What is Diabetes? (CDC, 2023).
Harris, M. I. & Eastman, R. C. Early detection of undiagnosed diabetes mellitus: a US perspective. Diabetes Metab. Res Rev. 16, 230–236 (2000).
Meyer, T. W. & Hostetter, T. H. Uremia. N. Engl. J. Med. 357, 1316–1325 (2007).
Zemaitis, M. R., Foris, L. A., Katta, S. & Bashir, K. Uremia (StatPearls Publishing, 2024).
National Prevention Strategy: America’s Plan for Better Health and Wellness (US Department of Health and Human Services, Office of the Surgeon General, 2011); www.healthcare.gov/center/councils/nphpphc
Health and Economic Costs of Chronic Diseases (NCCDPHP, 2023).
Waters, H. & Graf, M. The Costs of Chronic Disease in the U.S. (Milken Institute, 2018).
Borsky, A. et al. Few Americans receive all high-priority, appropriate clinical preventive services. Health Aff. 37, 925–928 (2018).
Levine, S. Health Care Industry Insights: Why the Use of Preventive Services Is Still Low (CDC, 2019).
Genuis, S. J. The proliferation of clinical practice guidelines: professional development or medicine-by-numbers? J. Am. Board Fam. Pr. 18, 419–425 (2005).
Genuis, S. J. & Dabog, F. An ounce of prevention: a pound of cure for an ailing health care system. Can. Fam. Physician 53, 597 (2007).
Prevention is Still the Best Medicine (US Department of Health and Human Services, 2024).
Pavlou, A. K. & Turner, A. P. F. Sniffing out the truth: clinical diagnosis using the electronic nose. Clin. Chem. Lab. Med. 38, 99–112 (2000).
Lin, Y. J. et al. Application of the electronic nose for uremia diagnosis. Sens. Actuators B 76, 177–180 (2001).
Seyhan, A. A. Lost in translation: the valley of death across preclinical and clinical divide—identification of problems and overcoming obstacles. Transl. Med. Commun. 4, 18 (2019).
Wastewater COVID-19 Tracking (Massachusetts Water Resources Authority Online, 2024).
Daughton, C. G. Wastewater surveillance for population-wide COVID-19: the present and future. Sci. Total Environ. 736, 139631 (2020).
Randazzo, W., Cuevas-Ferrando, E., Sanjuán, R., Domingo-Calap, P. & Sánchez, G. Metropolitan wastewater analysis for COVID-19 epidemiological surveillance. Int. J. Hyg. Environ. Health 230, 113621 (2020).
Manemann, S. M. et al. Longitudinal cohorts for harnessing the electronic health record for disease prediction in a US population. BMJ Open 11, 2293–2301 (2021).
Robbins, T. et al. Diabetes and the direct secondary use of electronic health records: using routinely collected and stored data to drive research and understanding. Digit Health 4, 2055207618804650 (2018).
Dagan, N., Cohen-Stavi, C., Leventer-Roberts, M. & Balicer, R. D. External validation and comparison of three prediction tools for risk of osteoporotic fractures using data from population based electronic health records: Retrospective cohort study. BMJ 356, i6755 (2017).
Chai, P. R. et al. Assessment of the acceptability and feasibility of using mobile robotic systems for patient evaluation. JAMA Netw. Open 4, e210667 (2021).
Yue, S., He, H., Wang, H., Rahul, H. & Katabi, D. Extracting multi-person respiration from entangled RF signals. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2, 1–22 (2018).
Liu, Y. et al. Monitoring gait at home with radio waves in Parkinson’s disease: a marker of severity, progression, and medication response. Sci. Transl. Med. 14, eadc9669 (2022).
Hsu, C.-Y. et al. Zero-effort in-home sleep and insomnia monitoring using radio signals. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 1, 1–18 (2017).
Zhao, M., Yue, S., Katabi, D., Jaakkola, T. S. & Bianchi, M. T. Learning sleep stages from radio signals: a conditional adversarial architecture. In Proc. 34th International Conference on Machine Learning 4100–4109 (PMLR, 2017).
Zhao, M., Hoti, K., Wang, H., Raghu, A. & Katabi, D. Assessment of medication self-administration using artificial intelligence. Nat. Med. 27, 727–735 (2021).
Yang, Y. et al. Artificial intelligence-enabled detection and assessment of Parkinson’s disease using nocturnal breathing signals. Nat. Med. 28, 2207–2215 (2022).
Au-Yeung, W. T. M. et al. Monitoring behaviors of patients with late-stage dementia using passive environmental sensing approaches: a case series. Am. J. Geriatr. Psychiatry 30, 1–11 (2022).
Vahia, I. V. et al. Mapping behavior symptoms in dementia using passive radio sensing. Alzheimer’s Dement. 16, e044139 (2020).
Aspen Neuroscience to partner with Rune Labs and Emerald Innovations to incorporate both active and passive digital health monitoring in trial ready cohort screening study. PR Newswire (24 August 2023).
BlueRock Therapeutics to incorporate wearable and invisible contactless digital health technologies from Rune Labs and Emerald Innovations in Parkinson’s disease clinical trial. PR Newswire (14 March 2023).
Silverstein, A. Verge Genomics to incorporate Emerald Digital Health Technology into its ALS phase 1b proof-of-concept clinical trial. Business Wire (23 May 2023).
Coenraads, M. Rett Syndrome Research Trust awards $1.1 million to Emerald Innovations to develop novel invisible biosensor for objective measures of rett symptoms. Rett Syndrome Research Trust (21 February 2023).
From wearables to ‘invisibles’: we’re collaborating to study itch in sleeping children. Sanofi (13 December 2021).
Sherchan, S. P. et al. First detection of SARS-CoV-2 RNA in wastewater in North America: a study in Louisiana, USA. Sci. Total Environ. 743, 140621 (2020).
Foppe, K. S. et al. Analysis of 39 drugs and metabolites, including 8 glucuronide conjugates, in an upstream wastewater network via HPLC-MS/MS. J. Chromatogr. B 1176, 122747 (2021).
Naughton, C. C., et al. Show us the data: global COVID-19 wastewater monitoring efforts, equity, and gaps. FEMS Microbes 4, xtad003 (2023).
Wu, F. et al. SARS-CoV-2 RNA concentrations in wastewater foreshadow dynamics and clinical presentation of new COVID-19 cases. Sci. Total Environ. 805, 150121 (2022).
Farkas, K., Hillary, L. S., Malham, S. K., McDonald, J. E. & Jones, D. L. Wastewater and public health: the potential of wastewater surveillance for monitoring COVID-19. Curr. Opin. Environ. Sci. Health 17, 14–20 (2020).
Xiao, A. et al. Metrics to relate COVID-19 wastewater data to clinical testing dynamics. Water Res. 212, 118070 (2022).
Hassard, F. et al. Wastewater surveillance for rapid identification of infectious diseases in prisons. Lancet Microbe 3, e556–e557 (2022).
Vuori, E. et al. Wastewater analysis reveals regional variability in exposure to abused drugs and opioids in Finland. Sci. Total Environ. 487, 688–695 (2014).
Gushgari, A. J., Driver, E. M., Steele, J. C. & Halden, R. U. Tracking narcotics consumption at a Southwestern U.S. university campus by wastewater-based epidemiology. J. Hazard. Mater. 359, 437–444 (2018).
Gushgari, A. J., Venkatesan, A. K., Chen, J., Steele, J. C. & Halden, R. U. Long-term tracking of opioid consumption in two United States cities using wastewater-based epidemiology approach. Water Res. 161, 171–180 (2019).
Endo, N. et al. Rapid assessment of opioid exposure and treatment in cities through robotic collection and chemical analysis of wastewater. J. Med. Toxicol. 16, 195–203 (2020).
Duvallet, C., Hayes, B. D., Erickson, T. B., Chai, P. R. & Matus, M. Mapping community opioid exposure through wastewater-based epidemiology as a means to engage pharmacies in harm reduction efforts. Prev. Chronic Dis. 17, E91 (2020).
American Rescue Plan (The White House, 2021).
National Wastewater Surveillance System (NWSS) (CDC, 2023).
Wastewater Analysis and Drugs—a European Multi-City Study (European Monitoring Centre for Drugs and Drug Addiction, 2023).
Du, Z. et al. Predicting the hand, foot, and mouth disease incidence using search engine query data and climate variables: an ecological study in Guangdong, China. BMJ Open 7, e016263 (2017).
Kandula, S. & Shaman, J. Reappraising the utility of Google Flu Trends. PLoS Comput. Biol. 15, e1007258 (2019).
Ayyoubzadeh, S. M., Ayyoubzadeh, S. M., Zahedi, H., Ahmadi, M. & Niakan Kalhori, S. R. Predicting COVID-19 incidence through analysis of Google Trends data in Iran: data mining and deep learning pilot study. JMIR Publ. Health Surveill. 6, e18828 (2020).
Hoerger, M. et al. Impact of the COVID-19 pandemic on mental health: real-time surveillance using Google Trends. Psychol. Trauma 12, 567–568 (2020).
Cheng, Y., Wang, F., Zhang, P. & Hu, J. Risk prediction with electronic health records: a deep learning approach. In Proc. 2016 SIAM International Conference on Data Mining (ed. West, M.) 432–440 (SIAM, 2016).
Misra, S. et al. Precision subclassification of type 2 diabetes: a systematic review OPEN Plain language summary. Commun. Med. 10, 210 (2023).
Norgeot, B., Glicksberg, B. S. & Butte, A. J. A call for deep-learning healthcare. Nat. Med. 25, 14–15 (2019).
Razavian, N. et al. Population-level prediction of type 2 diabetes from claims data and analysis of risk factors. Big Data 3, 277–287 (2015).
Sahoo, P. K., Mohapatra, S. K. & Wu, S. L. Analyzing healthcare big data with prediction for future health condition. IEEE Access 4, 9786–9799 (2016).
Henry, K. E. et al. Factors driving provider adoption of the TREWS machine learning-based early warning system and its effects on sepsis treatment timing. Nat. Med. 28, 1447–1454 (2022).
Watkins, M. et al. Translating social determinants of health into standardized clinical entities. Stud. Health Technol. Inform. https://doi.org/10.3233/SHTI200205 (2020).
Mikhael, P. G. et al. Sybil: a validated deep learning model to predict future lung cancer risk from a single low-dose chest computed tomography. J. Clin. Oncol. https://doi.org/10.1200/jco.22.01345 (2023).
Obermeyer, Z., Powers, B., Vogeli, C. & Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 366, 447–453 (2019).
Brewer, L. P. C. et al. Back to the future: achieving health equity through health informatics and digital health. JMIR mHealth uHealth 8, e14512 (2020).
Huang, Y., Li, W., Macheret, F., Gabriel, R. A. & Ohno-Machado, L. A tutorial on calibration measurements and calibration models for clinical prediction models. J. Am. Med. Inform. Assoc. 27, 621–633 (2020).
Fisch, A., Jaakkola, T. & Barzilay, R. Calibrated selective classification. Preprint at https://doi.org/10.48550/arXiv.2208.12084 (2022).
Ajami, S. & Arab-Chadegani, R. Barriers to implement electronic health records (EHRs). Mater. Sociomed. 25, 213–215 (2013).
Bates, D. W. Physicians and ambulatory electronic health records. Health Aff. https://doi.org/10.1377/hlthaff.24.5.1180 (2024).
Uscher-Pines, L. & Mehrotra, A. Analysis of teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff. 33, 258–264 (2014).
Uscher-Pines, L. et al. Access and quality of care in direct-to-consumer telemedicine. Telemed. J. e-Health 22, 282–287 (2016).
Muntner, P. et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA 324, 1190 (2020).
Ettehad, D. et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387, 957–967 (2016).
Lee, S. G. et al. Remote cardiovascular hypertension program enhanced blood pressure control during the COVID-19 pandemic. J. Am. Heart Assoc. 12, e027296 (2023).
Flodgren, G., Rachas, A., Farmer, A. J., Inzitari, M. & Shepperd, S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, CD002098 (2015).
Omboni, S. et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension. Hypertension 76, 1368–1383 (2020).
Gambhir, S. S., Ge, T. J., Vermesh, O., Spitler, R. & Gold, G. E. Continuous health monitoring: an opportunity for precision health. Sci. Transl. Med. 13, eabe5383 (2021).
Rodbard, D. Continuous glucose monitoring: a review of recent studies demonstrating improved glycemic outcomes. Diabetes Technol. Ther. 19, S25–S37 (2017).
Eze, N. D., Mateus, C. & Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS ONE 15, e0237585 (2020).
Polinski, J. M. et al. Patients’ satisfaction with and preference for telehealth visits. J. Gen. Intern. Med. 31, 269–275 (2016).
Tuckson, R. V., Edmunds, M. & Hodgkins, M. L. Telehealth. N. Engl. J. Med. 377, 1585–1592 (2017).
Telehealth Policy Changes after the COVID-19 Public Health Emergency (Telehealth.HHS.gov, 2023).
Wosik, J. et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 27, 957–962 (2020).
Gerke, S., Shachar, C., Chai, P. R. & Cohen, I. G. Regulatory, safety, and privacy concerns of home monitoring technologies during COVID-19. Nat. Med. 26, 1176–1182 (2020).
Demaerschalk, B. M. et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June 2020. JAMA Netw. Open 5, e2229958 (2022).
Gajarawala, S. N. & Pelkowski, J. N. Telehealth benefits and barriers. J. Nurse Pract. 17, 218–221 (2021).
Gerhart, J., Piff, A., Bartelt, K. & Barkley, E. Telehealth Visits Frequently Billed at Lower Level of Service Than Office Visits (Epic Research, 2013).
Wang, W., Den Brinker, A. C., Stuijk, S. & De Haan, G. Algorithmic principles of remote PPG. IEEE Trans. Biomed. Eng. 64, 1479–1491 (2017).
Wang, H., Huang, J., Wang, G., Lu, H. & Wang, W. Surveillance camera-based cardio-respiratory monitoring for critical patients in ICU. In Proc. IEEE EMBS International Conference on Information Technology Applications in Biomedicine (ITAB) 1–4 (IEEE, 2022).
Siena, F. L., Byrom, B., Watts, P. & Breedon, P. Utilising the Intel RealSense camera for measuring health outcomes in clinical research. J. Med. Syst. 42, 53 (2018).
Huang, H.-W. et al. Mobile robotic platform for contactless vital sign monitoring. Cyborg Bionic Syst. https://doi.org/10.34133/2022/9780497 (2022).
Protalinski, E. How Draganfly Brought a ‘Pandemic Drone’ to the U.S. (VentureBeat, 2020).
Huang, H.-W. et al. Cost-effective blimp for autonomous and continuous vital signs monitoring. In Proc. IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM) 1553–1559 (IEEE, 2024).
Gong, Z. et al. SHUYU Robot: an automatic rapid temperature screening system. Chin. J. Mech. Eng. 33, 1–4 (2020).
Cruzr Health Monitoring Robot (RobotLab, 2022).
Bogue, R. Robots in a contagious world. Ind. Robot 47, 673–642 (2020).
Jin, Z., Huang, J., Wang, W., Xiong, A. & Tan, X. Estimating human weight from a single image. IEEE Trans. Multimed. https://doi.org/10.1109/TMM.2022.3147945 (2022).
Jiang, M., Shang, Y. & Guo, G. On visual BMI analysis from facial images. Image Vis. Comput 89, 183–196 (2019).
Kocabey, E. et al. Face-to-BMI: using computer vision to infer body mass index on social media. Proc. Int. AAAI Conf. Web Soc. Media 11, 572–575 (2017).
Sun, Y. et al. Detecting discomfort in infants through facial expressions. Physiol. Meas. 40, 115006 (2019).
Huang, Z., Wang, W. & De Haan, G. Nose breathing or mouth breathing? A thermography-based new measurement for sleep monitoring. In 2021 IEEE/CVF Conference on Computer Vision and Pattern Recognition Workshops 3877–3883 (IEEE, 2021).
Wang, X., Ellul, J. & Azzopardi, G. Elderly fall detection systems: a literature survey. Front. Robot. AI 7, 71 (2020).
Park, S.-m. et al. A mountable toilet system for personalized health monitoring via the analysis of excreta. Nat. Biomed. Eng. 4, 624–635 (2020).
Moço, A. V., Stuijk, S. & de Haan, G. Motion robust PPG-imaging through color channel mapping. Biomed. Opt. Express 7, 1737 (2016).
Nowara, E. M., Marks, T. K., Mansour, H. & Veeraraghavan, A. SparsePPG: towards driver monitoring using camera-based vital signs estimation in near-infrared. In Proc. IEEE/CVF Conference on Computer Vision and Pattern Recognition Workshops (CVPRW) 1353–135309 (IEEE, 2018).
Dasari, A., Prakash, S. K. A., Jeni, L. A. & Tucker, C. S. Evaluation of biases in remote photoplethysmography methods. npj Digit. Med. 4, 91 (2021).
Pereira, C. B. et al. Remote monitoring of breathing dynamics using infrared thermography. Biomed. Opt. Express 6, 4378 (2015).
Bardou, M. et al. Modern approach to infectious disease management using infrared thermal camera scanning for fever in healthcare settings. J. Infect. 74, 95–97 (2017).
Nakagawa, K., Kawamoto, H. & Sankai, Y. Integrated non-invasive vital signs monitoring system for detecting stress. In Proc. 2018 57th Annual Conference of the Society of Instrument and Control Engineers of Japan (SICE) 1612–1617 (IEEE, 2018).
Huynh, S., Tan, H.-P. & Lee, Y. Towards unobtrusive mental well-being monitoring for independent-living elderly. In Proc. 4th International on Workshop on Physical Analytics 1–6 (ACM, 2017).
Wright, W. F. & Mackowiak, P. A. Why temperature screening for coronavirus disease 2019 With noncontact infrared thermometers does not work. Open Forum Infect. Dis. 8, ofaa603 (2021).
Bao, F. et al. Heat-assisted detection and ranging. Nature 619, 743–748 (2023).
Wang, Y., Wang, W., Van Gastel, M. & De Haan, G. Modeling on the feasibility of camera-based blood glucose measurement. In 2019 IEEE/CVF Conference on Computer Vision and Pattern Recognition Workshops (CVPRW) 1713–1720 (IEEE, 2019)
Choi, J. H., Kang, K. B. & Kim, K. T. Remote respiration monitoring of moving person using radio signals. Lect. Notes Comput. Sci. 13697, 253–270 (2022).
Ravichandran, R. et al. WiBreathe: estimating respiration rate using wireless signals in natural settings in the home. In Proc. 2015 IEEE International Conference on Pervasive Computing and Communications (PerCom) 131–139 (IEEE, 2015).
Zhao, M., Adib, F. & Katabi, D. Emotion recognition using wireless signals. Commun. ACM 61, 91–100 (2018).
Hsu, C. Y., Hristov, R., Lee, G. H., Zhao, M. & Katabi, D. Enabling identification and behavioral sensing in homes using radio reflections. In Proc. Conference on Human Factors in Computing Systems 1–13 (Association for Computing Machinery, 2019).
Adib, F., Kabelac, Z. & Katabi, D. Multi-person localization via rf body reflections. In Proc. 12th USENIX Symposium on Networked Systems Design and Implementation 279–292 (USENIX, 2015).
Hsu, C. Y. et al. Extracting gait velocity and stride length from surrounding radio signals. In Proc. 2017 CHI Conference on Human Factors in Computing Systems 2116–2126 (ACM, 2017).
Adib, F., Mao, H., Kabelac, Z., Katabi, D. & Miller, R. C. Smart homes that monitor breathing and heart rate. In Proc. Conference on Human Factors in Computing Systems 837–846 (ACM, 2015).
Cournoyer, K. Contactless wireless health monitoring system shows potential for use in clinical trials. AAAS EurekAlert! (30 May 2019).
Loring, M. et al. Novel technology to capture objective data from patients’ recovery from laparoscopic endometriosis surgery. J. Minim. Invasive Gynecol. 28, 325–331 (2021).
Kabelac, Z. et al. An in-home study of facioscapulohumeral muscular dystrophy (FSHD) patients using contactless wireless sensing and machine learning (1561). Neurology 94, 15_supplement (2020).
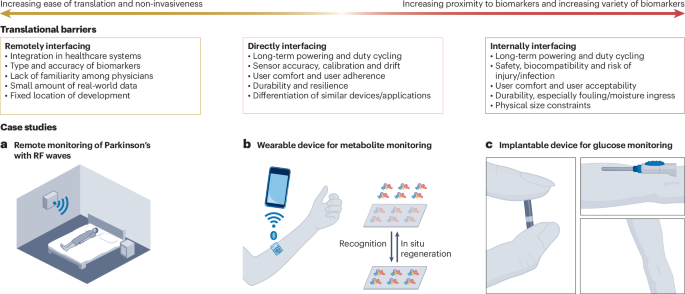
Ates, H. C. et al. End-to-end design of wearable sensors. Nat. Rev. Mater. 7, 887–907 (2022).
Yang, Y. & Gao, W. Wearable and flexible electronics for continuous molecular monitoring. Chem. Soc. Rev. 48, 1465–1491 (2019).
Jagannath, B. et al. A sweat-based wearable enabling technology for real-time monitoring of IL-1β and CRP as potential markers for inflammatory bowel disease. Inflamm. Bowel Dis. 26, 1533–1542 (2020).
Jagannath, B. et al. Temporal profiling of cytokines in passively expressed sweat for detection of infection using wearable device. Bioeng. Transl. Med. 6, e10220 (2021).
Kim, D.-H. et al. Epidermal electronics. Science 333, 838–843 (2011).
Chung, H. U. et al. Binodal, wireless epidermal electronic systems with in-sensor analytics for neonatal intensive care. Science 363, eaau0780 (2019).
Take an ECG with the ECG app on Apple Watch (Apple, 2023).
Wrist Monitor (biobeat, 2022).
Diagnose Your Irregular Heart Rhythm Faster and More Reliably with Zio (iRHYTHM, 2024).
Sugiyama, M. et al. An ultraflexible organic differential amplifier for recording electrocardiograms. Nat. Electron. 2, 351–360 (2019).
Perez, M. V. et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N. Engl. J. Med. 381, 1909–1917 (2019).
Detection vs Diagnosis: iRhythm and the Apple Watch (iRHYTHM, 2019).
Khunte, A. et al. Detection of left ventricular systolic dysfunction from single-lead electrocardiography adapted for portable and wearable devices. npj Digit. Med. 6, 124 (2023).
Lee, S. P., et al. Highly flexible, wearable, and disposable cardiac biosensors for remote and ambulatory monitoring. npj Digit. Med. 1, 2 (2018).
Chen, M., Ma, Y., Song, J., Lai, C. F. & Hu, B. Smart clothing: connecting human with clouds and big data for sustainable health monitoring. Mob. Netw. Appl. 21, 825–845 (2016).
Sepehri Shamloo, A., Bollmann, A., Dagres, N., Arya, A. & Hindricks, G. Smart watch devices for atrial fibrillation screening: it has to start somewhere. J. Am. Coll. Cardiol. 75, 1364–1365 (2020).
Chouhan, V. S. & Mehta, S. S. Total Removal of Baseline Drift from ECG Signal. In Proc. 2007 International Conference on Computing: Theory and Applications (ICCTA’07) 512–515 (IEEE, 2007).
Jeong, J. et al. Capacitive epidermal electronics for electrically safe, long-term electrophysiological measurements. Adv. Health. Mater. 3, 642–648 (2014).
Li, X. et al. A self-supporting, conductor-exposing, stretchable, ultrathin, and recyclable kirigami-structured liquid metal paper for multifunctional E-skin. ACS Nano 16, 5909–5919 (2022).
Goverdovsky, V., Looney, D., Kidmose, P. & Mandic, D. P. In-ear EEG From viscoelastic generic earpieces: robust and unobtrusive 24/7 monitoring. IEEE Sens. J. 16, 271–277 (2016).
Bulling, A., Roggen, D. & Tröster, G. Wearable EOG goggles: seamless sensing and context-awareness in everyday environments. J. Ambient Intell. Smart Environ. 1, 157–171 (2009).
Phinyomark, A., Khushaba, N. R. & Scheme, E. Feature extraction and selection for myoelectric control based on wearable EMG sensors. Sensors 18, 1615 (2018).
Jiang, S., Gao, Q., Liu, H. & Shull, P. B. A novel, co-located EMG-FMG-sensing wearable armband for hand gesture recognition. Sens. Actuators A 301, 111738 (2020).
Pico EMG (cometa, 2021).
STRIVE Elite (STRIVE, 2022).
You, S. S. et al. An ingestible device for gastric electrophysiology. Nat. Electron. 7, 497–508 (2024).
Gharibans, A. A. et al. Gastric dysfunction in patients with chronic nausea and vomiting syndromes defined by a noninvasive gastric mapping device. Sci. Transl. Med. 14, 3544 (2022).
Xu, S., Kim, J., Walter, J. R., Ghaffari, R. & Rogers, J. A. Translational gaps and opportunities for medical wearables in digital health. Sci. Transl. Med. 14, eabn6036 (2022).
Büyüközkan, G. & Göçer, F. Smart medical device selection based on intuitionistic fuzzy Choquet integral. Soft Comput. 23, 10085–10103 (2019).
Theodos, K. & Sittig, S. Health information privacy laws in the digital age: HIPAA doesn’t apply. Perspect. Health Inf. Manag. 18, 1l (2021).
Lee, S. et al. Nanomesh pressure sensor for monitoring finger manipulation without sensory interference. Science 370, 966–970 (2020).
Cheng, S. et al. Ultrathin hydrogel films toward breathable skin-integrated electronics. Adv. Mater. 35, e2206793 (2023).
Say, M. G. et al. Ultrathin paper microsupercapacitors for electronic skin applications. Adv. Mater. Technol. 7, 2101420 (2022).
Jia, J. et al. Conductive thread-based textile sensor for continuous perspiration level monitoring. Sensors 18, 3775 (2018).
Kannaian, T., Neelaveni, R. & Thilagavathi, G. Design and development of embroidered textile electrodes for continuous measurement of electrocardiogram signals. J. Ind. Text. 42, 303–318 (2012).
Wicaksono, I. et al. A tailored, electronic textile conformable suit for large-scale spatiotemporal physiological sensing in vivo. npj Flex. Electron. 4, 5 (2020).
Parlak, O., Keene, S. T., Marais, A., Curto, V. F. & Salleo, A. Molecularly selective nanoporous membrane-based wearable organic electrochemical device for noninvasive cortisol sensing. Sci. Adv. 4, eaar2904 (2018).
Min, J. et al. Skin-interfaced wearable sweat sensors for precision medicine. Chem. Rev. 123, 5049–5138 (2023).
Sharma, S., Saeed, A., Johnson, C., Gadegaard, N. & Cass, A. E. Rapid, low cost prototyping of transdermal devices for personal healthcare monitoring. Sens. Biosens. Res. 13, 104–108 (2017).
La Count, T. D., Jajack, A., Heikenfeld, J. & Kasting, G. B. Modeling glucose transport from systemic circulation to sweat. J. Pharm. Sci. 108, 364–371 (2019).
Talyor, N. P. Dexcom receives FDA clearance for first OTC glucose sensor. MEDTECHDIVE (6 March 2024).
Abbott introduces first ever consumer biowearable, LingoTM, set to re-energise the nation. Abbott (9 January 2024).
The American Diabetes Association Releases the Standards of Care in Diabetes—2024 (American Diabetes Association, 2023).
Findings from our FreeStyle Libre/GLP-1 analysis. Abbott https://www.abbott.com/corpnewsroom/strategy-and-strength/findings-from-our-freestyle-libre-glp-1-analysis.html (2023).
Heikenfeld, J. et al. Accessing analytes in biofluids for peripheral biochemical monitoring. Nat. Biotechnol. 37, 407–419 (2019).
Moonla, C. et al. Continuous ketone monitoring via wearable microneedle patch platform. ACS Sens. 9, 1004–1013 (2024).
Mannoor, M. S. et al. Graphene-based wireless bacteria detection on tooth enamel. Nat. Commun. 3, 763 (2012).
Kim, H. S. et al. Hand-held raman spectrometer-based dual detection of creatinine and cortisol in human sweat using silver nanoflakes. Anal. Chem. 93, 14996–15004 (2021).
Wang, M. et al. A wearable electrochemical biosensor for the monitoring of metabolites and nutrients. Nat. Biomed. Eng. 6, 1225–1235 (2022).
Tu, J., Torrente-Rodríguez, R. M., Wang, M. & Gao, W. The era of digital health: a review of portable and wearable affinity biosensors. Adv. Funct. Mater. 30, 1906713 (2020).
Gao, Y. et al. A flexible multiplexed immunosensor for point-of-care in situ wound monitoring. Sci. Adv. 7, eabg9614 (2021).
Flynn, C. D. et al. Biomolecular sensors for advanced physiological monitoring. Nat. Rev. Bioeng. 1, 560–575 (2023).
Goode, J. A., Rushworth, J. V. H. & Millner, P. A. Biosensor regeneration: a review of common techniques and outcomes. Langmuir 31, 6267–6276 (2015).
Jiang, Y. et al. A universal interface for plug-and-play assembly of stretchable devices. Nature 614, 456–462 (2023).
Yang, Y. et al. A laser-engraved wearable sensor for sensitive detection of uric acid and tyrosine in sweat. Nat. Biotechnol. 38, 217–224 (2020).
Breda, J., Springston, M., Mariakakis, A. & Patel, S. FeverPhone. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 7, 17 (2023).
Webb, R. C. et al. Ultrathin conformal devices for precise and continuous thermal characterization of human skin. Nat. Mater. 12, 938–944 (2013).
Yokota, T. et al. Ultraflexible, large-area, physiological temperature sensors for multipoint measurements. Proc. Natl Acad. Sci. USA 112, 14533–14538 (2015).
Shin, J. et al. Sensitive wearable temperature sensor with seamless monolithic integration. Adv. Mater. 32, 1905527 (2020).
Ota, H. et al. 3D printed “Earable” smart devices for real-time detection of core body temperature. ACS Sens. 2, 990–997 (2017).
Song, E. et al. Mn2+-activated dual-wavelength emitting materials toward wearable optical fibre temperature sensor. Nat. Commun. 13, 2166 (2022).
Choe, A. et al. Stretchable and wearable colorimetric patches based on thermoresponsive plasmonic microgels embedded in a hydrogel film. NPG Asia Mater. 10, 912–922 (2018).
Xu, X., Karis, A. J., Buller, M. J. & Santee, W. R. Relationship between core temperature, skin temperature, and heat flux during exercise in heat. Eur. J. Appl. Physiol. 113, 2381–2389 (2013).
Lavery, L. A. et al. Preventing diabetic foot ulcer recurrence in high-risk patients. Diabetes Care 30, 14–20 (2007).
Brickwood, K.-J., Watson, G., O’Brien, J. & Williams, A. D. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR mHealth uHealth 7, e11819 (2019).
Nyan, M. N., Tay, F. E. H. & Murugasu, E. A wearable system for pre-impact fall detection. J. Biomech. 41, 3475–3481 (2008).
Chen, J., Kwong, K., Chang, D., Luk, J. & Bajcsy, R. Wearable sensors for reliable fall detection. In Proc. 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference 3551–3554 (IEEE, 2005).
Chen, C., Ding, S. & Wang, J. Digital health for aging populations. Nat. Med. 29, 1623–1630 (2023).
Sole with SensFloor Technology (ShawContract, 2023); www.shawcontract.com/en-US/resources/Sole%E2%84%A2-with-SensFloor%C2%AE-Technology
Tanaka, O., Ryu, T., Hayashida, A., Moshnyaga, V. G. & Hashimoto, K. A smart carpet design for monitoring people with dementia. Adv. Intell. Syst. Comput. 1089, 653–659 (2015).
Cantoral-Ceballos, J. A. et al. Intelligent carpet system, based on photonic guided-path tomography, for gait and balance monitoring in home environments. IEEE Sens. J. 15, 279–289 (2015).
Rialle, V., Duchene, F., Noury, N., Bajolle, L. & Demongeot, J. Health ‘smart’ home: information technology for patients at home. Telemed. J. e-Health 8, 395–409 (2004).
Trung, T. Q. & Lee, N.-E. Flexible and stretchable physical sensor integrated platforms for wearable human-activity monitoringand personal healthcare. Adv. Mater. 28, 4338–4372 (2016).
Zhong, J. et al. Smart face mask based on an ultrathin pressure sensor for wireless monitoring of breath conditions. Adv. Mater. 34, 2107758 (2022).
Tee, B. C.-K. et al. Tunable flexible pressure sensors using microstructured elastomer geometries for intuitive electronics. Adv. Funct. Mater. 24, 5427–5434 (2014).
Tee, B. C.-K., Wang, C., Allen, R. & Bao, Z. An electrically and mechanically self-healing composite with pressure- and flexion-sensitive properties for electronic skin applications. Nat. Nanotechnol. 7, 825–832 (2012).
Yamada, T. et al. A stretchable carbon nanotube strain sensor for human-motion detection. Nat. Nanotechnol. 6, 296–301 (2011).
Kaltenbrunner, M. et al. An ultra-lightweight design for imperceptible plastic electronics. Nature 499, 458–463 (2013).
Jung, S. et al. Reverse-micelle-induced porous pressure-sensitive rubber for wearable human-machine interfaces. Adv. Mater. 26, 4825–4830 (2014).
Persano, L. et al. High performance piezoelectric devices based on aligned arrays of nanofibers of poly(vinylidenefluoride-co-trifluoroethylene). Nat. Commun. 4, 1633 (2013).
Dagdeviren, C. et al. Conformable amplified lead zirconate titanate sensors with enhanced piezoelectric response for cutaneous pressure monitoring. Nat. Commun. 5, 4496 (2014).
Wu, J. M. et al. Ultrahigh sensitive piezotronic strain sensors based on a ZnSnO3 nanowire/microwire. ACS Nano 6, 4369–4374 (2012).
Zhang, J. et al. Smart soft contact lenses for continuous 24-hour monitoring of intraocular pressure in glaucoma care. Nat. Commun. 13, 5518 (2022).
Hegde, N., Bries, M. & Sazonov, E. A comparative review of footwear-based wearable systems. Electronics 5, 48 (2016).
Kim, J. et al. Soft wearable pressure sensors for beat-to-beat blood pressure monitoring. Adv. Health. Mater. 8, 1900109 (2019).
Kang, D. et al. Ultrasensitive mechanical crack-based sensor inspired by the spider sensory system. Nature 516, 222–226 (2014).
Heikenfeld, J. et al. Wearable sensors: modalities, challenges, and prospects. Lab Chip 18, 217–248 (2018).
Chen, G. et al. Discovering giant magnetoelasticity in soft matter for electronic textiles. Matter 4, 3725–3740 (2021).
Yokota, T. et al. Ultraflexible organic photonic skin. Sci. Adv. 2, e1501856 (2016).
Nicolò, A., Massaroni, C., Schena, E. & Sacchetti, M. The importance of respiratory rate monitoring: from healthcare to sport and exercise. Sensors 20, 6396 (2020).
Wang, C. et al. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat. Biomed. Eng. 2, 687–695 (2018).
Wang, C. et al. Continuous monitoring of deep-tissue haemodynamics with stretchable ultrasonic phased arrays. Nat. Biomed. Eng. 5, 749–758 (2021).
Hu, H. et al. A wearable cardiac ultrasound imager. Nature 613, 667–675 (2023).
Zhang, L. et al. A conformable phased-array ultrasound patch for bladder volume monitoring. Nat. Electron. 7, 77–90 (2024).
Wang, C. et al. Bioadhesive ultrasound for long-term continuous imaging of diverse organs. Science 377, 517–523 (2022).
Du, W. et al. Conformable ultrasound breast patch for deep tissue scanning and imaging. Sci. Adv. 9, eadh5325 (2024).
Chen, L. et al. Soft elastic hydrogel couplants for ultrasonography. Mater. Sci. Eng. C 119, 111609 (2021).
McCarthy, C., Pradhan, N., Redpath, C. & Adler, A. Validation of the Empatica E4 wristband. In Proc. 2016 IEEE EMBS International Student Conference (ISC) 1–4 (IEEE, 2016).
Corsano Health receives FDA clearance. Corsano (22 March 2024).
Jastrzebska-Perfect, P. et al. Translational neuroelectronics. Adv. Funct. Mater. 30, 1909165 (2020).
Yang, C. et al. Wearable and implantable intraocular pressure biosensors: recent progress and future prospects. Adv. Sci. 8, 2002971 (2021).
Iyengar, K. P. et al. Smart sensor implant technology in total knee arthroplasty. J. Clin. Orthop. Trauma 22, 101605 (2021).
Heywood, J. T. et al. Impact of practice-based management of pulmonary artery pressures in 2000 patients implanted With the CardioMEMS sensor. Circulation 135, 1509–1517 (2017).
Koh, A. et al. Ultrathin injectable sensors of temperature, thermal conductivity, and heat capacity for cardiac ablation monitoring. Adv. Healthc. Mater. 5, 373 (2016).
Kanick, S. C., Schneider, P. A., Klitzman, B., Wisniewski, N. A. & Rebrin, K. Continuous monitoring of interstitial tissue oxygen using subcutaneous oxygen microsensors: in vivo characterization in healthy volunteers. Microvasc. Res. 124, 6–18 (2019).
Sonmezoglu, S., Fineman, J. R., Maltepe, E. & Maharbiz, M. M. Monitoring deep-tissue oxygenation with a millimeter-scale ultrasonic implant. Nat. Biotechnol. 39, 855–864 (2021).
Guo, H. et al. Wireless implantable optical probe for continuous monitoring of oxygen saturation in flaps and organ grafts. Nat. Commun. 13, 3009 (2022).
Kwon, K. et al. A battery-less wireless implant for the continuous monitoring of vascular pressure, flow rate and temperature. Nat.Biomed. Eng. 7, 1215–1228 (2023).
Chow, E. Y., Beier, B. L., Francino, A., Chappell, W. J. & Irazoqui, P. P. Toward an implantable wireless cardiac monitoring platform integrated with an FDA-approved cardiovascular stent. J. Inter. Cardiol. 22, 479–487 (2009).
Lu, D., et al. Bioresorbable, wireless, passive sensors as temporary implants for monitoring regional body temperature. Adv. Health. Mater. 9, 2000942 (2020).
Boutry, C. M. et al. A stretchable and biodegradable strain and pressure sensor for orthopaedic application. Nat. Electron. 1, 314–321 (2018).
Implant Files (International Consortium of Investigative Journalists, 2018).
Valero-Sarmiento, J. M., Ahmmed, P. & Bozkurt, A. In Vivo evaluation of a subcutaneously injectable implant with a low-power photoplethysmography ASIC for animal monitoring. Sensors 20, 7335 (2020).
Zhong, Y. et al. Development of an implantable wireless and batteryless bladder pressure monitor system for lower urinary tract dysfunction. Surg. Interv. Devices 8, 2500107 (2020).
Dhowan, B. et al. Simple minimally-invasive automatic antidote delivery device (A2D2) towards closed-loop reversal of opioid overdose. J. Control. Release 306, 130–137 (2019).
Imtiaz, M. S., Bandoian, C. V. & Santoro, T. J. Hypoxia driven opioid targeted automated device for overdose rescue. Sci. Rep. 11, 24513 (2021).
Kanter, K. et al. Willingness to use a wearable device capable of detecting and reversing overdose among people who use opioids in Philadelphia. Harm Reduct. J. 18, 75 (2021).
Huang, H. W. et al. An implantable system for opioid safety. Device 2, 100517 (2024).
Templer, S. Closed-loop insulin delivery systems: past, present, and future directions. Front. Endocrinol. https://doi.org/10.3389/fendo.2022.919942 (2022).
Krishnan, S. R. et al. A wireless, battery-free device enables oxygen generation and immune protection of therapeutic xenotransplants in vivo. Proc. Natl Acad. Sci. USA 120, e2311707120 (2023).
Lee, I. et al. Electrocatalytic on-site oxygenation for transplanted cell-based-therapies. Nat. Commun. 14, 7019 (2023).
Malik, S. et al. Injectable sensors based on passive rectification of volume-conducted currents. IEEE Trans. Biomed. Circuits Syst. 14, 867–878 (2020).
Yang, S. Y. et al. Powering implantable and ingestible electronics. Adv. Funct. Mater. 31, 2009289 (2021).
Celinskis, D. & Towe, B. C. Wireless impedance measurements for monitoring peripheral vascular disease. In Proc. 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society 6937–6940 (IEEE, 2014).
Hoefman, E., Van Weert, H. C. P. M., Reitsma, J. B., Koster, R. W. & Bindels, P. J. Diagnostic yield of patient-activated loop recorders for detecting heart rhythm abnormalities in general practice: a randomised clinical trial. Fam. Pract. 22, 478–484 (2005).
FDA Approves First Continuous Glucose Monitoring System With a Fully Implantable Glucose Sensor and Compatible Mobile App For Adults With Diabetes (FDA, 2018).
Eversense User Guide (Eversense, 2019).
Li, C. et al. Design of biodegradable, implantable devices towards clinical translation. Nat. Rev. Mater. 5, 61–81 (2019).
Maji, S. et al. A low-power dual-factor authentication unit for secure implantable devices. In Proc. Custom Integrated Circuits Conference 1–4 (IEEE, 2020).
Faris, O. & Shuren, J. An FDA viewpoint on unique considerations for medical-device clinical trials. N. Engl. J. Med. 376, 1350–1357 (2017).
Sands, B. E. Biomarkers of inflammation in inflammatory bowel disease. Gastroenterology 149, 1275–1285 (2015).
Steiger, C. et al. Dynamic monitoring of systemic biomarkers with gastric sensors. Adv. Sci. 8, e2102861 (2021).
Huang, H.-W. et al. In situ detection of gastrointestinal inflammatory biomarkers using electrochemical gas sensors. In Proc. IEEE International Engineering in Medicine and Biology Conference (EMBC) 2491–2494 (IEEE, 2022).
Mau, M. M., Sarker, S. & Terry, B. S. Ingestible devices for long-term gastrointestinal residency: a review. Prog. Biomed. Eng. 3, 042001 (2021).
Liu, X. et al. Ingestible hydrogel device. Nat. Commun. 10, 493 (2019).
Liu, J. et al. Triggerable tough hydrogels for gastric resident dosage forms. Nat. Commun. 8, 124 (2017).
Liu, S., Chu, S., Beardslee, L. A. & Ghodssi, R. Hybrid and passive tissue-anchoring mechanism for ingestible resident devices. J. Microelectromech. Syst. 29, 706–712 (2020).
Lin, W., Shi, Y., Jia, Z. & Yan, G. Design of a wireless anchoring and extending micro robot system for gastrointestinal tract. Int. J. Med. Rob. Comput. Assist. Surg. 9, 167–179 (2013).
Liu, X. et al. Magnetic living hydrogels for intestinal localization, retention, and diagnosis. Adv. Funct. Mater. 31, 2010918 (2021).
Inda-Webb, M. E. et al. Sub-1.4 cm3 capsule for detecting labile inflammatory biomarkers in situ. Nature 620, 386–392 (2022).
Mimee, M. et al. An ingestible bacterial-electronic system to monitor gastrointestinal health. Science 360, 915–918 (2018).
Hafezi, H. et al. An ingestible sensor for measuring medication adherence. IEEE Trans. Biomed. Eng. 62, 99–109 (2015).
Kong, Y. L. et al. 3D-printed gastric resident electronics. Adv. Mater. Technol. 4, 1800490 (2019).
Belknap, R. et al. Feasibility of an ingestible sensor-based system for monitoring adherence to tuberculosis therapy. PLoS ONE 8, e53373 (2013).
Alipour, A., Gabrielson, S. & Patel, P. B. Ingestible sensors and medication adherence: focus on use in serious mental illness. Pharmacy 8, 103 (2020).
Bass, D. M., Prevo, M. & Waxman, D. S. Gastrointestinal safety of an extended-release, nondeformable, oral dosage form (OROS®): a retrospective study. Drug Saf. 25, 1021–1033 (2002).
Li, F. et al. Retention of the capsule endoscope: a single-center experience of 1000 capsule endoscopy procedures. Gastrointest. Endosc. 68, 174–180 (2008).
He, S., Yan, G. Z., Ke, Q., Wang, Z. W. & Chen, W. W. A wirelessly powered expanding-extending robotic capsule endoscope for human intestine. Int. J. Precis. Eng. Manuf. 16, 1075–1084 (2015).
Thwaites, P. A. et al. Comparison of gastrointestinal landmarks using the gas-sensing capsule and wireless motility capsule. Aliment Pharm. Ther. 56, 1337–1348 (2022).
Mc Caffrey, C., Twomey, K. & Ogurtsov, V. I. Development of a wireless swallowable capsule with potentiostatic electrochemical sensor for gastrointestinal track investigation. Sens. Actuators B 218, 8–15 (2015).
De la Paz, E. et al. A self-powered ingestible wireless biosensing system for real-time in situ monitoring of gastrointestinal tract metabolites. Nat. Commun. 13, 7405 (2022).
McRae, J. C., Jastrzebska-Perfect, P. & Traverso, G. Challenges and opportunities for ingestible electronics across timescales. Device https://doi.org/10.1016/j.device.2023.100055 (2023).
Byrne, J. et al. Devices for drug delivery in the gastrointestinal tract: a review of systems physically interacting with the mucosa for enhanced delivery. Adv. Drug Deliv. Rev. 177, 113926 (2021).
Min, J., Yang, Y., Wu, Z. & Gao, W. Robotics in the gut. Adv. Ther. 3, 1900125 (2020).
Abramson, A. et al. A luminal unfolding microneedle injector for oral delivery of macromolecules. Nat. Med. 25, 1512–1518 (2019).
Steiger, C. et al. Ingestible electronics for diagnostics and therapy. Nat. Rev. Mater. 4, 83–98 (2019).
FDA Approval for Eko Health CORE 500 Digital Stethoscope (FDA, 2024); www.accessdata.fda.gov/cdrh_docs/pdf23/K233609.pdf
FDA Approval for the Apple Watch in Monitoring Cardiac Arrhythmia (FDA, 2018); www.accessdata.fda.gov/cdrh_docs/reviews/DEN180042.pdf
FDA Approval for the Apple Watch in Monitoring Atrial Fibrillation History (FDA, 2022); www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K213971
FDA Emergency Use Authorization for the VitalPatch by VitalConnect (FDA, 2020); www.fda.gov/media/137397/download#:~:text=Based%20on%20bench%20testing%20and,intervals%20and%20may%20cause%20life
FDA Permits Marketing of Device That Senses Optimal Time to Check Patient’s Eye Pressure (FDA, 2016); www.fda.gov/news-events/press-announcements/fda-permits-marketing-device-senses-optimal-time-check-patients-eye-pressure
BioIntellisense wins FDA nod for BioButton multi-patient wearable monitor. Mass Device (2 October 2024); www.massdevice.com/biointellisense-fda-nod-biobutton-wearable-monitor/
FDA Approval of CardioMEMS Implant by Abbott (FDA, 2022); www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P100045S056
Zimmer Biomet and Canary Medical Announce FDA de novo classification grant and authorization to market the world’s first and only smart knee implant. PR Newswire (30 August 2021).
Chai, P. R. et al. DigiPrEP: a pilot trial to evaluate the feasibility, acceptability, and accuracy of a digital pill system to measure PrEP adherence in men who have sex with men who use substances. J. Acquir. Immune Defic. Syndr. 89, e5–e15 (2022).
Parkinson’s Disease: Challenges, Progress, and Promise (National Institute of Neurological Disorders and Stroke, 2023).