Seven patients (6 males and 1 female) presented with ten episodes of acute encephalopathy, and cerebral edema was present during nine episodes. One asymptomatic patient was readmitted electively as cerebral edema was noted on an outpatient MRI of the brain.
All patients had classic form of MSUD, diagnosed in the neonatal period by plasma amino acid analysis, when they were admitted with encephalopathy. The diagnosis was later confirmed by genetic analysis. Their demographic data, genetic mutations, and clinical, biochemical, and imaging profiles on admission are shown in the Table 1.. They had infrequent routine plasma amino acid monitoring. Baseline plasma leucine levels were much higher in patients with poor dietary compliance (Table 1.).
Table 1 Clinical, molecular data with biochemical and imaging profile of the patients with MSUD on admission
Respiratory tract infection and poor dietary compliance were the trigger factors for acute metabolic crises in most patients. The hospital course of these patients during acute illness is summarized as follows:
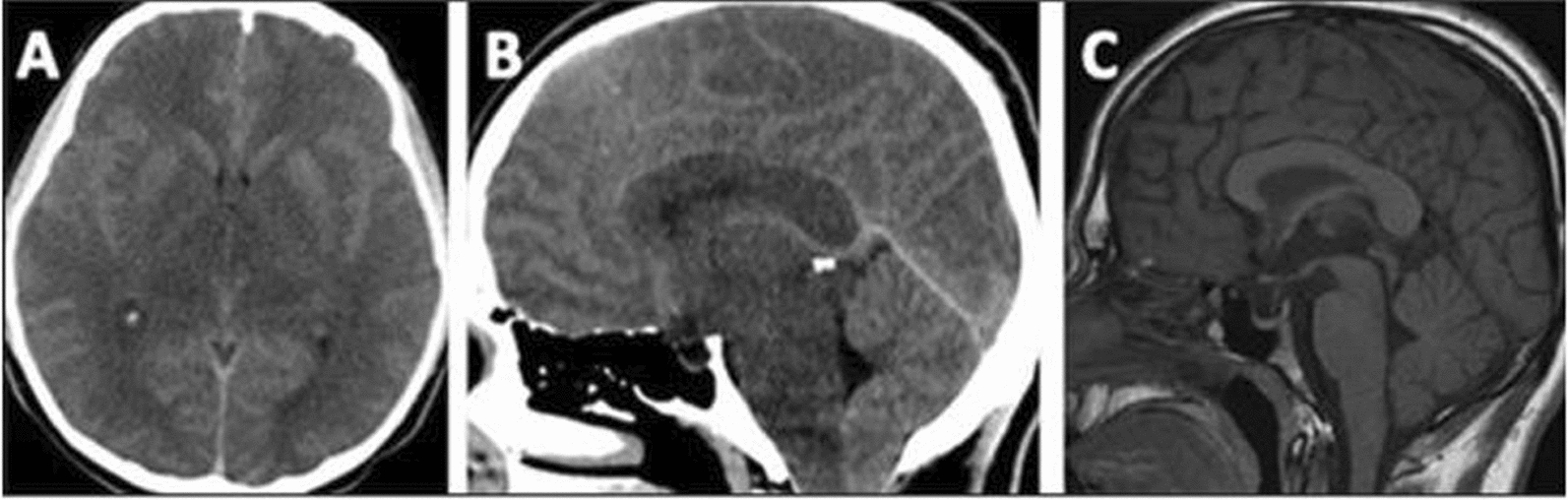
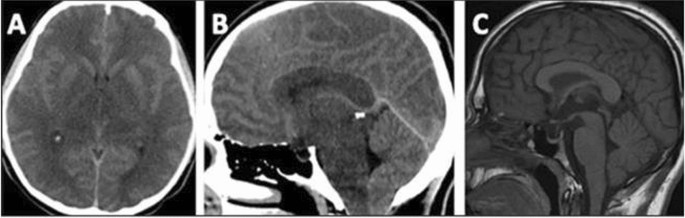
Patient 1: A 21-year-old male patient presented with nausea, vomiting, and reduced oral intake for 3 days. He looked lethargic, although fully conscious, with a GCS of 15/15. Due to poor dietary compliance, plasma leucine levels were chronically elevated (1300–1600 µmol/L) for 1 year prior to this episode. He was admitted as a case of metabolic decompensation and received conservative treatment with IV dextrose in saline infusion, BCAA-free formula and dietary natural protein restriction. The next day of admission, he had a headache and transient abnormal hand movements. A CT scan of the brain showed diffuse cerebral edema causing cerebellar tonsillar herniation (Fig. 1: A and B). He remained fully conscious with no focal neurological signs. Plasma leucine was 1300, isoleucine 237 and valine 271 µmol/L. He was shifted to the ICU and received continuous renal replacement therapy (CRRT) for 48 h until leucine levels were reduced to 400 µmol/L. Conservative management continued with hypertonic saline infusion, high-calorie intake, BCAA-free formula and valine and isoleucine supplements. He remained clinically stable and asymptomatic; however, a repeat CT scan after 5 days showed persistent diffuse cerebral edema and cerebellar tonsillar herniation.
Brain imaging of patient 1 Head-CT at the initial presentation shows diffuse brain edema (A and B), causing cerebellar tonsillar herniation (B). Sagittal T1 from the following MRI brain shows improved edema and resolution of tonsillar herniation (C)
Following discharge from the hospital, the patient developed bilateral visual impairment. His leucine levels were satisfactory (200 µmol/L). Ophthalmological examination revealed severe bilateral papilledema with a visual acuity of 20/200 in the right eye and 20/300 in the left eye. A repeat CT scan showed improvement in cerebral edema with persistent but improved cerebellar tonsillar herniation. He was prescribed acetazolamide for papilledema. Plasma leucine levels were 200–600 µmol/L in the following few months. CT brain scan after 12 weeks of the initial presentation showed further improvement of cerebral edema and resolution of cerebellar tonsillar herniation. However, his vision remained poor, which justified magnetic resonance imaging (MRI; Fig. 1C) demonstrating persistent brain edema in a distribution compatible with MSUD extending to the optic tracts. The optic nerves were mildly atrophic, with a mildly abnormal signal in the optic chiasma. His dietary compliance, which initially improved for a few months after discharge from the hospital, gradually worsened.
During the study period, he had two more admissions, one 3 years prior to this admission and another, 2 years following this admission, when he presented with nausea, vomiting, and a poor appetite. He was fully conscious with a GCS of 15/15 and was noted to have diffuse cerebral edema on CT scan on both occasions. During those admissions, he received renal replacement therapy in addition to conservative management, recovered clinically and was discharged.
Patient 2: A 19-year-old female was admitted with epigastric pain, nausea, visual hallucinations, and ataxia. Her BCAAs were high (Table). She also had acute pancreatitis as the plasma lipase was 620 IU/L (< 60). She fully recovered following conservative management. After discharge, she remained non-compliant with the protein-restricted diet. Her amino acid profile consistently showed high leucine levels (1200–1700 µmol/L) for several months, although she remained asymptomatic. An outpatient brain MRI revealed vasogenic edema in the bilateral basal ganglia, thalami, and deep white matter extending into the brainstem and cerebellar hemispheres. Her neurological examination was unremarkable. Plasma BCAA levels were high (Table 1.). She was admitted for conservative management and was discharged after four days when her leucine level improved to 600 µmol/L. An ophthalmological examination ruled out papilledema. Her follow-up BCAA levels remained in the higher range.
Patient 3: A 14-year-old male presented to the emergency room (ER) with a history of fever and reduced activity. He appeared well clinically and had unremarkable routine blood test results. He was discharged on antipyretics. The next day, he presented with a reduced level of consciousness, a GCS of 9/15 and had an episode of seizure in the ER. CT brain was unremarkable. BCAA on admission were high (Table 1.). In addition to IV fluids, BCAA-free formula, CRRT was started. Initially, there were frequent and prolonged interruptions in CRRT due to technical issues, and the leucine level was 2058 µmol/L after 48 h. There was no improvement in the level of consciousness. A repeat CT scan on the third day showed diffuse cerebral edema. CRRT continued with hypertonic saline infusion. Plasma leucine levels were reduced to 560 µmol/L when he developed fixed dilated pupils and loss of gag reflex, with confirmation of cerebellar tonsillar herniation on a CT scan. He died on the 15th day of admission.
Patient 4: A 15-year-old male patient presented with agitation, unsteady gait, and visual hallucinations, seeing “snakes on the wall” after a flu-like illness and recurrent vomiting for 3 days. His GCS was 15/15 on admission. He had not taken the BCAA-free formula for a few months. BCAA levels were high on admission (Table 1.) and CT brain showed diffuse edema. He received IV fluids, BCAA-free formula, and CRRT was initiated. He later became drowsy and required intubation and ventilatory support. On the third day, when plasma leucine was reduced to 1033 µmol/L, he developed sinus tachycardia and hypertension. He had fixed dilated pupils, with no corneal or gag reflex. CT- brain confirmed the worsening of cerebral edema with cerebellar tonsillar herniation. He underwent urgent bifrontal decompressive craniotomy but died on the 9th day of admission.
Patient 5: A 16-year-old male, the elder brother of patient 4, presented with fever and vomiting for 4 days. He was irritable and had visual hallucinations. GCS was 15/15 on admission. Plasma BCAA levels were high (Table 1.). The CT brain showed diffuse cerebral edema. He received IV fluids, BCAA-free formula and underwent hemodialysis twice with a resolution of acute symptoms. He was readmitted after two years with flu-like symptoms, irritability, headache, photophobia, visual hallucination, and unsteady gait. He received IV fluids, BCAA-free formula, and CRRT was initiated. Plasma leucine levels were reduced to 616 µmol/L in 48 h with marked clinical improvement. He was discharged in 9 days. There were no neurological sequelae.
Patient 6: A 16-year-old male presented with fever, vomiting, and confusion. His GCS was 9/15. He had an upper respiratory tract infection. The initial BCAA levels were high (Table 1.), and the CT brain showed cerebral edema. He responded well to antibiotics and conservative management, fully recovering to his baseline, and was discharged in 8 days.
Patient 7: A 28-year-old male patient with seizure disorder, spastic quadriplegia, erosive esophagitis and G-tube feeding, was admitted with vomiting, fever and drowsiness (GCS,7/15). He had aspiration pneumonia. He received antibiotics, IV fluids, and a BCAA-free formula; CRRT was initiated. Plasma leucine was reduced to 400 µmol/L with clinical improvement to baseline status, and the patient was discharged in 12 days. He was readmitted after 6 months in a state of shock, following severe vomiting and diarrhea. He was drowsy, febrile, severely dehydrated, and chest X-ray showed collapse consolidation in the left lobe. He did not respond to conservative treatment and died.