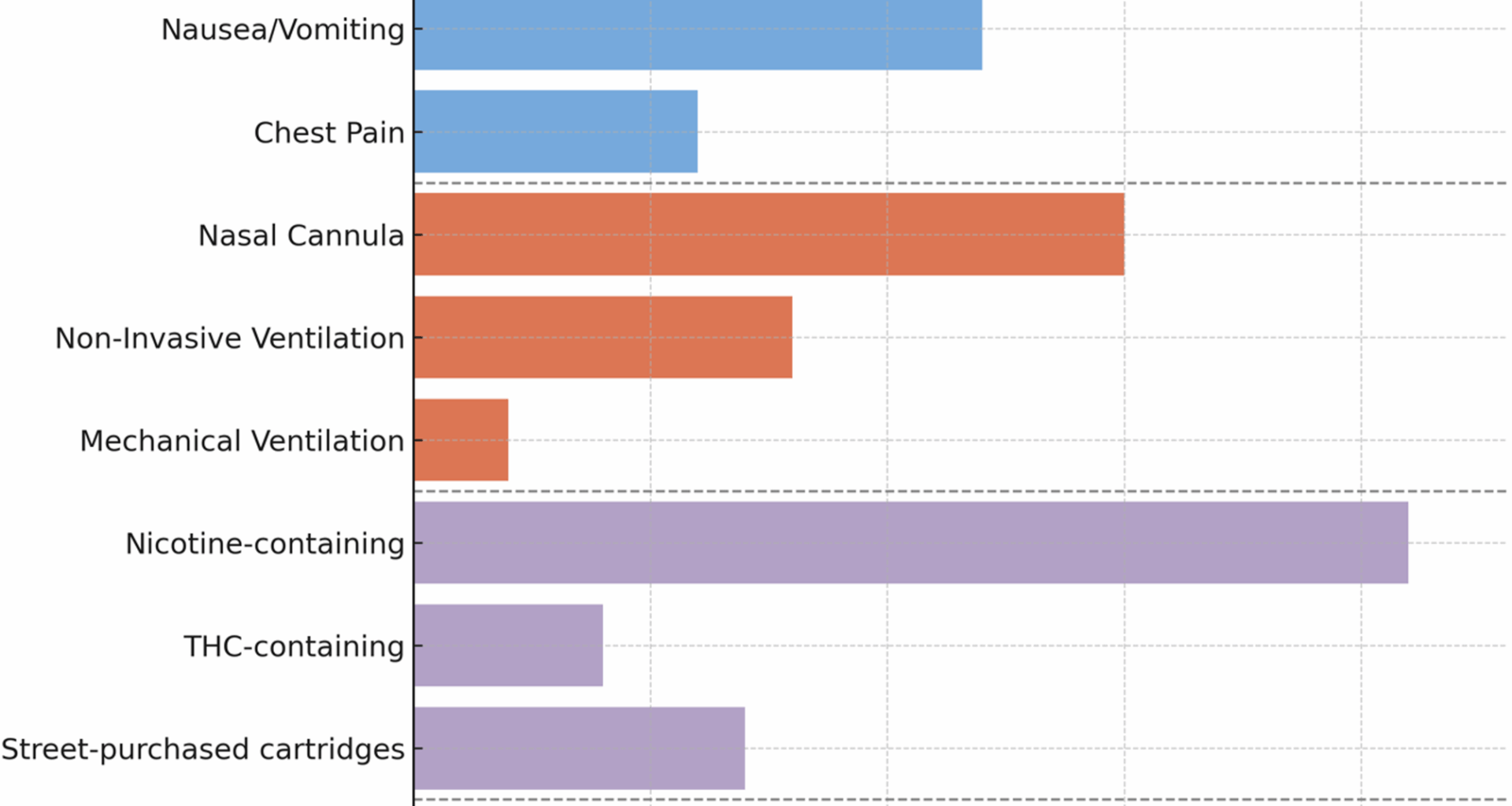
We identified 25 patients who met CDC criteria for EVALI and were admitted to Fundación Santa Fe de Bogotá between January 2020 and July 2024. The mean age was 30 years (range: 18–45), and 80% of the patients were male. Baseline demographic, clinical, and diagnostic characteristics are summarized in Table 1. The median duration of symptoms prior to hospital presentation was 6 days (IQR: 4–9). Most patients (72%, n = 18) reported exclusive use of e-cigarettes without concurrent combustible tobacco, while 28% (n = 7) had a history of dual use. Among those using vaping products, 84% (n = 21) reported nicotine-based liquids, and 16% (n = 4) reported products containing THC. Seven patients (28%) obtained their cartridges from informal street vendors, often lacking clear labeling or composition data. Figure 1 illustrates the distribution of vaping product types and hospital admission settings.
Table 1 Demographic, Clinical, Imaging, and treatment characteristics of patients with EVALIFig. 1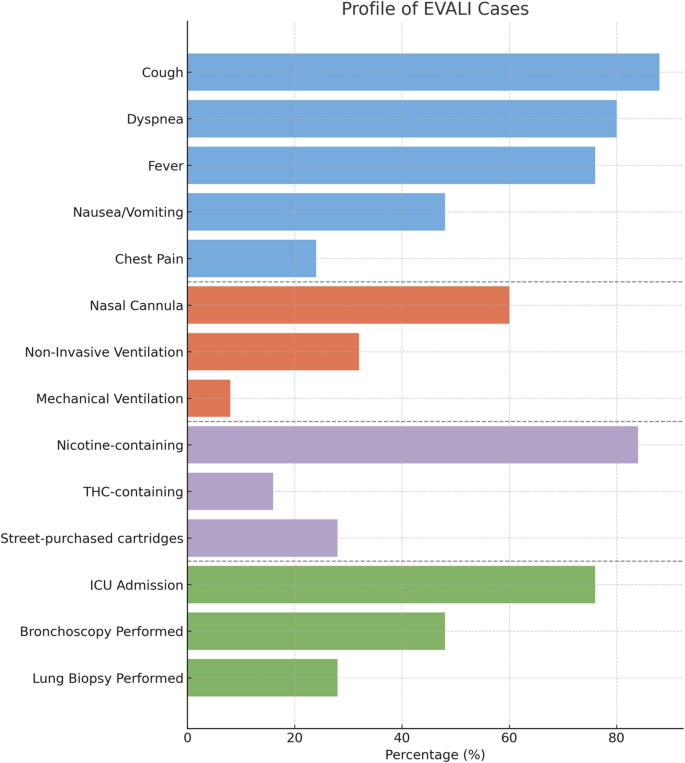
Summary of clinical symptoms, respiratory support, vaping product characteristics, and hospital course among 25 patients diagnosed with EVALI at Fundación Santa Fe de Bogotá, a tertiary academic hospital in Colombia, between January 2020 and July 2024. Data were collected retrospectively. Categories are grouped into four sections: symptoms (blue), respiratory support required (orange), vaping product characteristics (purple), and hospital course and invasive procedures (green). Percentages reflect the proportion of the total cohort. This figure is designed to be interpreted independently and provides a compact summary of patient characteristics and clinical course
The most commonly reported symptoms were cough (88%, n = 22), dyspnea (80%, n = 20), and fever (76%, n = 19), with a median recorded temperature of 38.3 °C. Gastrointestinal symptoms were present in 48% (n = 12), including nausea (36%, n = 9), vomiting (28%, n = 7), and diarrhea (12%, n = 3). Chest pain was reported in 24% (n = 6), and fatigue in 40% (n = 10). Oxygen desaturation on presentation (SpO₂ < 92% on room air) was noted in 68% (n = 17). Laboratory findings revealed leukocytosis (WBC > 11,000/mm³) in 68% of patients, with a median white blood cell count of 13,200/mm³. C-reactive protein was elevated (> 10 mg/L) in 84% (n = 21), with a median value of 78 mg/L (IQR: 54–120). Lactate dehydrogenase (LDH) was elevated in 60% (n = 15), and 3 patients had transient elevation of liver transaminases. HIV and influenza testing were negative in all cases; two patients had low-positive cytomegalovirus (CMV) PCR titers but without organ involvement.
Chest CT imaging revealed bilateral ground-glass opacities in 88% of patients (n = 22), with peripheral distribution and subpleural sparing observed in 72% (n = 18). Additional findings included interlobular septal thickening (44%, n = 11), consolidation (28%, n = 7), and mild pleural effusion in 12% (n = 3). No pulmonary emboli were identified. In one patient, a CT pulmonary angiogram was performed due to suspected embolism and was negative.
Oxygen support was required in 100% of cases. Fifteen patients (60%) were managed with nasal cannula (median FiO₂ 30%), 8 patients (32%) required non-invasive ventilation (NIV), and 2 patients (8%) progressed to invasive mechanical ventilation. High-flow nasal cannula (HFNC) was used in 4 cases (16%) as an intermediate step. The median oxygenation index (PaO₂/FiO₂) among patients requiring ventilatory support was 190 (IQR: 140–230). The frequency of presenting symptoms and respiratory support modalities is shown in Fig. 1.
Bronchoscopy with bronchoalveolar lavage (BAL) was performed in 12 patients (48%), yielding negative results for bacterial, fungal, and mycobacterial cultures. Cytology of BAL fluid demonstrated lipid-laden macrophages in 5 patients (42% of those sampled). Seven patients (28%) underwent lung biopsy: four via transbronchial biopsy and three via surgical wedge resection. Histopathological analysis revealed organizing pneumonia (n = 4), diffuse alveolar damage (n = 2), and eosinophilic pneumonitis (n = 1).
All patients received systemic corticosteroids, initiated with intravenous methylprednisolone (median initial dose: 1 mg/kg/day), followed by tapering oral prednisone. Duration of steroid therapy ranged from 7 to 21 days. Empiric antibiotics were initiated in 68% (n = 17), but discontinued in 12 patients after exclusion of infection. No patients required extracorporeal membrane oxygenation (ECMO).
Nineteen patients (76%) were admitted to the ICU, with a median ICU stay of 4 days (IQR: 2–6). The total median length of hospital stay was 8 days (IQR: 6–11). All patients survived to hospital discharge. On follow-up imaging at 1–3 months, radiologic improvement was observed in 98% of patients (n = 24), including complete resolution in 80% (n = 20), and persistent mild ground-glass opacities without functional impairment in 20% (n = 5). One patient was lost to imaging follow-up.