A 68-year-old woman visited the cardiology outpatient clinic for chronic chest discomfort and was diagnosed with severe aortic regurgitation on her echocardiography. Initial chest X-ray showed no evidence of pulmonary edema but revealed mild cardiomegaly. Electrocardiography demonstrated sinus rhythm with first-degree atrioventricular block at a rate of 68 beats per minute. Laboratory findings, including CBC, routine chemistry, and inflammatory markers, were all within normal limits. Cardiac enzymes were also unremarkable (creatine kinase 47 U/L, CK-MB < 0.18 mcg/L, and troponin I 0.039 ng/mL). Transthoracic echocardiography revealed a decreased left ventricular ejection fraction of 44% with global hypokinesia. The tricuspid aortic valve was thickened and uncoapted, with severe aortic regurgitation. Mild aortic stenosis was also noted (aortic valve area 1.7 cm², peak velocity 2.9 m/s, mean/peak pressure gradient 15/34 mmHg). The aortic annulus measured 18 mm, sinus of valsalva 30 mm, indicating no annular ectasia. Additionally, there was grade 1 mitral regurgitation and trivial tricuspid regurgitation. Her coronary arteries were normal without any stenosis in coronary angiography.
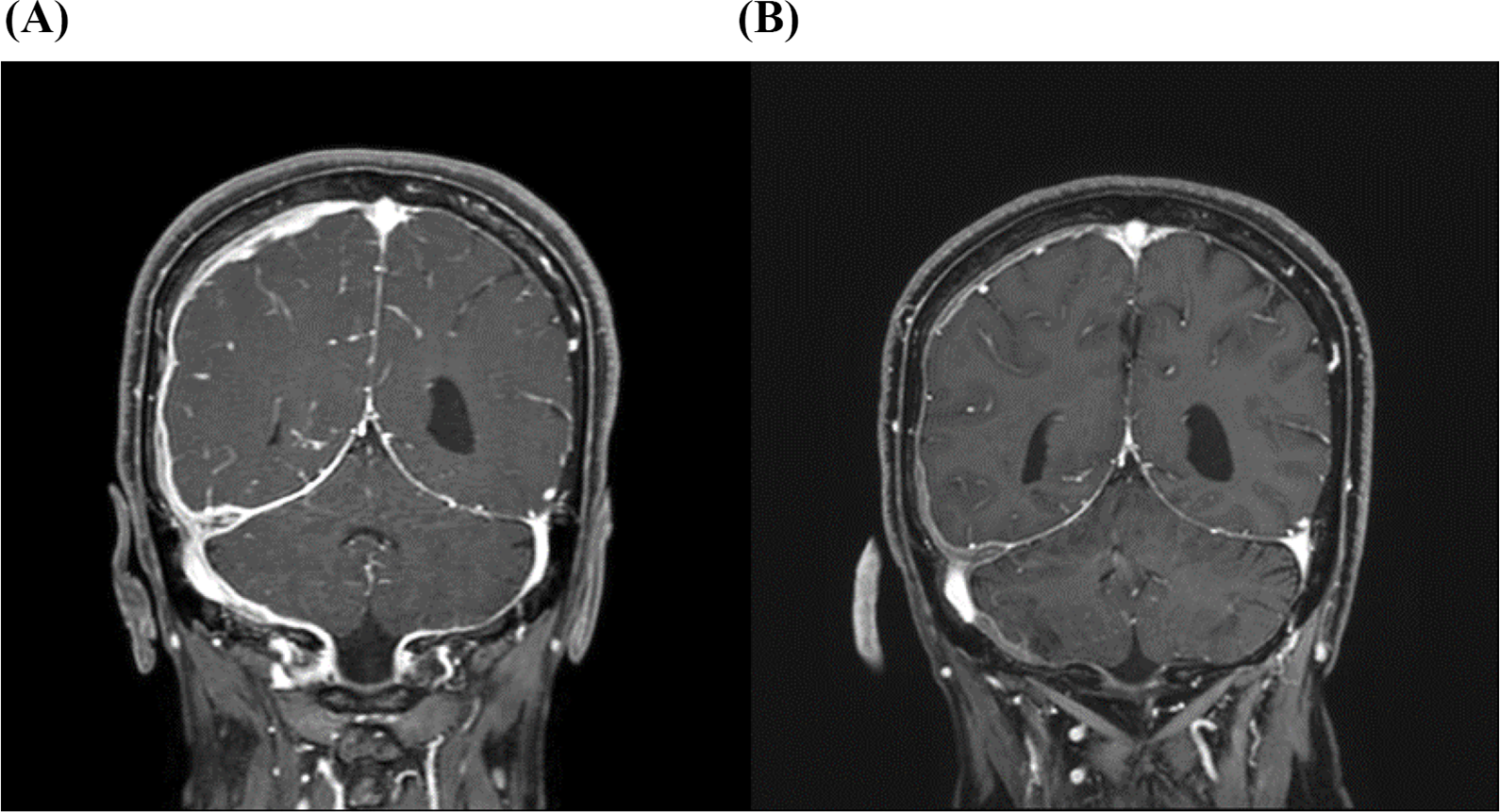
Several months prior, she had suffered from severe headache. She was admitted to the neurologist for evaluation and received steroid pulse therapy for suspected autoimmune encephalitis. Her brain magnetic resonance imaging (MRI) revealed diffuse pachymeningeal thickening and enhancement in the right cerebral hemisphere which were correlated with her symptoms (Fig. 1), and both IgG and IgG4 levels were increased in the CSF (IgG: 73.8 mg/dL; normal range [1] 0.8–3.8 mg/dL, IgG4: 30.5 mg/dL; normal range [1] 0.01–0.33 mg/dL). The patient’s symptoms improved after steroid pulse therapy, and oral methylprednisolone 10 mg daily was continued for maintenance.
The patient underwent sutureless aortic valve replacement (Sorin sutureless Perceval tissue valve #S, CE Intuity). Intraoperatively, the aortic valve leaflets showed abnormal thickening (or hypertrophy) without severe calcifications. After the native aortic valve was excised, diffuse fibrosclerosis of the subvalvular structure was observed. Histopathology revealed fibromyxoid degeneration with multifocal dense infiltration of IgG4-positive plasma cells, which are probable histologic features of IgG4-RD (Fig. 2). Postoperative echocardiography revealed a well-functioning prosthetic aortic valve, and the patient maintained a stable cardiac rhythm. (Fig. 3). There were no clinical signs suggestive of myocardial involvement during the postoperative course. The patient had previously received steroid pulse therapy during treatment for encephalitis and had since been maintained on oral methylprednisolone 10 mg daily. As there were no new issues following surgery, the same immunosuppressive regimen was continued at discharge. 12 days after surgery, the patient was discharged without any complications.
Two months after discharge, the patient was admitted to the cardiology department with syncope several times, palpitations, and occasional hypotension. Laboratory tests showed an elevated C-reactive protein level of 7.86 mg/dL(normal range < 0.5 mg/dL), while cardiac enzyme levels were within the normal range. In 24-hour Holter monitoring, paroxysmal ventricular tachycardia (VT) was observed, and an implantable cardioverter defibrillator (ICD) was inserted (Fig. 4). Two months from then, the VT recurred and the patient was readmitted, and received medical treatments including amiodarone (intravenous 150 mg loading and 200 mg bid), lidocaine (intravenous 30 mg) and beta-blockers (carvedilol 6.25 mg bid). After receiving medication, which improved symptoms and stabilized rhythm, the patient was discharged while taking a beta-blocker. However, just two days after discharge, the patient was admitted to the emergency room for chest discomfort, and the electrocardiogram showed sustained VT with an HR of 180 bpm/min. Even after medication control with amiodarone and repeated electrical cardioversion, VT persisted and the patient eventually underwent radiofrequency catheter ablation (RFCA). Following a recurrence of arrhythmia, the patient was readmitted under cardiology care, and additional immunosuppressive therapy was initiated. Four years after then, the patient remains stable without further episodes, maintained on oral methylprednisolone (Solondo) 5 mg daily and azathioprine (Immuthera) 50 mg daily. At the time of the initial diagnosis of encephalitis, both serum and cerebrospinal fluid (CSF) IgG4 levels were elevated. However, a subsequent evaluation by the rheumatology team revealed no elevation in serum IgG4 levels, and chest and abdominal CT scans showed no definitive evidence of other organ involvement. The patient is currently being managed conservatively with low-dose steroids and close clinical follow-up. There has been no recurrence to date.