DuBois LZ, Kaiser Trujillo A, McCarthy MM. Sex and gender: toward transforming scientific practice. Cham: Springer Nature; 2025. https://doi.org/10.1007/978-3-031-91371-6.
European Commission. Gender in EU research and innovation. Brussels: European Research Executive Agency; 2025 [cited 2025 May 25]. Available from: https://rea.ec.europa.eu/gender-eu-research-and-innovation_en
World Health Organization. Gender and COVID-19: advocacy brief [Internet]. Geneva: WHO. 2020 [cited 2025 Apr 28]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Advocacy_brief-Gender-2020.1
Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Mayo Clin Proc. 2020;95(8):1613–20. https://doi.org/10.1016/j.mayocp.2020.05.014.
Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20:7:442–7. https://doi.org/10.1038/s41577-020-0348-8.
Vahidy FS, Pan AP, Ahnstedt H, Munshi Y, Choi HA, Tiruneh Y, et al. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS ONE. 2021;16:1e0245556. https://doi.org/10.1371/journal.pone.0245556.
Quaresima V, Scarpazza C, Sottini A, Fiorini C, Signorini S, Delmonte OM, et al. Sex differences in a cohort of COVID-19 Italian patients hospitalized during the first and second pandemic waves. Biol Sex Differ. 2021;12:1–11. https://doi.org/10.1186/s13293-021-00386-z.
Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11:16317. https://doi.org/10.1038/s41467-020-19741-6.
Ahmed SB, Dumanski SM. Sex, gender and COVID-19: a call to action. Can J Public Health. 2020;111:6:980–3. https://doi.org/10.17269/s41997-020-00417-z.
Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395:10227. https://doi.org/10.1016/S0140-6736(20)30526-2.
Klein SL, Dhakal S, Ursin RL, Deshpande S, Sandberg K, Mauvais-Jarvis F. Biological sex impacts COVID-19 outcomes. PLoS Pathog. 2020;16(6):6e1008570. https://doi.org/10.1371/journal.ppat.1008570.
Global Health 50/50. Sex-disaggregated COVID-19 data tracker. 2025 [cited 2025 Apr 30]. Available from: https://globalhealth5050.org/the-sex-gender-and-covid-19-project/
Hawkes S, Buse K. COVID-19 and the gendered markets of people and products: explaining inequalities in infections and deaths. Can J Dev Stud. 2021;42:1–2. https://doi.org/10.1080/02255189.2020.1824894.
Hawkes S, Pantazis A, Purdie A, Gautam A, Kiwuwa-Muyingo S, Buse K, et al. Sex-disaggregated data matters: tracking the impact of COVID-19 on the health of women and men. Econ Polit. 2022;39(1):55–73. https://doi.org/10.1007/s40888-021-00254-4.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:10223507. https://doi.org/10.1016/S0140-6736(20)30211-7.
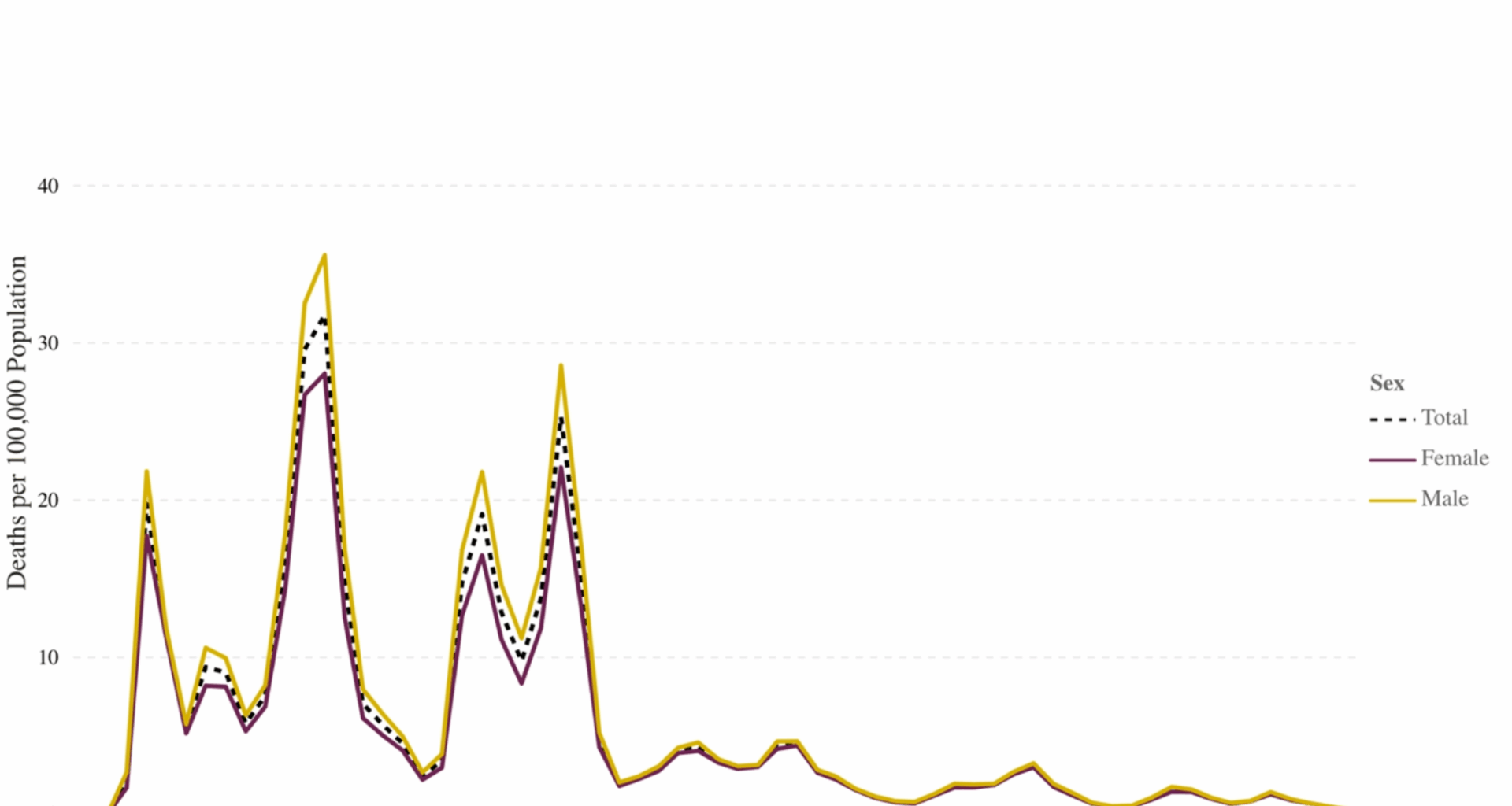
Akter S. The gender gap in COVID-19 mortality in the United States. Fem Econ. 2021;27(1–2):30–47. https://doi.org/10.1080/13545701.2020.1829673.
Green MS, Nitzan D, Schwartz N, Niv Y, Peer V. Sex differences in the case-fatality rates for COVID-19—a comparison of the age-related differences and consistency over seven countries. PLoS ONE. 2021;16:4e0250523. https://doi.org/10.1371/journal.pone.0250523.
Venegas-Ramírez J, Mendoza-Cano O, Trujillo X, Huerta M, Ríos-Silva M, Lugo-Radillo A, et al. Sex differences in pneumonia risk during COVID-19 in Mexico. Sci Rep. 2024;14:127962. https://doi.org/10.1038/s41598-024-78200-0.
Centers for Disease Control and Prevention (CDC). COVID data tracker. 2025 [cited 2025 June 21]. Available from: https://covid.cdc.gov/covid-data-tracker
Danielsen AC, Lee KM, Boulicault M, Rushovich T, Gompers A, Tarrant A, et al. Sex disparities in COVID-19 outcomes in the United States: quantifying and contextualizing variation. Soc Sci Med. 2022;294:114716. https://doi.org/10.1016/j.socscimed.2022.114716.
Garcia J, Torres C, Barbieri M, Camarda C-G, Cambois E, Caporali A, et al. Differences in COVID-19 mortality: implications of imperfect and diverse data collection systems. Population. 2021;76(1):35–72. https://doi.org/10.3917/popu.2101.0035.
Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11:1–13. https://doi.org/10.1186/s13293-020-00304-9.
Premraj L, Weaver NA, Ahmad SA, White N, Whitman G, Arora R, et al. Sex differences in the outcome of critically ill patients with COVID-19-an international multicenter critical care consortium study. Heart Lung. 2024;68:373–80. https://doi.org/10.1016/j.hrtlng.2024.09.001.
Kharroubi SA, Diab-El-Harake M. Sex differences in COVID-19 mortality: a large US-based cohort study (2020–2022). AIMS Public Health. 2024;11:3886. https://doi.org/10.3934/publichealth.2024045.
DiMarco M, Zhao H, Boulicault M, Richardson SS. Why sex as a biological variable conflicts with precision medicine initiatives. Cell Rep Med. 2022;3:4100550. https://doi.org/10.1016/j.xcrm.2022.100550.
Sanchis-Segura C, Wilcox RR. From means to meaning in the study of sex/gender differences and similarities. Front Neuroendocrinol. 2024;73:101133. https://doi.org/10.1016/j.yfrne.2024.101133.
Pradhan A, Olsson P-E. Sex differences in severity and mortality from COVID-19: are males more vulnerable? Biol Sex Differ. 2020;11:153. https://doi.org/10.1186/s13293-020-00330-7.
Capuano A, Rossi F, Paolisso G. Covid-19 kills more men than women: an overview of possible reasons. Front Cardiovasc Med. 2020;7:131. https://doi.org/10.3389/fcvm.2020.00131.
Alwani M, Yassin A, Al-Zoubi RM, Aboumarzouk OM, Nettleship J, Kelly D, et al. Sex‐based differences in severity and mortality in COVID‐19. Rev Med Virol. 2021;31:6e2223. https://doi.org/10.1002/rmv.2223.
Gompers A, Bruch JD, Richardson SS. Are COVID-19 case fatality rates a reliable measure of sex disparities? Womens Health Issues. 2021;32:287. https://doi.org/10.1016/j.whi.2021.11.007.
Eliot L, Richardson SS. Sex in context: limitations of animal studies for addressing human sex/gender neurobehavioral health disparities. J Neurosci. 2016;36(47):11823–30. https://doi.org/10.1523/JNEUROSCI.1391-16.2016.
Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198(10):4046–53. https://doi.org/10.4049/jimmunol.1601896.
Dhakal S, Ruiz-Bedoya CA, Zhou R, Creisher PS, Villano JS, Littlefield K, et al. Sex differences in lung imaging and SARS-CoV-2 antibody responses in a COVID-19 golden Syrian hamster model. mBio. 2021;12:e400974–21. https://doi.org/10.1128/mbio.00974-21.
Onodera Y, Liang J, Li Y, Griffin B, Thanabalasingam T, Lu C, et al. Inhalation of ACE2 as a therapeutic target on sex-bias differences in SARS-CoV-2 infection and variant of concern. iScience. 2023. https://doi.org/10.1016/j.isci.2023.107470.
Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588:7837315–20. https://doi.org/10.1038/s41586-020-2700-3.
Park MD. Sex differences in immune responses in COVID-19. Nat Rev Immunol. 2020;20:8461. https://doi.org/10.1038/s41577-020-0378-2.
Takahashi T, Iwasaki A. Sex differences in immune responses. Science. 2021;371:6527. https://doi.org/10.1126/science.abe7199.
Shattuck-Heidorn H, Danielsen AC, Gompers A, Bruch JD, Zhao H, Boulicault M, et al. A finding of sex similarities rather than differences in COVID-19 outcomes. Nature. 2021;597:7877:E7–9. https://doi.org/10.1038/s41586-021-03644-7.
Sharma G, Volgman AS, Michos ED. Sex differences in mortality from COVID-19 pandemic: are men vulnerable and women protected? Case Rep. 2020;2:9:1407–10. https://doi.org/10.1016/j.jaccas.2020.04.027.
Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res. 2020;116:142197–206. https://doi.org/10.1093/cvr/cvaa284.
Pape M, Miyagi M, Ritz S, Boulicault A, Richardson M, Maney SS. Sex contextualism in laboratory research: enhancing rigor and precision in the study of sex-related variables. Cell. 2024;187:6:1316–26. https://doi.org/10.1016/j.cell.2024.02.008.
Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8:9737–44. https://doi.org/10.1038/nri2394.
Wilkinson NM, Chen H-C, Lechner MG, Su MA. Sex differences in immunity. Annu Rev Immunol. 2022;40:1:75–94. https://doi.org/10.1146/annurev-immunol-101320-125133.
Tukiainen T, Villani A-C, Yen A, Rivas MA, Marshall JL, Satija R, et al. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:7675:244–8. https://doi.org/10.1038/nature24265.
Forsyth KS, Jiwrajka N, Lovell CD, Toothacre NE, Anguera MC. The connexion between sex and immune responses. Nat Rev Immunol. 2024;24(7):487–502. https://doi.org/10.1038/s41577-024-00996-9.
Schurz H, Salie M, Tromp G, Hoal EG, Kinnear CJ, Möller M. The X chromosome and sex-specific effects in infectious disease susceptibility. Hum Genomics. 2019;13:1–12. https://doi.org/10.1186/s40246-018-0185-z.
Behzadi P, Chandran D, Chakraborty C, Bhattacharya M, Saikumar G, Dhama K, et al. The dual role of toll-like receptors in COVID-19: balancing protective immunity and Immunopathogenesis. Int J Biol Macromol. 2024;137836. https://doi.org/10.1016/j.ijbiomac.2024.137836.
Zhang Q, Bastard P, Cobat A, Casanova J-L. Human genetic and immunological determinants of critical COVID-19 pneumonia. Nature. 2022;603(7902):587–98. https://doi.org/10.1038/s41586-022-04447-0.
Boos J, van der Made CI, Ramakrishnan G, Coughlan E, Asselta R, Löscher B-S, et al. Stratified analyses refine association between TLR7 rare variants and severe COVID-19. Human Genetics and Genomics Advances. 2024;5:4. https://doi.org/10.1016/j.xhgg.2024.100323.
Klein SL, Marriott I, Fish EN. Sex-based differences in immune function and responses to vaccination. Trans R Soc Trop Med Hyg. 2015;109(1):9–15. https://doi.org/10.1093/trstmh/tru167.
Foresta C, Rocca M, Di Nisio A. Gender susceptibility to COVID-19: a review of the putative role of sex hormones and X chromosome. J Endocrinol Invest. 2021;44:951–6. https://doi.org/10.1007/s40618-020-01383-6.
Pairo-Castineira E, Clohisey S, Klaric L, Bretherick AD, Rawlik K, Pasko D, et al. Genetic mechanisms of critical illness in COVID-19. Nature. 2021;591:784892–8. https://doi.org/10.1038/s41586-020-03065-y.
Brandi ML. Are sex hormones promising candidates to explain sex disparities in the COVID-19 pandemic? Rev Endocr Metab Disord. 2022;23(2):171–83. https://doi.org/10.1007/s11154-021-09692-8
COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19. Nature. 2021;600:7889. https://doi.org/10.1038/s41586-021-03767-x.
Saengsiwaritt W, Jittikoon J, Chaikledkaew U, Udomsinprasert W. Genetic polymorphisms of ACE1, ACE2, and TMPRSS2 associated with COVID-19 severity: A systematic review with meta‐analysis. Rev Med Virol. 2022;32:4e2323. https://doi.org/10.1002/rmv.2323.
Pairo-Castineira E, Rawlik K, Bretherick AD, Qi T, Wu Y, Nassiri I, et al. GWAS and meta-analysis identifies 49 genetic variants underlying critical COVID-19. Nature. 2023;617:7962:764–8. https://doi.org/10.1038/s41586-023-06034-3.
Cobat A, Zhang Q, Effort CHG, Abel L, Casanova J-L, Fellay J. Human genomics of COVID-19 pneumonia: contributions of rare and common variants. Annu Rev Biomed Data Sci. 2023;6:1465–86. https://doi.org/10.1146/annurev-biodatasci-020222-021705.
Pérez-Jurado LA, Cáceres A, Balagué-Dobón L, Esko T, López de Heredia M, Quintela I, et al. Clonal chromosomal mosaicism and loss of chromosome Y in elderly men increase vulnerability for SARS-CoV-2. Commun Biol. 2024;7:1202. https://doi.org/10.1038/s42003-024-05805-6.
Bruhn-Olszewska B, Davies H, Sarkisyan D, Juhas U, Rychlicka-Buniowska E, Wójcik M, et al. Loss of Y in leukocytes as a risk factor for critical COVID-19 in men. Genome Med. 2022;14:1139. https://doi.org/10.1186/s13073-022-01144-5.
Bruhn-Olszewska B, Markljung E, Rychlicka-Buniowska E, Sarkisyan D, Filipowicz N, Dumanski JP. The effects of loss of Y chromosome on male health. Nat Rev Genet. 2025. https://doi.org/10.1038/s41576-024-00805-y.
D’Onofrio V, Sékaly RP. The immune–endocrine interplay in sex differential responses to viral infection and COVID-19. Trends Immunol. 2024;45:12:943 – 58. https://doi.org/10.1016/j.it.2024.10.004.
Harvey BJ, McElvaney NG. Sex differences in airway disease: Estrogen and airway surface liquid dynamics. Biol Sex Differ. 2024;15(1):56. https://doi.org/10.1186/s13293-024-00633-z
Frederiksen H, Johannsen TH, Andersen SE, Albrethsen J, Landersoe SK, Petersen JH, et al. Sex-specific Estrogen levels and reference intervals from infancy to late adulthood determined by LC-MS/MS. J Clin Endocrinol Metab. 2020;105:3754–68. https://doi.org/10.1210/clinem/dgz196.
Stanton SJ, Schultheiss OC. Basal and dynamic relationships between implicit power motivation and estradiol in women. Horm Behav. 2007;52(5):571. https://doi.org/10.1016/j.yhbeh.2007.07.002.
Fan C, Wu Y, Rui X, Yang Y, Ling C, Liu S, et al. Animal models for COVID-19: advances, gaps and perspectives. Signal Transduct Target Ther. 2022;7:1220. https://doi.org/10.1038/s41392-022-01087-8.
Ding T, Zhang J, Wang T, Cui P, Chen Z, Jiang J, et al. Potential influence of menstrual status and sex hormones on female severe acute respiratory syndrome coronavirus 2 infection: a cross-sectional multicenter study in Wuhan, China. Clin Infect Dis. 2021;72:e9240–8. https://doi.org/10.1093/cid/ciaa1022.
Wang X-W, Hu H, Xu Z-Y, Zhang G-K, Yu Q-H, Yang H-L, et al. Association of menopausal status with COVID-19 outcomes: a propensity score matching analysis. Biol Sex Differ. 2021;12(1):1–8. https://doi.org/10.1186/s13293-021-00363-6.
Cinislioglu AE, Cinislioglu N, Demirdogen SO, Sam E, Akkas F, Altay MS, et al. The relationship of serum testosterone levels with the clinical course and prognosis of COVID-19 disease in male patients: a prospective study. Andrology. 2022;10:1. https://doi.org/10.1111/andr.13081.
Lott N, Gebhard CE, Bengs S, Haider A, Kuster GM, Regitz-Zagrosek V, et al. Sex hormones in SARS-CoV-2 susceptibility: key players or confounders? Nat Rev Endocrinol. 2023;19:4217–31. https://doi.org/10.1038/s41574-022-00780-6.
Viveiros A, Rasmuson J, Vu J, Mulvagh SL, Yip CY, Norris CM, et al. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320(1):H296–304. https://doi.org/10.1152/ajpheart.00755.2020.
Solis O, Beccari AR, Iaconis D, Talarico C, Ruiz-Bedoya CA, Nwachukwu JC, et al. The SARS-CoV-2 Spike protein binds and modulates Estrogen receptors. Sci Adv. 2022;8:48eadd4150. https://doi.org/10.1126/sciadv.add4150.
Qiao Y, Wang X-M, Mannan R, Pitchiaya S, Zhang Y, Wotring JW, et al. Targeting transcriptional regulation of SARS-CoV-2 entry factors ACE2 and TMPRSS2. Proc Natl Acad Sci U S A. 2021;118:1e2021450118. https://doi.org/10.1073/pnas.2021450118.
Stelzig KE, Canepa-Escaro F, Schiliro M, Berdnikovs S, Prakash Y, Chiarella SE. Estrogen regulates the expression of SARS-CoV-2 receptor ACE2 in differentiated airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2020;318(6):L1280–1. https://doi.org/10.1152/ajplung.00153.2020.
Chappell MC. Renin-angiotensin system and sex differences in COVID-19: a critical assessment. Circ Res. 2023;132(10):1320–37. https://doi.org/10.1161/CIRCRESAHA.123.321883.
Wettstein L, Kirchhoff F, Münch J. The transmembrane protease TMPRSS2 as a therapeutic target for COVID-19 treatment. Int J Mol Sci. 2022;23(3):31351. https://doi.org/10.3390/ijms23031351.
Mohan EC, Savarraj JP, Colpo GD, Morales D, Finger CE, McAlister A, et al. Aromatase, testosterone, TMPRSS2: determinants of COVID-19 severity. Biol Sex Differ. 2024;15:184. https://doi.org/10.1186/s13293-024-00658-4.
Jacobsen H, Klein SL. Sex differences in immunity to viral infections. Front Immunol. 2021;12:720952. https://doi.org/10.3389/fimmu.2021.720952.
Qi S, Ngwa C, Morales Scheihing DA, Al Mamun A, Ahnstedt HW, Finger CE, et al. Sex differences in the immune response to acute COVID-19 respiratory tract infection. Biol Sex Differ. 2021;12(1):1–10. https://doi.org/10.1186/s13293-021-00410-2.
Agrawal S, Salazar J, Tran TM, Agrawal A. Sex-related differences in innate and adaptive immune responses to SARS-CoV-2. Front Immunol. 2021;12:739757. https://doi.org/10.3389/fimmu.2021.739757.
Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021;27:1. https://doi.org/10.1038/s41591-020-01202-8.
Calabrò A, Accardi G, Aiello A, Caruso C, Candore G. Sex and gender affect immune aging. Front Aging. 2023;4:1272118. https://doi.org/10.3389/fragi.2023.1272118.
Ren X, Wen W, Fan X, Hou W, Su B, Cai P, et al. COVID-19 immune features revealed by a large-scale single-cell transcriptome atlas. Cell. 2021;184(7):1895 –913. e19. https://doi.org/10.1016/j.cell.2021.01.053
Gygi JP, Maguire C, Patel RK, Shinde P, Konstorum A, Shannon CP, et al. Integrated longitudinal multiomics study identifies immune programs associated with acute COVID-19 severity and mortality. J Clin Invest. 2024. https://doi.org/10.1172/JCI176640.
Escarcega RD, Honarpisheh P, Colpo GD, Ahnstedt HW, Couture L, Juneja S, et al. Sex differences in global metabolomic profiles of COVID-19 patients. Cell Death Dis. 2022;13:5461. https://doi.org/10.1038/s41419-022-04861-2.
Krieger N. Genders, sexes, and health: what are the connections—and why does it matter? Int J Epidemiol. 2003;32(4):652–7. https://doi.org/10.1093/ije/dyg156.
Richardson SS. Sex contextualism. Philosophy, Theory, and Practice in Biology. 2022;14:2. https://doi.org/10.3998/ptpbio.2096.
Brewis A, Currah P, DuBois LZ, Greaves L, Hoppe K, Karkazis K, et al. Gender, sex, and their entanglement. In: Springer S, editor. Sex and gender. Cham: Springer; 2025. pp. 241–65. https://doi.org/10.1007/978-3-031-91371-6.
Shattuck-Heidorn H, Reiches MW, Richardson SS. What’s Really Behind the Gender Gap in Covid-19 Deaths? The New York Times. https://www.nytimes.com/2020/06/24/opinion/sex-differences-covid.html (2020).
Bengtsson T, Dribe M, Eriksson B. Social class and excess mortality in Sweden during the 1918 influenza pandemic. Am J Epidemiol. 2018;187(12):2568–76. https://doi.org/10.1093/aje/kwy151.
Yang YM, Hsu CY, Lai CC, Yen MF, Wikramaratna PS, Chen HH, et al. Impact of comorbidity on fatality rate of patients with middle East respiratory syndrome. Sci Rep. 2017;7:111307. https://doi.org/10.1038/s41598-017-10402-1.
Rushovich T, Boulicault M, Chen JT, Danielsen AC, Tarrant A, Richardson SS, et al. Sex disparities in COVID-19 mortality vary across US Racial groups. J Gen Intern Med. 2021;36:61696–701. https://doi.org/10.1007/s11606-021-06699-4.
Raparelli V, Palmieri L, Canevelli M, Pricci F, Unim B, Lo Noce C, et al. Sex differences in clinical phenotype and transitions of care among individuals dying of COVID-19 in Italy. Biol Sex Differ. 2020;11:1–9. https://doi.org/10.1186/s13293-020-00334-3.
Kharroubi SA, Diab-El-Harake M. Sex-differences in COVID-19 diagnosis, risk factors and disease comorbidities: a large US-based cohort study. Front Public Health. 2022;10:1029190. https://doi.org/10.3389/fpubh.2022.1029190.
Yoshida Y, Chu S, Fox S, Zu Y, Lovre D, Denson JL, et al. Sex differences in determinants of COVID-19 severe outcomes – findings from the National COVID cohort collaborative (N3C). BMC Infect Dis. 2022;22:1784. https://doi.org/10.1186/s12879-022-07776-7.
Kilic H, Arguder E, Karalezli A, Unsal E, Guner R, Kayaslan B, et al. Effect of chronic lung diseases on mortality of prevariant COVID-19 pneumonia patients. Front Med Lausanne. 2022;9:957598. https://doi.org/10.3389/fmed.2022.957598.
Peters SA, MacMahon S, Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the UK biobank: comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab. 2021;23:1258–62. https://doi.org/10.1111/dom.14199.
Sudhakar M, Winfred SB, Meiyazhagan G, Venkatachalam DP. Mechanisms contributing to adverse outcomes of COVID-19 in obesity. Mol Cell Biochem. 2022;477:4:1155–93. https://doi.org/10.1007/s11010-022-04356-w.
Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero J-J, DeMeo DL, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396 :565–82. https://doi.org/10.1016/S0140-6736(20)31561-0
Khalil A, Dhingra R, Al-Mulki J, Hassoun M, Alexis N. Questioning the sex-specific differences in the association of smoking on the survival rate of hospitalized COVID-19 patients. PLoS ONE. 2021;16(8):e0255692. https://doi.org/10.1371/journal.pone.0255692.
Lacedonia D, Scioscia G, Santomasi C, Fuso P, Carpagnano GE, Portacci A, et al. Impact of smoking, COPD and comorbidities on the mortality of COVID-19 patients. Sci Rep. 2021;11:119251. https://doi.org/10.1038/s41598-021-98749-4.
Haischer MH, Beilfuss R, Hart MR, Opielinski L, Wrucke D, Zirgaitis G, et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS ONE. 2020;15(10):e0240785. https://doi.org/10.1371/journal.pone.0240785.
Tang CS-k, Wong C-y. Factors influencing the wearing of facemasks to prevent the severe acute respiratory syndrome among adult Chinese in Hong Kong. Prev Med. 2004;39:6:1187–93. https://doi.org/10.1016/j.ypmed.2004.04.032.
Okten IO, Gollwitzer A, Oettingen G. Gender differences in preventing the spread of coronavirus. Behav Sci Policy. 2020;6:2109–22. https://doi.org/10.1177/237946152000600214.
Hearne BN, Niño MD. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: evidence from the COVID impact survey. J Racial Ethn Health Disparities. 2021:1–8. https://doi.org/10.1007/s40615-020-00941-1
Almagro M, Orane-Hutchinson AJUE, Insight. The determinants of the differential exposure to COVID-19 in new York City and their evolution over time. J Urban Econ. 2022;127:103293. https://doi.org/10.1016/j.jue.2020.103293.
Goldman N, Pebley AR, Lee K, Andrasfay T, Pratt B. Racial and ethnic differentials in COVID-19-related job exposures by occupational standing in the US. PLoS ONE. 2021;16(9):e0256085. https://doi.org/10.1371/journal.pone.0256085.
Morgan R, Baker P, Griffith DM, Klein SL, Logie CH, Mwiine AA, et al. Beyond a zero-sum game: how does the impact of COVID-19 vary by gender? Front Sociol. 2021;6:650729. https://doi.org/10.3389/fsoc.2021.650729.
Auderset D, Amiguet M, Clair C, Riou J, Pittet V, Schwarz J, et al. Gender/sex disparities in the COVID-19 cascade from testing to mortality: an intersectional analysis of Swiss surveillance data. Int J Public Health. 2024;69:1607063. https://doi.org/10.3389/ijph.2024.1607063.
Sant Fruchtman C, Fischer FB, Monzón Llamas L, Tavakkoli M, Cobos Muñoz D, Antillon M, Did. COVID-19 policies have the same effect on COVID-19 incidence among women and men? Evidence from Spain and Switzerland. Int J Public Health. 2022;67:1604994. https://doi.org/10.3389/ijph.2022.1604994.
Krieger N. Epidemiology and the people’s health: theory and context. Oxford University Press; 2024.
Vandentorren S, Smaïli S, Chatignoux E, Maurel M, Alleaume C, Neufcourt L, et al. The effect of social deprivation on the dynamic of SARS-CoV-2 infection in france: a population-based analysis. Lancet Public Health. 2022;7:e3240–9. https://doi.org/10.1016/S2468-2667(22)00007-X.
Dehingia N, Raj A. Sex differences in COVID-19 case fatality: do we know enough? Lancet Glob Health. 2021;9(1):e14-e5. https://doi.org/10.1016/S2214-109X(20)30464-2
Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:1137. https://doi.org/10.1016/j.amepre.2020.04.003.
Hawkins RB, Charles EJ, Mehaffey JH. Socio-economic status and COVID-19–related cases and fatalities. Public Health. 2020. https://doi.org/10.1016/j.puhe.2020.09.016. 189:129 – 34.
Wachtler B, Michalski N, Nowossadeck E, Diercke M, Wahrendorf M, Santos-Hövener C, et al. Socioeconomic inequalities and COVID-19 – A review of the current international literature. J Health Monit. 2020;5(Suppl 7):3. https://doi.org/10.25646/7059.
Magesh S, John D, Li WT, Li Y, Mattingly-App A, Jain S, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. https://doi.org/10.1001/jamanetworkopen.2021.34147.
Pal S, Gangu K, Garg I, Shuja H, Bobba A, Chourasia P, et al. Gender and race-based health disparities in COVID-19 outcomes among hospitalized patients in the United States: a retrospective analysis of a national sample. Vaccines. 2022;10:122036. https://doi.org/10.3390/vaccines10122036.
Matthay EC, Duchowny KA, Riley AR, Thomas MD, Chen Y-H, Bibbins-Domingo K, et al. Occupation and educational attainment characteristics associated with COVID-19 mortality by race and ethnicity in California. JAMA Netw Open. 2022;5:4e228406. https://doi.org/10.1001/jamanetworkopen.2022.8406.
Elo IT, Luck A, Stokes AC, Hempstead K, Xie W, Preston SH. Evaluation of age patterns of COVID-19 mortality by race and ethnicity from March 2020 to October 2021 in the US. JAMA Netw Open. 2022;5(5):5e2212686. https://doi.org/10.1001/jamanetworkopen.2022.12686.
Yuan AY, Atanasov V, Barreto N, Franchi L, Whittle J, Weston B, et al. Understanding racial/ethnic disparities in COVID-19 mortality using a novel metric: COVID excess mortality percentage. Am J Epidemiol. 2024;193:6853–62. https://doi.org/10.1093/aje/kwae007.
Islam N, Khunti K, Dambha-Miller H, Kawachi I, Marmot M. COVID-19 mortality: a complex interplay of sex, gender and ethnicity. Eur J Public Health. 2020;30:5. https://doi.org/10.1093/eurpub/ckaa150.
Khalatbari-Soltani S, Cumming RC, Delpierre C, Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health. 2020;74:8. https://doi.org/10.1136/jech-2020-214297.
Hawkes S, Sy EA, Barker G, Baum FE, Buse K, Chang AY, et al. Achieving gender justice for global health equity: the lancet commission on gender and global health. Lancet. 2025;405:104871373–438. https://doi.org/10.1016/S0140-6736(25)00488-X.