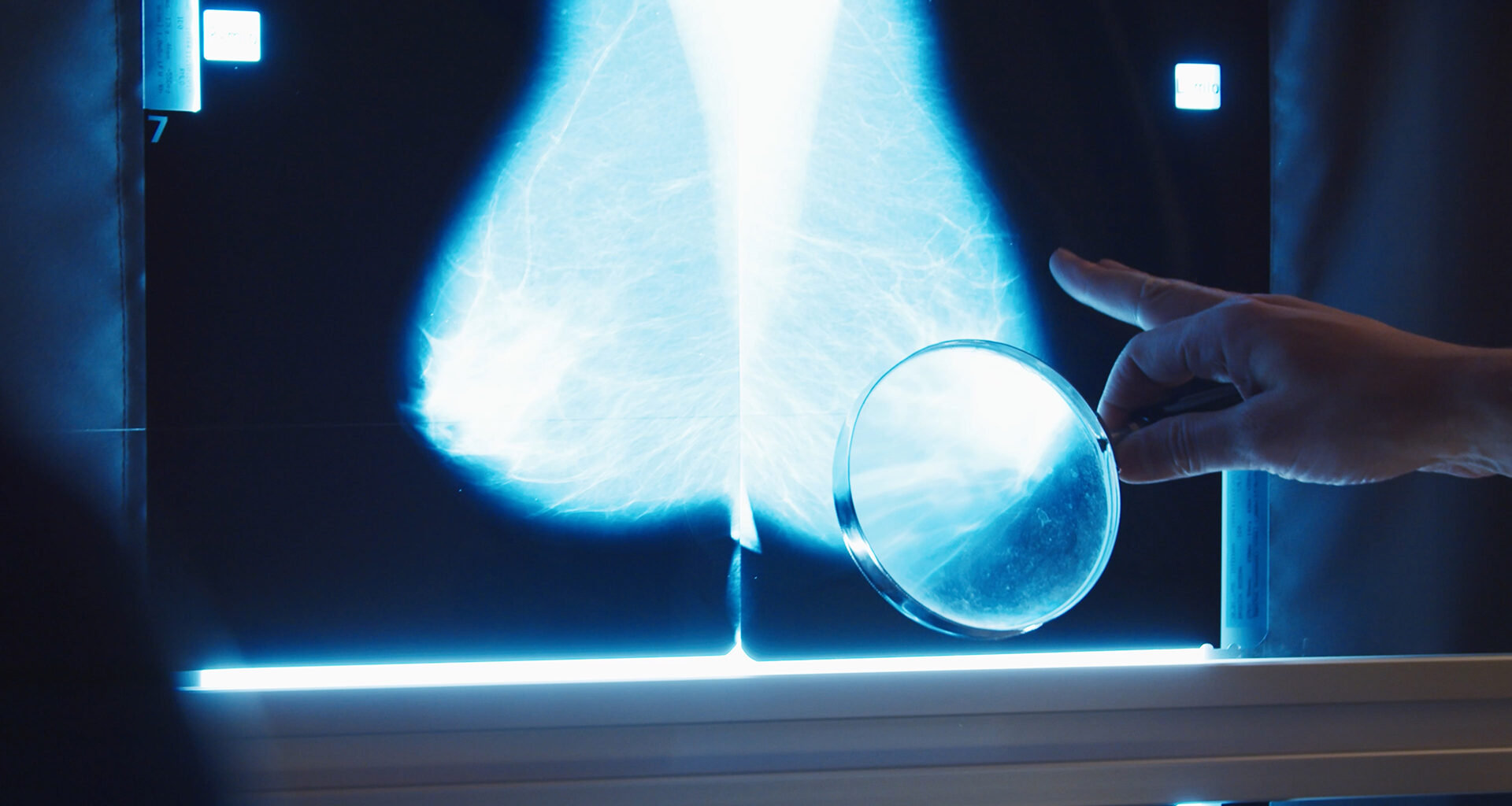
Dan Sarno, Founder and CTO at Sona, introduces the mobile breast density monitoring device aiming to enhance breast cancer detection.
Breast density is of crucial importance when it comes to the detection of breast cancer, as high breast density both increases breast cancer risk and can cause cancers to be missed on mammogram screenings. Despite this, most women are not aware of their breast density.
Focusing on breast density and aiming to revolutionise breast cancer screening, National Physical Laboratory (NPL) spinout Sona has developed the world’s first ultrasound-based breast density assessment and monitoring technology that does not require imaging or trained radiologists.
Sona’s technology enables healthcare providers to offer timely and personalised screening through simple, safe and low-cost access to breast density information, which is currently limited by age and use of traditional mammograms.
Unlike traditional methods that rely on X-rays, Sona’s patented solution leverages novel ultrasound sensor-platform technology to provide safer, more sensitive breast density assessments. Sona’s simple, low-cost desktop device, easily deployed in local GP clinics and primary care sites, delivers quick, reliable breast density readings.
To find out more about Sona’s innovation, The Innovation Platform spoke to Founder and CTO Dan Sarno.
Can you explain more about breast density and why it is so important to be aware of breast density in relation to cancer detection?
Breast density refers to the proportion of fibroglandular (dense) tissue compared to fatty tissue in the breast. Its most immediate impact is on how clearly a cancer can be seen on a mammogram. Dense tissue and tumours both appear white on a mammogram, which makes it difficult to spot cancers hidden within dense areas – a problem known as ‘masking’.
This is a major issue in screening. Studies show that up to half of cancers may be missed in women with dense breasts during routine mammograms. These are not rare outliers either – around 40-50% of women over 40 have dense breasts, with even higher prevalence in women in their 30s and 40s.
Beyond masking, breast density is also an independent risk factor. Women with extremely dense breasts may be up to six times more likely to develop breast cancer than those with low density. Despite this, breast density is not routinely measured or reported in UK screening programmes, leaving millions of women unaware that they face both an elevated risk and reduced benefit from standard screening.
How can breast density information provide better screening services?
Once breast density is known, it becomes possible to personalise screening to the individual – rather than relying on a one-size-fits-all approach. That’s already happening in parts of Europe and across the US, where women are routinely informed of their breast density and may be offered additional imaging, such as an ultrasound or MRI, if they’re at higher risk.
The UK has yet to adopt this model, but recent evidence suggests it could have a major impact. A UK study found that providing alternative, additional scans to mammograms for women with dense breasts could help detect more cancers earlier and potentially save around 700 lives a year. Without knowing who has dense tissue, these women are effectively invisible to the system.
Bringing density into routine screening would allow the NHS to make better-informed decisions – targeting enhanced screening where it’s most needed, and helping to close current gaps in early detection.
What is the premise of Sona’s ultrasound technology?
These developments highlight a gap in current breast screening pathways: the absence of a practical, routine method for measuring breast density. While mammograms can provide an estimate of density, this is not measured consistently and is rarely used to inform risk or follow-up care.
Without reliable, accessible ways to measure density across the population, opportunities for improved monitoring, early detection, and service planning are being missed.
In response to this challenge, a prospective spinout – known as Sona – from the UK’s National Physical Laboratory (NPL) is developing a new approach. We are working on a compact, ultrasound-based device designed to assess breast tissue composition safely, objectively, and in settings beyond the hospital.
How is the technology being developed?
Sona aims to deliver a safe, consistent, and accessible way to assess breast density which combines both reliable measurement and a comfortable experience – something distinctly different from the pain associated with mammograms.
The technology’s foundation is rooted in measurement science. The device uses ultrasound to extract quantitative measurement of breast tissue composition which is linked to breast density. Sona’s technical development builds on over a decade of research at NPL, including patent-protected sensor innovation and novel measurement methods.
The system is also being developed in consultation with women and clinicians to ensure the design is both comfortable and simple to use. By combining measurement science with co-designed product development, Sona is working towards a tool that can deliver reliable measurements quickly and be more sympathetic to the needs of women.
What stage is development at and what are the aims for the technology’s use (key users and when)?
The technology is currently at a preclinical stage, with working prototypes undergoing refinement ahead of first-in-human testing. Core components have been demonstrated in the lab, and the team is preparing for healthy volunteer studies in collaboration with NHS partners. These will assess performance and usability of the system ahead of larger-scale studies.
The development is being supported by the Government Office for Technology Transfer (GOTT) and the UK Innovation & Science Seed Fund (UKI2S), which are helping to progress the technology beyond research and into applied use. This includes advancing both the device itself and the surrounding clinical and regulatory pathway.
In the longer term, the system is being designed for use by trained healthcare staff – including nurses, screening practitioners, and primary care teams – in settings close to the community. The aim is to support earlier, safer, and more inclusive breast health assessment, particularly for women who are currently underserved by existing pathways.
What advantages could Sona’s device have over current screening methods?
Current breast screening is largely a one-size-fits-all approach centred around mammography, which has limitations – particularly for women with dense tissue and those considered average risk. Sona’s technology could enable a different approach: a personalised, risk-adaptive screening programme where women at higher risk or with dense breast tissue are informed from an earlier age through accessible measurement outside of a hospital setting.
Because the system is designed to be small, low-cost, and operator-independent, it could be used in community settings and earlier in life, making it easier to identify women who may benefit from tailored screening or further monitoring. This is particularly relevant for groups who are often underrepresented in current screening services, including younger women and those in underserved areas.
By providing consistent and accessible measurement of breast tissue properties, Sona’s technology could support more personalised screening pathways and contribute to earlier identification of those at increased risk – helping to close gaps in detection without replacing existing imaging methods.
Please note, this article will also appear in the 23rd edition of our quarterly publication.