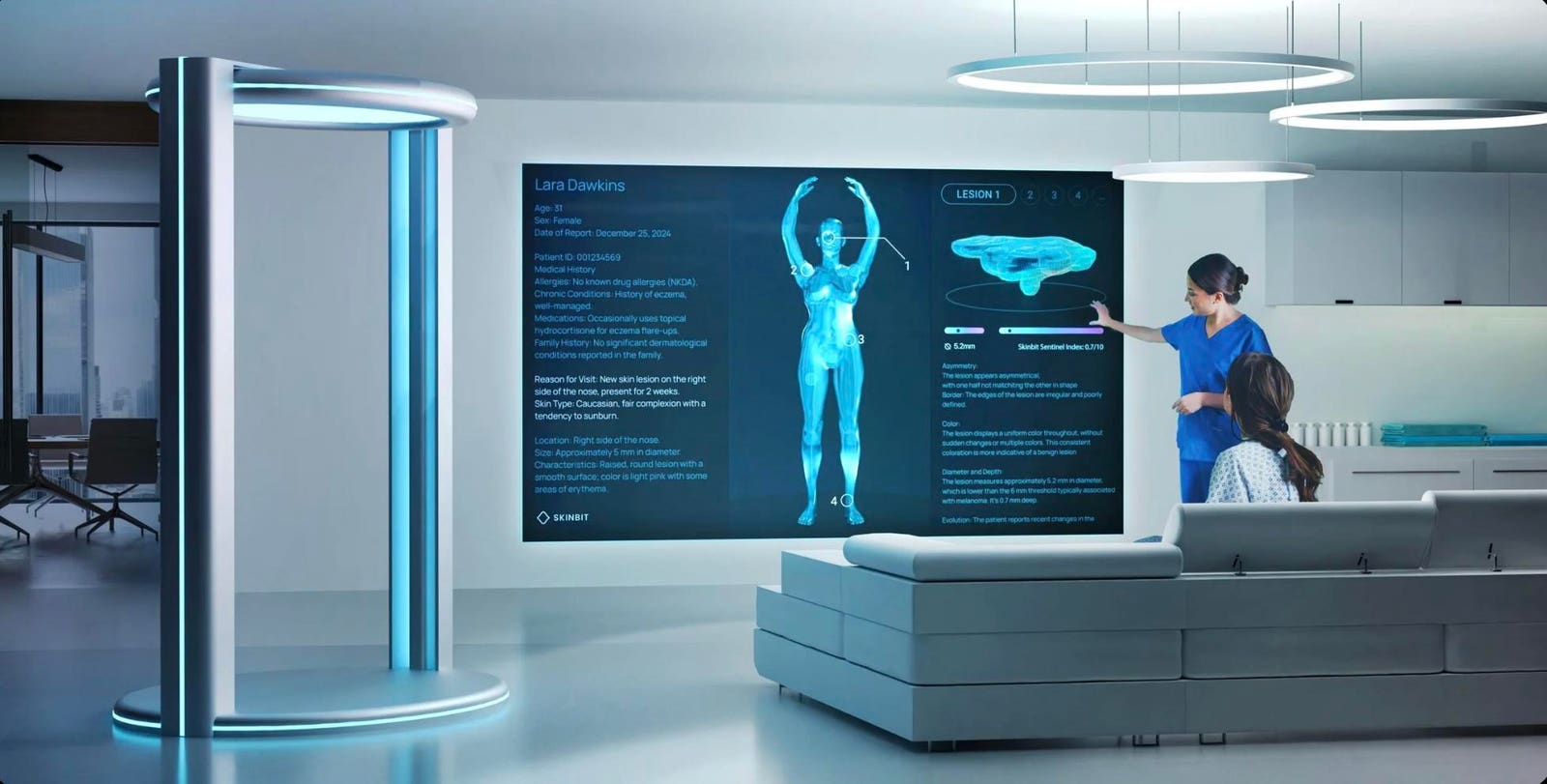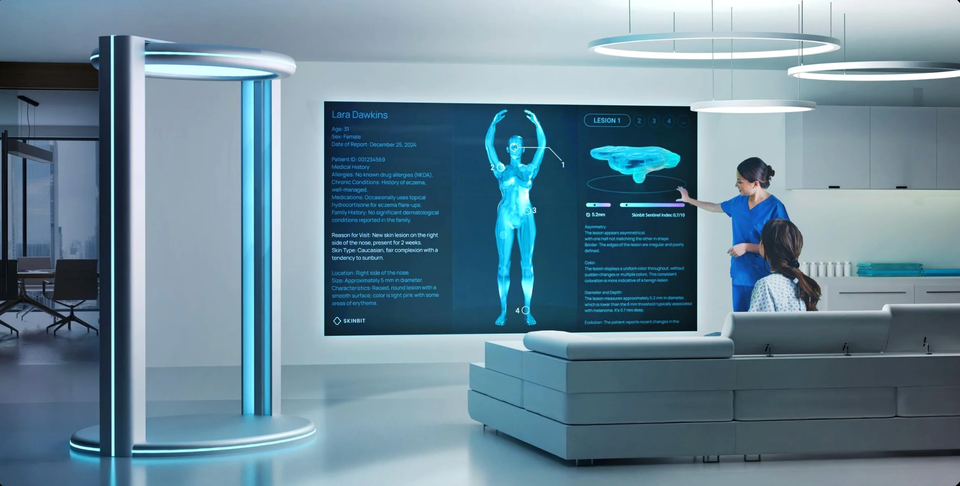
An artist rendering of the Skinbit scanner and scan report.
Skinbit
In 2020, Jonathan Benassaya walked into a dermatologist’s office for a routine skin check—an appointment that took months to secure. The examination lasted barely two minutes. The doctor said he was fine and told him to come back in a year.
But as Benassaya was paying his bill, the doctor happened by and realized that she had forgotten to check beneath his face mask.
There, on his nose, was a dark spot that turned out to be melanoma. But for a stroke of luck, Benassaya reflects, “I would be dead by now.”
Jonathan Benssaya, CEO of Skinbit
Skinbit
That near-miss became the catalyst for SkinBit, an AI-powered total body scanning system Benassaya went on to design to detect skin cancer years before it becomes life-threatening.
Benassaya’s story exemplifies a growing movement of technically sophisticated patients who are channeling their diagnoses into AI systems that address gaps their own doctors couldn’t fill.
The Patient-Innovator Movement
This unique cohort of patients shares common threads: a diagnosis that revealed systemic failures in healthcare delivery, technical skills to build sophisticated AI systems, and the determination to ensure others don’t face the same challenges they endured.
Regina Barzilay, an MIT computer scientist, was diagnosed with breast cancer in 2014 and, in response, developed a deep learning model that analyzes mammography images to predict breast cancer risk up to five years in advance.
Seventeen-year-old Sachchit Balamurugan watched his grandfather die from a rare and aggressive cancer, then spent months developing AI models that combine MRI imaging, transcriptomic data, and convolutional neural networks to detect the disease with over 90 percent accuracy.
And Aaron Babier, a PhD candidate at the University of Toronto, developed AI software that reduces radiation therapy planning time from days to just 20 minutes after his stepmother died from a brain tumor.
What distinguishes these patient-developed systems from institutional AI research is their focus on problems that only become apparent when you’re the patient navigating the system.
CureWise: Creating Your Virtual Medical Advisory Board
Steve Brown, CEO of CureWise
CureWise
Steve Brown spent a year being misdiagnosed before a new medical team finally identified his rare blood cancer. After that diagnosis, he applied two decades of experience in healthcare technology to build CureWise, an AI-powered platform designed to analyze complex medical records and help patients navigate treatment decisions with clearer insight.
When Brown fed the same complete medical history his earlier doctors had already reviewed into CureWise, the system immediately flagged concerning patterns: mild anemia, elevated ferritin, and low immunoglobulins, pointing to immune dysfunction and bone marrow involvement. Within minutes, it surfaced serum-free light chains testing and a bone marrow biopsy, tests that had never been raised during the year his symptoms were being explained away.
“The AI immediately put the pieces together,” Brown explains. “If I had known about that test, I would have asked for it a year earlier.”
Brown expanded his approach, creating a panel of specialized AI agents, large-language models that behave as an oncologist, a gastroenterologist, a hematologist, and an emergency room doctor, each with distinct personas and perspectives. A more general model, which he calls “Hippocrates,” consolidates the various recommendations through what he describes as a “chain of debate,” where agents based on multiple AI models (OpenAI, Anthropic, Google, Mistral, and xAI) argue with each other from different angles to explore as many pathways through the knowledge as possible.
The collaboration between Brown’s human oncologists and his AI-powered insights fundamentally reshaped his treatment. Instead of “standard of care,” the accepted treatment that doctors follow for a particular disease, he’s now on an off-label combination of drugs that has produced what he calls “almost a miraculous response,” with his key cancer marker returning to normal range.
“If you don’t know what to ask for, you’re just going to get standard of care,” Brown explains, adding that response rates for standard treatment can be under 30% for some cancers. “You might spend very valuable time going down a path that’s not going to work when there might be things already today that are better for you, but you’re not going to know about them unless you ask.”
Brown discovered the importance of this comprehensive approach when his cancer marker plateaued unexpectedly. His AI analysis revealed he wasn’t taking his medication with sufficient fat for proper absorption. When a friend mentioned his brother died not from multiple myeloma but from an infection during treatment, Brown asked the AI about defensive measures and learned about prophylactic antibodies through monthly infusions. His doctors were happy to provide the infusions, but hadn’t suggested them.
“You might not get the care you need unless you’re in a position to advocate for it,” Brown emphasizes. “I’m on a bunch of things that I never would have gotten if I didn’t know about them and advocate for them.”
CureWise is now entering private beta for other cancer patients, offering them the virtual medical advisory board Brown built for himself.
SkinBit: Building the Triage Infrastructure Dermatology Lacks
Benassaya, who previously founded the music streaming service Deezer was stunned by the technological gap he encountered in dermatology. “We live in a world of MRIs, robotic surgery, and AI diagnostics,” he said in a telephone interview. “Yet skin cancer, the most common cancer with 50 percent-plus of diagnoses worldwide, is still detected primarily through visual inspection methods from the 1970s.”
Skin cancer affects 5.4 million Americans annually, yet there are only 12,000 dermatologists in the United States. That’s why it takes months to get an appointment and why visits are so brief, Benassaya says.
With an aging population and more and more people with skin cancer, the capacity of dermatology is barely reaching 50 percent of what the US needs.
SkinBit’s solution creates a digital twin of your entire body in under 60 seconds using 16 high-resolution cameras arranged in an elliptical ring. The system combines the images so every pixel is in focus, even in complex areas like the creases of the nose or beneath the eyes. The resulting 3D model has a resolution fine enough to visualize individual blood vessels and skin texture patterns invisible to the naked eye.
Computer vision algorithms trained on over 50,000 clinical data points segment and classify every lesion, assigning risk scores for each. Benassaya claims the system achieves over 90 percent accuracy in detecting skin cancer.
He envisions scanners in dermatology clinics, but also in other settings from general practitioners’ offices to medical spas, pharmacies, even gyms and wellness clinics.
“We can transform skin cancer care and ensure that no one dies from a cancer that could have been detected early,” he says.
The Broader Impact of Patient-Driven Innovation
Of course, AI should assist, not replace, clinical judgment. Barzilay’s MIRAI has undergone extensive clinical validation. SkinBit’s scans are reviewed by board-certified dermatologists. And Brown’s CureWise is designed to help patients ask better questions and advocate more effectively, not to bypass their oncology teams.
But these patient-innovators signal a fundamental shift in how medical technology gets developed. Innovation traditionally flowed from researchers and institutions to patients. Now, increasingly, it flows from patients’ lived experiences into technological solutions that address systemic gaps.
What unites them isn’t just technical capability or personal experience. It’s a refusal to accept the status quo, a determination to ask why their care couldn’t be better, then build the systems to make it so.