-stratified alert framework supports more efficient triaging of responses, enabling staff to prioritize attention for individuals at highest risk while reducing unnecessary alerts and mitigating alarm fatigue.
Risk-based alert sensitivity settings for patient monitoring
Deep learning framework for patient monitoring
The SMART AI Patient Sitter system employs a vision-based deep learning framework designed for real-time detection of bed exits, falls, and staff presence, utilizing standard optical sensors within hospital environments. For detecting bed exits and falls, the system analyzes video frames captured by ceiling or wall-mounted sensors focused on the patient’s bedside area. Instead of relying on pose estimation, a ResNet-based convolutional neural network (CNN) is used to extract spatial features from each frame. This model identifies behavioral patterns such as lying down, sitting at the edge of the bed, or moving away from the bed and classifies the corresponding frame accordingly.
To detect the presence of staff at the bedside, the system incorporates a You Only Look Once (YOLO)-based object detection model trained to recognize the staff through features such as uniforms or contextual visual indicators. This functionality enables automatic cancellation of alerts when staff are present and supports passive logging of response times, thus eliminating the need for manual input.
Notably, the system avoids the use of resource-intensive architectures such as recurrent neural networks (RNNs) or long short-term memory (LSTM) models for temporal analysis. These were excluded due to their high computational and memory demands, which could increase operational costs and hinder scalability. Instead, a custom event logic engine integrates the CNN’s frame-level outputs with time-based heuristics to detect high-risk patterns, such as approaching the bed edge or initiating bed departure. This combination of deep CNN-based spatial analysis and lightweight temporal logic enables efficient, accurate, and scalable continuous monitoring and supporting timely alerts while maintaining low hardware requirements.
Study design and data collection
The study was conducted from January to December 2024, with continuous data collection on falls identified by the SMART AI Patient Sitter system. The system displayed real-time patient status and fall risk, functioning according to its intended use. Its alert panel provided various notifications regarding the patient’s condition, with alert colors changing based on priority levels. When an incident or anomaly was detected, the AI server promptly alerted the ASUHSJ observation counter for immediate response.
The investigators involved in the study were clinical staff who were part of the hospital’s regular healthcare team. They continued performing their routine clinical duties throughout the study and were not employed specifically for research purposes. Their responsibilities included documenting fall-related incidents and contributing relevant clinical observations during the course of patient care.
During the signing of consent, patients were informed by the investigators that they would be monitored by AI and that a blurred video would appear at the observation counter when an alert was triggered. Once an alert was activated, the system began counting and awaited the investigator’s arrival in the room to provide assistance. When the investigator arrived and was detected by the system through uniform recognition, the system automatically dismissed the alert and recorded the response time. The interaction was solely between the system and the investigators, without direct engagement with the patients. The system at the ASUHSJ observation counter functioned only as a tool to notify investigators, ensuring timely intervention to prevent falls. The device was activated by an investigator at the counter only after the patient had given consent, initiating fall monitoring for that patient.
Several user training sessions were conducted by the sponsor to familiarize investigators with the system. Investigators were informed that their presence at the patient’s bedside would be tracked through uniform recognition, without the use of personal identifiers or clear facial images. When a subject was discharged from the ward, the investigators was required to check the patient out of the system at the observation counter, with all actions being logged. If a new patient occupied the same bed and required AI monitoring, the investigator had to perform a new check-in with the updated patient details.
AI monitoring was deactivated when the investigator turned off monitoring through the control panel at the investigator counter. After deactivation, all monitoring, alert triggering, and recording ceased. Patients who did not provide consent were not checked into the system, ensuring that no monitoring or alerts were activated for those patients.
Inclusion criteria and exclusion criteria
Stroke patients aged 18 and above who were admitted to ASUHSJ and agreed to participate in the study, either by themselves or through their legally authorized representative (LAR), were included. Patients or LARs who did not provide consent were excluded from the study. AI monitoring was not conducted on patients who were unwilling to participate. In cases where patients were unable to provide consent themselves, their LARs were approached for consent. However, if a patient later regained consciousness and chose not to participate, the investigator can check the patient out of the system.
Sample size
All stroke patients admitted to ASUHSJ from January till December 2024.
Statistical analysis
Continuous variables were summarized using descriptive statistics, including mean, median, standard deviation, minimum, and maximum values. All statistical analyses were calculated using SPSS (version 23; SPSS, Inc., Chicago, IL) statistical software.