This study highlights the significant impact of anemia on clinical outcomes in patients presenting to the ED with AHF. When compared with large international registries such as ALARM-HF and ADHERE International-Asia Pacific, our findings show a similar prevalence of anemia (approximately 60–70%) and comparable trends in hospital admission rates and mortality [12, 13]. This alignment supports the generalizability of anemia as a common and clinically meaningful comorbidity among Asian patients with AHF.
The findings indicate that the severity of anemia is linked to higher rates of hospital admissions and increased requirements for oxygen supplementation. This suggests that anemia may serve as an indicator of more severe clinical presentations and underlying comorbidities. The relationship between anemia and outcomes in heart failure may also be influenced by the degree of congestion. Scicchitano et al. reported that patients with anemia exhibited higher levels of central congestion, indicated by elevated BNP levels, and greater peripheral congestion, assessed using a hydration index through bioimpedance analysis [14]. These findings imply that anemia in acute heart failure (AHF) may partially reflect a more severe congestion phenotype. In this context, hemodilution caused by intravascular volume expansion can lead to lower measured hemoglobin levels, while chronic comorbidities and inflammatory processes contribute to persistent anemia.
Patients with severe anemia had the highest hospital admission rates (93%) and the lowest discharge rates (6.6%), highlighting the significant clinical challenges and resource demands associated with this subgroup. Although in-hospital mortality tended to increase with anemia severity, the lack of statistical significance suggests that additional factors may influence mortality in this population. Previous studies have identified anemia and iron deficiency anemia as predictors of poor prognosis and increased mortality risk in heart failure patients [6, 15, 16]. However, this study did not include iron study to specify the associated risk factor.
A retrospective cohort study at Songklanagarind Hospital’s Emergency Department in southern Thailand examined predictive factors for 30-day adverse events in patients with AHF after discharge. The study involved 421 AHF patients and identified anemia as a significant risk factor. Anemia was linked to unscheduled ED revisits, hospital admissions for AHF, and deaths within 30 days post-discharge [17]. These results are consistent with our findings on anemia’s impact on hospital admissions.
The similar rates of ICU transfers and inotrope use among different levels of anemia severity indicate that once patients are admitted and stabilized, the intensity of treatment does not change significantly. This finding is consistent with findings from the ALARM-HF survey, which reported standardized management strategies for patients with AHF, regardless of subgroup differences. The survey highlighted that while ICU admissions were linked to higher mortality rates, treatments such as diuretics and inotropes were consistently used across various patient profiles [12].
However, the increased use of simple oxygen supplementation in severely anemic patients underscores the impact of reduced oxygen-carrying capacity on respiratory compromise. Beyond hemodilution and renal dysfunction, iron deficiency and inflammation are increasingly recognized as central drivers of anemia in heart failure. Elevated hepcidin levels can restrict iron absorption and mobilization, impairing erythropoiesis even in the absence of overt deficiency. De Biase et al. highlighted the role of inflammation-mediated iron sequestration in heart failure and its association with adverse outcomes [18]. Although our study lacked ferritin and hepcidin measurements, the high prevalence of anemia suggests that iron-restricted erythropoiesis may play a role in our population. This finding is supported by Siddiqui et al., who highlighted that anemia exacerbates hypoxia-induced physiological stress, often necessitating additional oxygen support in AHF patients [9]. The study by Pinto RD et al. highlighted that a reduced supply of oxygen to the tissues in anemic subjects triggers hemodynamic and neuro-hormonal alterations, which aggravate the myocardial workload and contribute, over time, to left ventricular remodeling [19].
Despite non-anemic patients showing a higher usage of dopamine, there was no significant difference in the use of other inotropes, such as norepinephrine and epinephrine. This indicates that the selection of inotropic agents may be influenced more by patients’ hemodynamic profiles and specific cardiac conditions rather than their anemia status. In line with findings from the Italian IN-HF Outcome registry, the use of inotropic therapies—particularly in patients with low systolic blood pressure was primarily driven by the severity of hemodynamic instability, rather than by isolated factors like anemia [20].
This study highlights the impact of anemia and its severity on outcomes in patients with AHF. The higher hospitalization rates observed in the more severe anemia groups underscore the need for a comprehensive approach to managing AHF patients with anemia. In many studies, anemia with IDA is associated with poor outcomes in HF. These include worsened disease progression and increased mortality rates. Treatment with iron supplementation is beneficial for patients with HF [21, 22]. However, current HF guidelines do not explicitly recommend the use of iron supplementation to reduce the severity of HF [2].
Further studies should delve into the specific causes of anemia to enable tailored management strategies that address the root causes effectively, such as chronic kidney disease or nutritional deficiencies. Additionally, future research should focus on exploring targeted interventions, such as early correction of anemia through iron supplementation or erythropoiesis-stimulating agents, to enhance clinical outcomes in selected groups of the AHF population.
Limitation
This study has several limitations. First, its retrospective design introduces inherent limitations, including potential selection bias, missing data, and reliance on the accuracy of documentation in electronic medical records. Because the data were collected retrospectively, important variables such as duration of anemia, iron status, and treatment responses were not consistently available. Furthermore, causality cannot be established between anemia and adverse outcomes due to the observational nature of the analysis. The results, therefore, represent associations that should be interpreted cautiously.
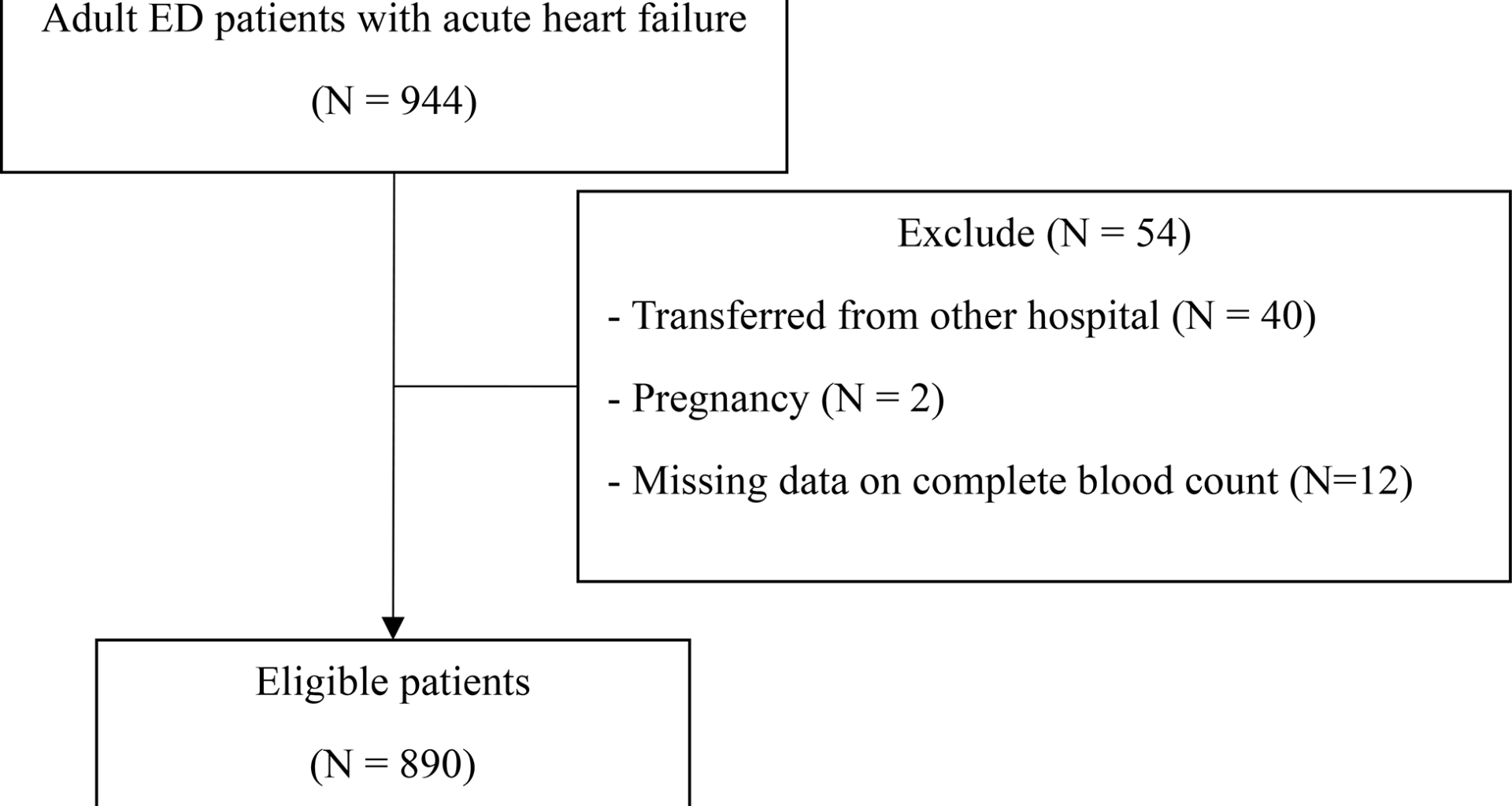
The study was conducted in a single hospital setting, which may limit the generalizability of the results to other populations or healthcare systems with different patient demographics or treatment protocols. Some patients were excluded due to incomplete data, particularly missing complete blood count (CBC) information, which may have affected the representativeness of the study population. The categorization of anemia was based on hemoglobin levels at the time of admission, which might not reflect chronic anemia or fluctuations due to acute illness or treatment interventions.
Potential confounding factors, such as nutritional status, pharmacological profiles, or underlying inflammatory conditions, were not accounted for, which could influence the relationship between anemia and outcomes. As an observational study, causation cannot be established between anemia and adverse outcomes. The findings are associations that warrant further exploration through prospective or interventional studies. The study focused on clinical and laboratory outcomes without evaluating the functional status or quality of life of the patients, which are essential aspects of heart failure management.
Additionally, outcome assessment was restricted to in-hospital events due to the retrospective single-center design, and follow-up data such as 30-day mortality or readmission were unavailable. This limits the ability to assess the longer-term prognostic effect of anemia in AHF.