Medical history
A 60-year-old man, who had been happily married for 37 years, retired in April 2021 after 18 years of working as a truck driver. His medical history included severe scoliosis that had been corrected surgically as a teenager, an occasional tinnitus, and arterial hypertension treated with lercanidipine and ramipril. He had no history of road accidents. Additionally, he had no history of parasomnia, other sleep problems, psychiatric issues, alcohol or drug abuse, or domestic violence.
History of violent strangulation episode
The following October 2021 he developed symptoms of anxiety, including severe sleep-onset insomnia. On November 14, 2021 his physician prescribed 0.125 mg of alprazolam at bedtime. This dosage was increased to 0.25 mg on November 17 due to inefficacy. On November 18 (the second night on 0.25 mg of alprazolam), he went to bed at 9 p.m. He woke up several times during the night to urinate. At 5:30 a.m., he was suddenly awakened by his wife’s loud coughing and found his hands tightly wrapped around his wife’s neck, choking her severely. She was unconscious but still breathing. He had no dream recall. He immediately called the police emergency phone number and explained his situation. He performed first aid as instructed by the operator. In the recording of the 50-minute phone conversation, he seemed to be oriented in time and place, as he gave a clear report of the events and the address for ambulance, but he was clearly appalled (he gave brief responses and repeated, “What have I done?“). The police and ambulance arrived 50 min later, due to the distance and specific safety procedures in cases of domestic violence, as the perpetrator had stated that he was in possession of two rifles and as three police officers had been recently shot dead when intervening on a case of domestic violence.
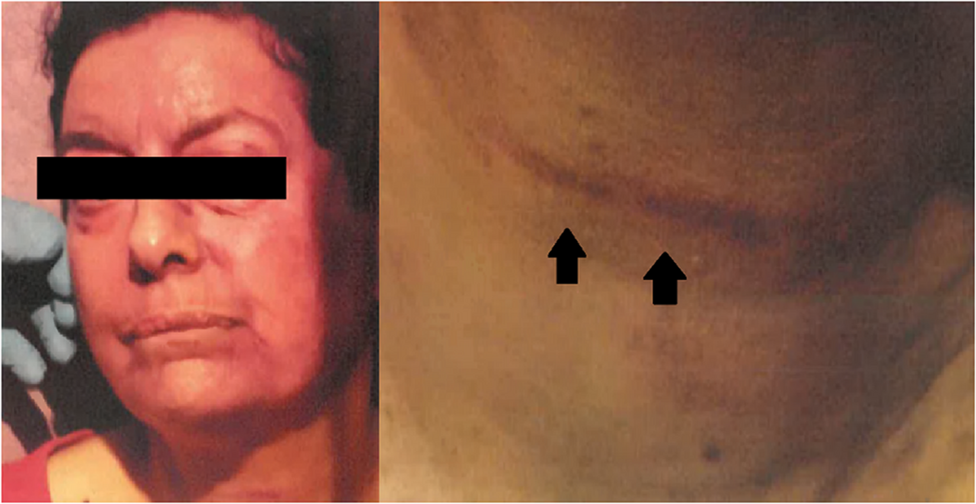
His wife (who was at first in the marital bed and then fell on the floor, according to the patient) was found unconscious on the floor behind the bed. She had severe traces of strangulation, cyanotic face, conjunctival redness, multiple petechiae, dyspnea, dysarthria and dysphagia (Fig. 1). She was hospitalized for 5 days, but eventually recovered fully, without any sequelae. She had a total amnesia of the event and reported that it was the first episode of violence in their 37 years of common life. Her husband was arrested for attempted homicide. A few hours later, his toxicology blood tests revealed no alcohol, normal carbon monoxide levels (0.3%), no cyanide, no cannabis, no lithium, and therapeutic levels of alprazolam (residual blood levels: 6.5 µg/L; therapeutic reference interval: 5–50 µg/L).
Lesions inflicted by the patient on wife’s neck (right panel, arrows), cyanotic lips and periorbital petechiae (left panel)
He appeared immediately in front of the examining magistrate. As he was seemingly devastated by what he had done, he was transferred to a psychiatric hospital for 2 weeks instead of jail. The psychiatrist only identified moderate secondary depression, reactive to these events. He received paroxetine 20 mg (that was progressively tapered down and stopped 13 days before the sleep study).
Psychiatric evaluation
Police investigations conducted with the family and neighbors revealed that the patient and his wife were a loving couple and that he was a quiet person. For 15 months, he was under judiciary control, forbidden to live with his wife, only allowed to phone her and meet with her in a restaurant. The submitted psychiatric evaluation (performed in March 2022, when the patient was treated for 3.5 months with paroxetine) stated that he had no psychosis or psychiatric disease except for mild reactive depression. He no longer experienced insomnia or anxiety. It also stated that alprazolam could be associated with paradoxical and sometimes violent side effects and recommended a sleep evaluation, with which the judge agreed. The patient and his wife repeatedly told the authorities that there was no prior history of domestic violence and no intentionality behind the episode.
Sleep interview
In the sleep interview, performed in January 2023, the patient had no sleep complaints. He reported urinating twice per night and experiencing no snoring, choking or dry mouth as potential symptoms of sleep apnea. He obtained an average of seven hours of restorative sleep per night. He denied experiencing sleepiness (scoring a 3/24 on the Epworth Sleepiness Scale; normative score < 11/24 [5]), restless legs syndrome, bruxism, or parasomnia. His spouse confirmed that there was no history of snoring or abnormal motor behavior at night. The REM Sleep Behavior Disorder Screening Questionnaire score was 1/13, normative score < 5/13 [6]. The patient recalled having one dream per month and reported no nightmares, hallucinations, or sleep paralysis. He was not anxious, depressed, or apathetic, and his interpersonal contact was appropriate. His hospital anxiety and depression scale scores were 5/21 for both anxiety and depression [7]. The Starkstein apathy scale score was 10/42, normative score < 15/42 [8].
The body mass index was 22.6 kg/m², which has been stable for over 10 years. Macroglossia was observed during pharynx examination, along with an erythematous velum and a Mallampati score of 2. Arterial blood pressure was 144/81 mm Hg, SpO2 was 100%. The neurological exam was normal, showing no signs of parkinsonism or cerebellar syndrome. There was no supine hypotension. The olfactory performance was excellent (11 odors recognized out of 12). He received a score of 25/30 on the Montreal Cognitive Assessment (a mildly decreased score, due to having received only six years of formal education) [9], a score of 28/30 on the Mini-Mental State Examination, and a score of 135/144 on the Mattis Scale (all normal scores). Neuropsychological examination showed reduced social cognition, a very mild dysexecutive syndrome on the Stroop test, and mildly altered episodic memory despite normal visuospatial abilities and memory, praxis, gnosis and language. Positron emission tomography with fluorodeoxyglucose revealed borderline hypometabolism in the bilateral frontal and temporal lobes. Meanwhile, metabolism was normal and symmetrical in the basal ganglia, parietal lobes, posterior cingulate, and cerebellum.
Sleep and video monitoring
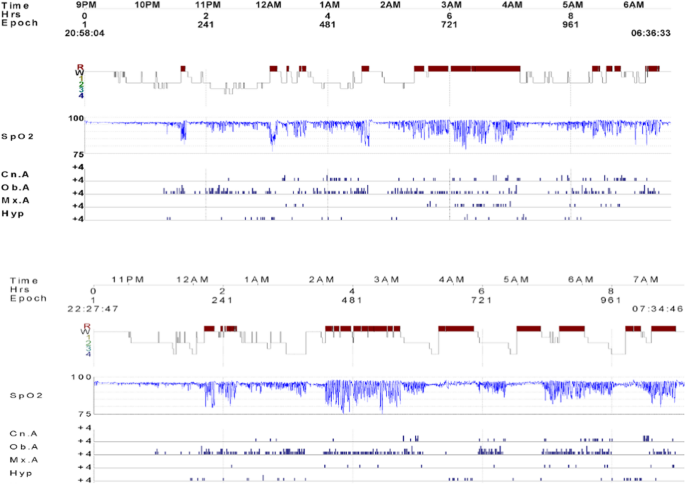
A two-night video-polysomnography was scheduled. In both nights, the sleep EEG was easy to score, with no abnormal figures, no abnormal slowing. The EEG rhythm was regular and in the alpha range at 8 Hz during quiet wakefulness. Sleep figures, including spindles, K complexes, slow waves, and sawtooth waves, were normal in shape and frequency. There were no signs of dissociated sleep, including no rapid eye movements during non-rapid eye movement (NREM) sleep, no abnormal REM sleep without atonia, no arousal containing slow waves in N3 sleep, and no epileptic figures. The first night showed severe obstructive sleep apnea (OSA), with an apnea-hypopnea index of 45 per hour (Fig. 2A). There were apneas lasting up to 100 s and significant desaturations (minimal saturation in NREM sleep: 81%; REM sleep: 76%). A total of 120 min were spent in apnea or hypopnea; 10% of that time was spent below SpO2 90%. REM sleep percentage was excessive (32% of total sleep time), probably due to a rebound post antidepressant withdrawal. The periodic leg movement index was 4.9 per hour. REM sleep without atonia occurred in only 4% of REM sleep, and neither simple nor complex behaviors were observed. The arousal index was 37.7/hour. On the second night, the man was given the same dose of alprazolam (0.25 mg at 9 p.m.) as on the night of the strangulation event. Video-polysomnography revealed a similar apnea-hypopnea index (46/hour), but longer apneas, and 150 min spent in apnea or hypopnea (Fig. 2B). Time spent below an SpO2 of 90% was 12.6% (minimal saturation in non-REM sleep: 84%; REM sleep: 74%). The arousal index was 51.7/hour. There were no parasomnia behaviors or abnormal movements (whether in N1, N2, N3 and REM sleep, including no confusional arousal nor any arousal in N3, no behavior, even mild in REM sleep), and REM sleep percentage was 42% without any REM sleep without atonia. The final diagnosis given in the expertise report (by IA and FC) was violent sudden confusional arousal induced by OSA, which was exacerbated by a benzodiazepine taken at bedtime.
Hypnograms obtained from video-polysomnography during A (upper panel: first night without any medication) and B (lower panel, second night when treated with alprazolam 0.5 mg at bedtime) (upper graph; R: REM sleep; W: wake; 1: N1; 2: N2; 3–4: N3 sleep stages), oxygen saturation (SpO2, middle graph) and respiratory events (lower graph Cn: central; Ob: obstructive, Mx: mixed; A: apnea; Hyp: hypopnea)
The patient began continuous positive airway pressure therapy and has shown good compliance and efficacy. Since the start of treatment, the patient has not experienced any additional violent episodes. The couple repeatedly told the judge that they loved each other and wanted to remain married. The man was released to return to his wife, and all legal charges were dropped. In our last contact, nearly four years after the violent incident, the couple was still happily married and sharing a bed. According to his wife, 4 years after the event, the patient was quiet during sleep, indicating that he has not developed RBD since the polysomnography evaluation. He reported not developing any neurological disorders, such as Parkinson’s disease or dementia, or any psychiatric disorders. The patient, his wife, the judge, and the Prosecutor of the Republic agreed to publish the case anonymously.