Maternal history
A 34-year-old woman with a singleton pregnancy presented at 37 weeks and 5 days of gestation. Her medical history revealed a diagnosis of GDM, made based on test results at 26 weeks of gestation. The results included HbA1c of 5.4, Fasting Blood Sugar (FBS) of 98 mmol/L, and 2-h postprandial glucose (2hpp) of 130 mg/dL. After being diagnosed with gestational diabetes, she was referred to a dietitian for management. With adherence to the prescribed diet and continuous follow-up, her test results returned to the normal range for pregnancy over several measurements (2hpp > 120, FBS < 95).
Prenatal findings
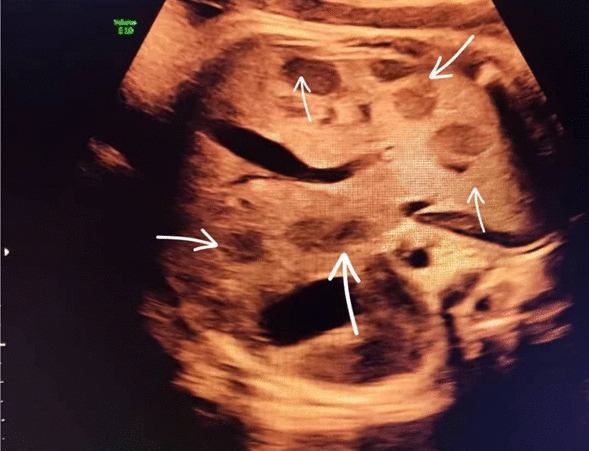
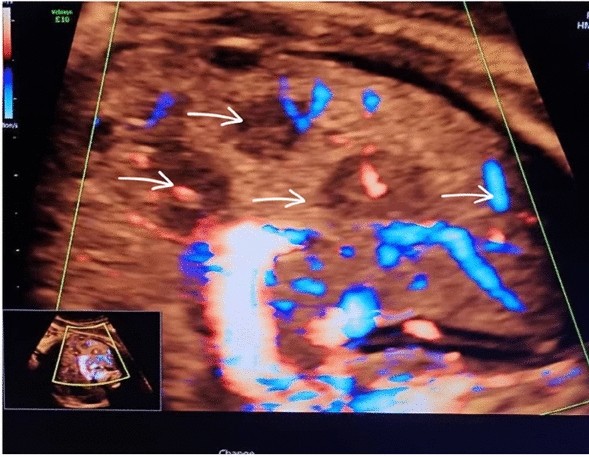
At 37 weeks of gestation, a routine third-trimester ultrasound revealed a hypoechoic lesions in the fetal liver. The lesions were well-circumscribed, measuring approximately 3.5 cm in diameter, and exhibited characteristics suggestive of a vascular tumor. Doppler imaging indicated hypervascularity, raising suspicion for a hemangioendothelioma. Furthermore, the fetal brain appeared normal upon prenatal evaluation. Amniotic fluid levels and fetal growth parameters were within normal limits, and no signs of fetal hydrops were observed. Amniotic fluid levels and fetal growth parameters were within normal limits, and no signs of fetal hydrops were observed. The fetal echocardiogram was normal. Figures 1, 2, and 3
Transverse view of the fetal abdomen obtained by sonography shows multiple hypoechoic lesions, indicated by arrows
Sagittal view of the fetal abdomen obtained with sonography, showing multiple hypoechoic lesions indicated by arrows
Sagittal view of the fetal abdomen using color Doppler ultrasound, showing vascularity and multiple hypoechoic lesions indicated by arrows
Referral and delivery
The patient was referred to the labor and delivery department at 38 weeks of gestation for further evaluation and management. Delivery was initiated due to the rupture of membranes and the presence of meconium-stained amniotic fluid. Following a multidisciplinary discussion involving obstetricians, neonatologists, and pediatric surgeons, a decision was made to proceed with delivery at term. The patient underwent a spontaneous vaginal delivery of a male neonate weighing 3,200 g, with Apgar scores of 8 and 9 at 1 and 5 min, respectively. The delivery was uncomplicated, and the mother remained hemodynamically stable in the postpartum period.
Neonatal evaluation
Postnatal imaging, including abdominal ultrasound and Magnetic Resonance Imaging (MRI), confirmed the presence of a 3.5 cm HH in the right lobe of the liver. Given that endothelial hemangioma (infantile hemangioma), particularly in multifocal forms, can be associated with intracranial vascular abnormalities, neuroimaging is recommended to rule out cerebrovascular involvement and prevent potentially serious complications such as stroke [10]. Therefore, to thoroughly evaluate and ensure that the central nervous system is not affected, a brain MRI was performed on the infant, which yielded normal results. Laboratory investigations revealed normal liver function tests and coagulation parameters. The neonate exhibited no signs of high-output cardiac failure or other complications associated with the tumor. Further evaluation was conducted, and the final diagnosis of hepatic hemangioendothelioma was confirmed based on imaging findings and clinical assessment.
Diagnosis and management
The final diagnosis of HH was established based on imaging findings and clinical evaluation. Given the asymptomatic nature of the tumor and the absence of complications, the neonate was managed conservatively with regular follow-up to monitor tumor size and potential complications. The parents were extensively counseled about the benign nature of the condition and the low likelihood of long-term sequelae. The baby was monitored for three months, and according to sonography and MRI findings, the tumor size had slightly decreased. The echocardiogram was normal, and fetal growth and development were within normal limits. The baby did not exhibit jaundice or heart complications. However, further follow-up was not possible due to the parents’ unwillingness and lack of cooperation.