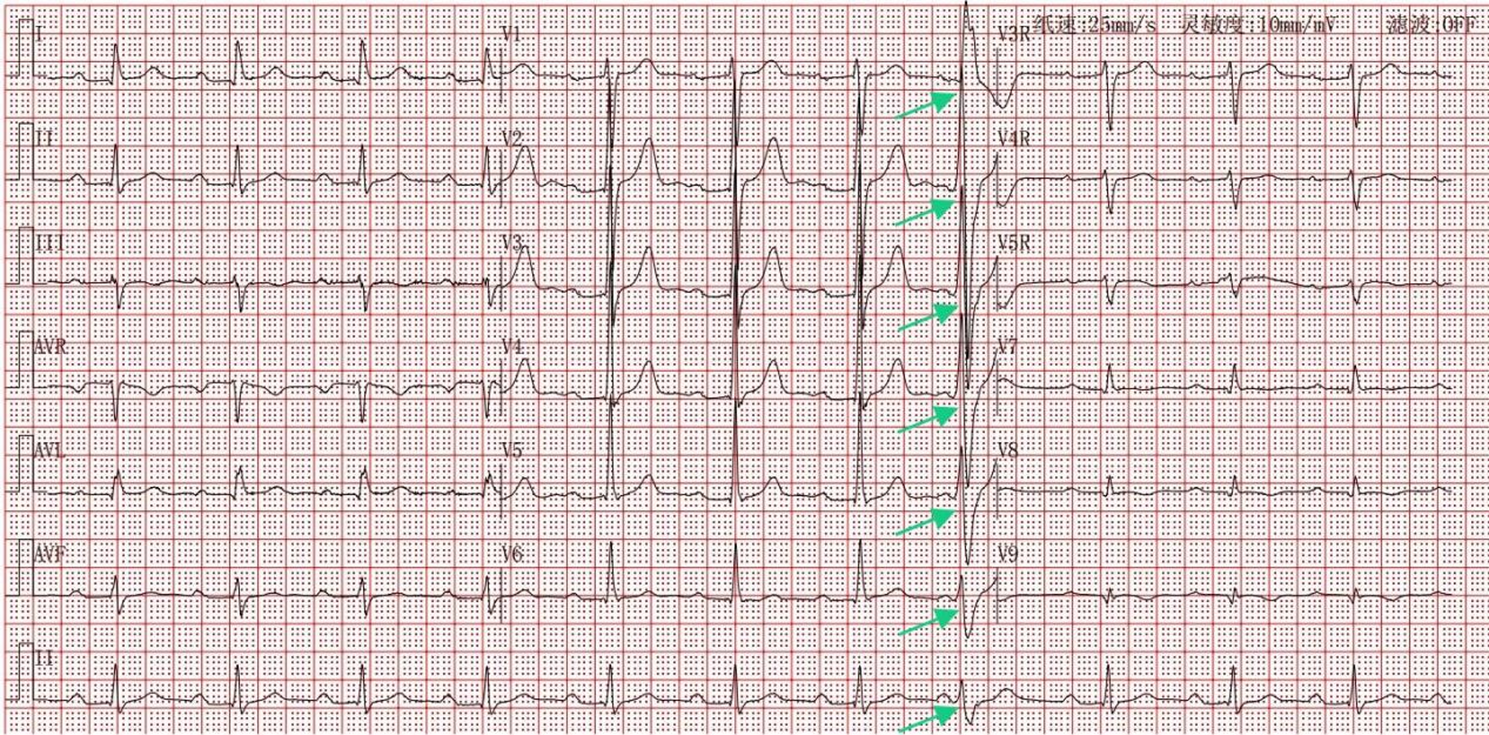
Herein, we presented a middle-aged man with a giant extensively calcified pseudoaneurysm, suffering from recurrent chest pain. Cardiac examination and imaging techniques have both confirmed the presence of left ventricle enlargment with reduced ejection fraction. Notably, this patient’s LVP was not caused by typical transmural myocardial infarction, a unique feature. Based on electrocardiogram, echocardiography, CMR, and coronary angiography, a silent antecedent myocardial infarction in the absence of obstructive coronary artery disease (MINOCA) is highly suspeceted as the underlying cause. Surgery directly confirmed inferolateral wall rupture and a calcified pseudoaneurysm.
To our knowledge, similar cases are extremely rare. Naseerullah FS et al. reported a similar case of an elderly woman with nonobstructive coronary artery disease, a history of embolic stroke, no antecedent myocardial infarction, who was hospitalized for intermittent chest pain and diagnosed with LVP, ultimately undergoing surgical repair [9]. Unlike our case, her LVP was apical and had no thrombus due to pre-admission anticoagulation. The insights gleaned from our case have broaden our understanding of chronic giant LVPs management.
Firstly, despite the risk of sudden cardiac death, patients affected with LVP could be hemodynamically stable. The most common symptoms are chest pain, dyspnea, and congestive heart failure [2], less frequent are systemic embolization and symptomatic arrhythmia. Occasional nonspecific discomforts include shoulder, back, or arm pain, hemoptysis, and altered mental status. Yet, asymptomatic LVPs exist, with a reported incidence of 12%−48% across case series [2, 10].
In this case, the patient initially presented with recurrent chest pain, which was not significantly relieved by anti-anginal drugs including nitrates and nicorandil after admission. In other words, the chest pain was atypical. Coronary angiography excluded residual significant lesions; instead, it was more likely due to adjacent tissue compression and stimulation by the expanding pseudoaneurysm, as reported in the literature [11, 12].
Another important finding is extensive thrombosis in the false cavity, raising concern about systemic embolism. The patient had a stroke 2 years pre-admission, with local secondary hospital outpatient cranial CT and magnetic resonance imaging showing acute right cerebral peduncle infarction. No ambulatory electrocardiogram or echocardiography (with or without bubble test) was performed then, precluding confirmation of systemic embolism. The patient has since been on regular aspirin and statins. From a monistic perspective, embolism is strongly suspected as the etiology underlying the patient’s prior stroke.
A few studies have elaborated on anticoagulation in this context [2, 13]. For conservatively treated LVPs, the reported 1-year ischaemic stroke incidence was 10%, rising to 32.5% at 4 years [14]. These figures support considering anticoagulation to prevent systemic embolism, despite theoretical risks of complete rupture and bleeding. A similar case described by Naseerullah FS et al. illustrated this clinical dilemma: a patient with embolic stroke was found to have a large mobile left ventricular thrombus during diagnosis, and following standardized anticoagulation therapy, repeat TTE demonstrated complete thrombus resolution but newly identified LVP [9]. In the absence of sufficient evidence to support or refute the use of anticoagulation, clinicians should therefore make decisions tailored to the individual patient’s condition [9, 13].
In the specific context of this case, current consensus on MINOCA notes controversial use of antiplatelet agents except for plaque disruption-related cases [15]. Given the probable embolic etiology of the patient’s stroke and planned surgery, pre-operative anticoagulation rather than antiplatelet therapy was reasonable. However, concern about complete rupture outweighed the benefit of thromboembolism prevention, anticoagulant treatment was ultimately withheld.
A final crucial point is that surgical indications and optimal timing for asymptomatic or stable chronic LVP remain undefined. Generally, LVP is classified by time from AMI onset as acute (within 2 weeks), subacute (from 2 weeks to 3 months) and chronic (beyond 3 months) [1, 16]. This classification helps predict patient outcomes and guide treatment decisions. For clinicians, key factors in surgical decision-making are the risk of fatal rupture associated with conservative treatment and surgical mortality [1, 14].
The long-term mortality rate for patients with medically treated LVP reached as high as 60%, as indicated by a small Mayo Clinic cohort study [10]. Notably, none of the deaths were due to cardiac rupture, consistent with findings in another small cohort of conservatively treated LVPs [14]. A review of 290 LVP cases showed that the mortality of medically treated patients was 48% within first week [2]. However, those surviving the early days had a median survival of 156 weeks.
Generally, the risk of complete rupture is associated with timing from AMI onset and pseudoaneurysm morphological features. Large LVPs or those developing within 3 months post-AMI are considered high rupture risk; in contrast, small chronic LVPs (< 3 cm) with heavily fibrotic edges have low rupture risk [1, 3]. Furthermore, the coexistence of impaired cardiac function or systemic embolism indicates a poor prognosis [1, 14]. Whether the optimal medical therapy that’s proven effective in heart failure patients exerts the same effect in heart failure complicated with large LVP remains uncertain.
The surgical mortality varied in different case series, ranging from 7% to 35.7% [10, 17, 18], and increasing further when accompanied by mitral valve replacement [2]. Limited studies suggest a correlation between surgical timing and surgical mortality risk. One study of 45 patients undergoing surgery for myocardial infarction-induced LVP showed that acute-phase surgery was associated with significantly higher in-hospital mortality than non-acute-phase surgery (15.6% vs. 61.5%, p = 0.0066) [16]. Since the first successful percutaneous closure of LVP reported in 2004, percutaneous approaches for anatomically suitable LVP patients has emerged as a feasible and safe alternative to sugical repair [19].
In this chronic LVP case, surgical risk is significantly lower than in the acute phase. Its anatomical features—large aneurysm, marked calcification, and proximity to basal segments—make traditional surgery preferable to percutaneous closure as the optimal treatment. These features also influence surgical techniques [20]. Chronic LVPs typically have calcified and fibrous edges, allowing direct neck closure with pledgeted sutures. Given its large cavity and basal location, a bovine pericardial patch was utilized to restore normal left ventricle geometry and avoid excessive traction of the subvalvular apparatus [20, 21]. In concomitant mitral valve replacement, internal LVP repair via the left atrium is preferred for better exposure of the sub-valvular apparatus [1, 22].