Alex Barr arrived back from hospital on a fine spring day and sat in her car on the driveway panicking about the safety of her unborn baby.
She was almost 42 weeks pregnant and she and her husband Steven had been sent home by midwives at Poole Hospital who had dismissed her elevated heart rate and signs of bleeding.
Without warning, the specialist renal nurse felt a rush of warmth between her legs. Pulling her hand away she saw bright red blood and knew her daughter, Marnie, was in terrible danger.
Barr dialled 999 and was taken back to hospital by ambulance. It was too late. Marnie had already died. Barr’s repeated requests for an induction and procedures to bring on labour had been refused because of the midwives’ fixation, she believes, on a “normal” birth.
After a decade of inquiries into thousands of baby deaths in Britain, 65 per cent of maternity units still need to improve safety, according to the care watchdog.
But a Sunday Times investigation reveals today how the crisis has deeper roots, in the universities training the next generation of midwives. It found:
● Dozens of institutions are promoting an ideology of normal (vaginal) birth which avoids the use of instruments, drugs and caesarean sections.
● Experts say this has become the focus to the detriment of the clinical skills midwives need to care for the older and unhealthier women who are giving birth in Britain today.
● An analysis of publicly available curriculums show that 66 per cent of universities explicitly mention the promotion of normal birth. The NHS has moved away from this after a series of scandals linking it to deaths and poor care.
● The chief executive of the Royal College of Midwives (RCM) warned that universities should not be promoting an ideology and said she had been raising serious concerns about the quality of university education for student midwives.
● The Nursing and Midwifery Council (NMC) has been criticised for its poor monitoring of teaching quality.
● Donna Ockenden, the senior midwife who is leading the inquiry into the largest maternity scandal, said she was already concerned that students are not being taught required skills.
● Wes Streeting, the health secretary, said he was working with the NHS to overhaul midwifery training.
● Streeting has been separately warned that the government’s approach to maternity is failing to tackle a “deeper malaise” in the service, including training and ideas around normal birth.
In response to our investigation the NMC wrote to universities on Friday warning them against promoting normal birth. Paul Rees, the chief executive, told vice-chancellors that their courses must not deviate from the watchdog’s standards, demanding that all universities report back within a month on any courses that have been modified away from NMC standards.
Where the danger lies
A normal birth is what many women aim for — to avoid as much medical intervention as possible, such as forceps, other instruments, drugs and pain relief. One of the key targets is to avoid a caesarean section.
Natural births can offer a faster recovery time with some evidence suggesting it may be beneficial for the baby’s health and the mother’s wellbeing.
The danger lies in the unintended consequences of the overpromotion within universities and hospitals of an ideology around the ideal birth. That can lead to staff not intervening when they should, with potentially fatal consequences.
A series of hospital investigations has linked the ideology of normal birth to a reluctance among some midwives to call for doctors’ help and to resist women’s requests for inductions or caesareans.
The normal birth movement emerged in the 1970s, supported by organisations such as the National Childbirth Trust (NCT) in response to a perceived overmedicalisation of childbirth. The NCT says this is no longer its position. The World Health Organisation encouraged countries to pursue low caesarean rates and medical royal colleges encouraged midwives to delay intervening.
Following a series of scandals, in 2022 NHS England abandoned hospital targets for lower caesarean section rates and the RCM apologised for its normal birth campaign, acknowledging it may have gone too far.
However, concerns persist.
A document submitted to the Department of Health this year said the current approach to maternity was not working. Compiled by the team investigating the East Kent maternity scandal, in which dozens of babies and mothers died or were injured in childbirth, it warned that staff are being trained separately in “silos” — for example, doctors and midwives are taught different approaches. The result can “pit one professional group against another, most obviously around normal birth”. This can mean that midwives see their role as trying to prevent the involvement of doctors, and delay calling for help.
‘It felt like normal birth at all costs’
Alex and Steven Barr believe that was a key factor in Marnie’s death.
After being told her daughter had died, Barr was forced to give birth naturally on April 21, 2020, her pleas for a caesarean ignored. This is what is often recommended to parents to avoid surgery complications but a woman’s wishes should be taken into account.
“That was the most important thing to them,” she said: “I felt bullied by the consultant. It felt like normal birth at all costs.”
She suffers flashbacks and has been forced to quit her job: “It was like a bomb went off and everything just turned to darkness. My whole life has been blown apart in every way.”

Alex and Steven Barr believe there were many missed opportunities to save their daughter Marnie’s life
PETER TARRY FOR THE SUNDAY TIMES
A postmortem examination found that Marnie had been starved of oxygen, after Barr had suffered a possible placental abruption. Earlier this year, the University Hospitals Dorset NHS Foundation Trust settled the couple’s negligence claim with a six-figure payout.
The Barrs believe there were many missed opportunities to save their daughter’s life in the weeks leading up to her death. “As a mother, when something’s not right, you know, but nobody wanted to listen,” said Barr, now 37.

A post-mortem examination found that Marnie had been starved of oxygen
After asking to be induced, she was told by a community midwife to try clary sage oil aromatherapy and to go for a walk.
“There is no evidence to support that at all, it was all about achieving a normal birth,” she said. “It shouldn’t matter what interventions have to happen for a baby to be delivered safely and for that woman to receive safe care.”
Jennifer Janes, a solicitor for Enable Law, who represents Barr, said: “We have found that, sadly, this approach of normalising abnormal findings and avoiding medical intervention is a common theme, often resulting in the death or injury of babies, and we are deeply concerned that it is a cultural issue starting with the education of midwives.”
An ideological crusade
In 2023-24, more than 13,700 students at 62 universities studied for a midwifery degree, the qualification required to work as a registered midwife.
Using data on universities providing undergraduate midwifery from the Higher Education Statistics Agency, The Sunday Times has examined publicly available course materials and module descriptions to evaluate the emphasis universities placed on normal birth and promoting natural or physiological birth.
It was found in course materials for two thirds of universities, including some of the biggest providers such as Anglia Ruskin, Middlesex and the University of Salford.
At Middlesex, students are told the emphasis of some modules is on “promoting normality” and how to apply that “to women experiencing complexity”. It also offers training in complex situation and how to deal with “obstetric emergencies”.
The University of Greenwich’s 445 students are taught how to promote normality and the role of the midwife, which is described as “leading and promoting normality”. They also learn about complex care for women.
Similar language on “promoting normality” appeared in course materials at dozens more universities including Hertfordshire, Huddersfield and Bangor. However, they also offer courses in complex care. For example, at Huddersfield, students are taught “about pre-existing, current and emerging complications and additional care needs” and develop skills to “recognise compromise and deterioration, provide first-line management, escalate concerns appropriately and work collaboratively with the interprofessional team”.
Gill Walton, the RCM’s chief executive, said: “Our expectation is that universities do not promote an ideology of birth.
“Educating midwives to the evidence and making sure that they apply that evidence in practice — that’s what universities should be doing.”

Gill Walton, chief executive of the Royal College of Midwives
SUNDAY TIMES PHOTOGRAPHER RICHARD POHLE
At the University of Nottingham — where the local hospital is at the centre of the largest maternity scandal in NHS history, with Ockenden examining 2,400 baby deaths — students are taught about “optimising normality within complex midwifery care”.
• Our newborn died due to NHS errors — we were treated with contempt
A reading list included the work of Professor Soo Downe, from the University of Central Lancashire, which has been criticised for organising an annual “normal birth” conference for many years.
Also on the list was Sheena Byrom, co-director of All4Maternity, a private organisation that critics say supports the normal birth agenda. Following enquiries by The Sunday Times, the online information about the course was deleted.
Downe and Byrom both said their work may have been wrongly interpreted or applied by some staff and they rejected a “normal birth at any cost” ideology.
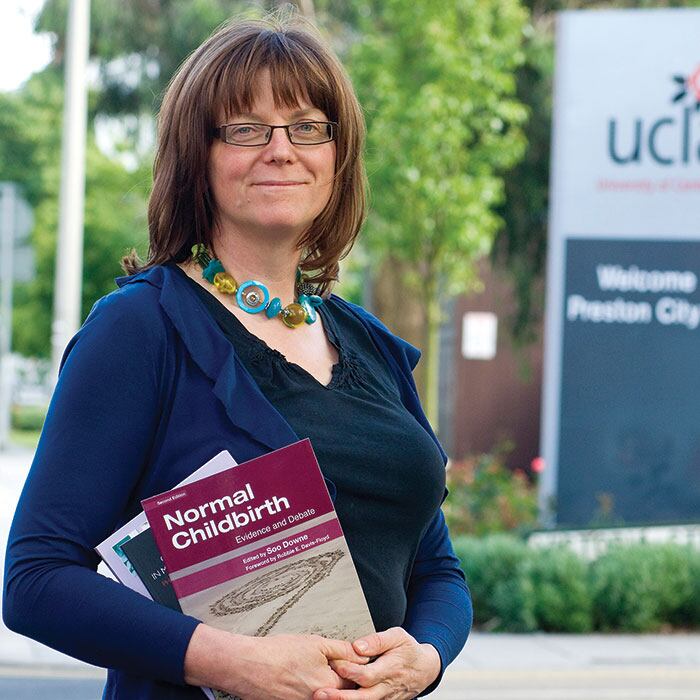
Soo Downe’s university ran a yearly “normal birth” conference
However, Bill Kirkup, a former obstetrician who led maternity investigations at Morecambe Bay, East Kent and Swansea hospitals, said: “It has become an ideological crusade in some people’s minds, probably in these universities where you’ve found these problems.”
He said training “silos” were part of the problem: “You’re setting them up from the start to think they are against each other. That you’re the guardian of normality.”
Older, heavier, sicker
Experts fear that a focus on normal birth is failing to prepare students for today’s reality: the women giving birth are now older, heavier and sicker than ever before. More than a quarter of pregnant women are now obese and the average age of a first-time mother is almost 31, compared with 26 in 1974.
Professor Marian Knight has worked on investigations into the deaths of women and babies during pregnancy at the national perinatal epidemiology unit at the University of Oxford.

She said: “I can see evidence that midwives don’t have the training, the understanding, to manage women who are very sick because of the change in the characteristics of women who are giving birth. What worries me is the [curriculums are] not moving with the times to recognise that change.” Knight believes the curriculum for midwives should be updated, or there needs to be more substantial postgraduate training.
Ockenden, who also led the inquiry into Shrewsbury and Telford Hospitals NHS Trust where almost 300 babies died or suffered brain damage as a result of poor care, said she had found that midwifery students worried about what they were being taught.
“I am picking up concerns from a range of colleagues across the perinatal team, including student midwives themselves, who have said to me that when they qualify, they will not be adequately prepared for the complexities of the women that they need to provide care for as registered midwives,” she said.
“What we have to do is look at the woman in front of us and make the right decisions in partnership with that woman to keep that mother and her baby safe. We should be providing individualised care for that mother and her baby, based on the needs that the mother presents to us, not any one ideology.”
• Three hundred babies lost to a fixation on natural births
James Titcombe, chief executive of the Patient Safety Watch charity, whose son Joshua died as a result of poor care in 2008, has warned for more than a decade about the risks of overemphasising “normality”.
“We’ve focused too much on hospital culture without looking at deeper issues — midwifery education is long overdue for scrutiny,” he said.

James Titcombe
PETER BYRNE/PA
‘Set up to fail’
Students confirmed an ideological focus on normal birth. One in the north of England said students were assessed on 38 skills, with 27 related to normal birth. Only 11 were about the additional care women might need.
“This is despite the fact that more than a third of women who give birth are having either caesarean sections or instrumental deliveries,” the student said. “It’s not really reflective of the current maternity picture.
“There’s been a lot of talk in the NHS around removing the whole normal birth ideology and outwardly I think that is happening. But as a student, in educational institutions, we are still very much in that place.
“A lot of us are fresh out of college and pretty much the first thing you are told about is normal birth. Our job as midwives is to prevent what they call the cascade of interventions and how that can cause problems.
“When you’ve got that message being given to you by lecturers, that is always going to remain in the back of your mind.”
Another student in the south said: “There is a lot of emphasis on normal births. There’s so little care about safety from that education side that I don’t know how we can expect midwives to be so focused on safety. It’s almost like you’re being set up to fail a lot of the time.”
Universities’ funding challenge
A Freedom of Information request by the RCM has uncovered widespread funding cuts across most midwifery programmes.
The university sector is facing £1.4 billion in net funding cuts in 2025-26, according to Universities UK.
Almost two fifths of midwifery departments have had a recruitment freeze or undergone a restructure in the previous year. Sixteen per cent of universities were planning to cut staff. The average number of staff per course has been cut by 15 per cent from 13 to 11.
Midwives are also being taught by staff who themselves don’t have key qualifications. Fewer than half had a postgraduate qualification and 30 per cent did not have any type of teaching qualification at all — up from 20 per cent in 2018.
Walton said concerns about quality of education and student experience had been raised by the RCM repeatedly in recent years.
She said: “There are some universities [which] absolutely have got it right but there’s also a whole bunch of students who are poorly educated, poorly trained in practice and have an awful experience.
“If we’re going to all be part of improving maternity services, then actually the whole system has to improve and that includes the education that student midwives have.
“Our expectation is that universities do not promote an ideology of birth. Promoting is not about being woman-centred, that is absolutely not the right thing to do.”
The absent watchdog
Universities train to standards set by theNMC. But the watchdog no longer requires formal teaching qualifications and has outsourced its assurance of education to a private company, the Quality Assurance Agency for Higher Education.
Streeting was warned in June by the Professional Standards Authority — a regulator of regulators — that there was “significant concern” over the NMC’s ability to monitor the quality of teaching.
The NMC said it was carrying out a review of midwifery curriculums and visited universities where concerns were raised.
Professor Donna O’Boyle, acting executive director of professional practice, said: “If any university is found to be misconstruing our standards in education provision, for example around the meaning of ‘optimising normal physiological processes’, we will address that directly with them as a matter of urgency.”
Streeting said: “Every mother deserves midwives trained for the reality of modern childbirth, in the principles of modern maternity care — respecting women’s choice, and individual circumstances — not an outdated ideal.
“I am working urgently with NHS England and the Nursing and Midwifery Council to overhaul midwifery training, so it reflects the complex needs of women today.”
The University of Nottingham said its programmes were based on best evidence and rigorously reviewed internally and approved by the NMC.
Middlesex University said its “midwifery provision is validated by the NMC standards for midwifery education”.
Ed Hughes, chief executive of the Council of Deans of Health, which represents more than 100 universities, said: “All our members are providing evidence-informed midwifery education with safety and quality always being paramount.”

