Reasoning behind the evaluation of leachable compoundsOff-label use of plastic syringes in batch compounding
In a hospital setting, the selection of primary packaging for batch production, such as syringes, infusion bags, vials, and elastomeric pumps, is important when patient care is involved. In this case, syringes are used to contain compounded intravitreal chemotherapeutic drug products such as TPT. In addition to specific reports of excess silicone oil in the medical field, there has been an ongoing trend of off-label use of plastic primary packaging in hospital pharmacy batch compounding10,33,34,35,36,37,38,39. Immediate to short-term use of plastic syringes is being used in the production of long-term, ready-to-administer PFS for storage. This could represent toxicological issues because these syringes have been accounted for only as immediate-use medical devices based on risk assessments performed by the manufacturer, which makes them safe to use as labelled on the container’s technical sheets. Manufacturers such as BD and BBraun have performed assessments to ensure population safety if their containers are used as intended. However, the storage of filled devices beyond their approved use can lead to the release of unmonitored, potentially harmful, leachable compounds11.
Adoption of medical device regulatory logics in hospital pharmacy compounding
According to the European Union Medical Device Regulation (EU MDR) and the FDA 510(k), immediate- to short-term use syringes are considered Class 1 syringes because of their low-risk functions; these syringes are used directly in medical wards for general purpose aspirations and the withdrawal of fluids such as diluents, drug products, and body fluids. According to these regulations, industries are obliged to use Class 2 and 3 syringes as long-term storage container closure systems (CCSs) based on good practices for safety of the general population40,41. These regulations do not serve hospital pharmacy productions and therefore do not oblige hospital pharmacy compounders to do so. However, industry-based regulatory logic is based on solid scientific data; therefore, hospital pharmacy compounders are inclined to follow regulations to ensure optimal patient safety. MDR regulations state that the intended purpose of a container must align with the data and conclusions generated for the container.
In this context, it would be interesting to show potential leachables in syringes used off-label in the form of case studies to increase awareness by using an analytical method built for assessment of leachables by hospital pharmacies. By considering the risk assessments of leachables studies, hospital pharmacists can advise on safe use in terms of toxicology and clinical risks for patients11,17,18.
Risk-based approach
According to most extractables and leachables (E&L) experts, the typical E&L protocol is long and expensive to perform in industry, involving a full extractable study on the medical device and then a leachable study on the combined container closure system (CCS) (medical device and drug formulation) based on guidelines40,41,42,43,44,45,46. In response, many industries are proceeding towards simplifying the E&L procedure. If hospital pharmacies are to perform risk assessment of their batch products, they would do best to adopt a similar approach. A risk-based approach in hospital pharmacy leachable assessment should be composed of different variables: route, frequency and duration of administration, type of patients, and formulation. TPT PFS can be considered a medium-risk product because it not only uses an off-label medical device but is also used for parenteral administration to frail and vulnerable patients, such as infants11. This approach would also include an estimative quantification with an estimative toxicology. All the analytical procedures and a comprehensive toxicological assessment are expensive, demanding high cost and time, which makes this approach necessary as a means of first-step measurement. Moreover, this estimative approach underestimates the value, making the toxicological threshold value of a given compound in exposure to the patient lower, adding an extra layer of protection for frail and vulnerable patients such as neonates and infants that are physiologically different from those of the general adult population.
Materials for the construction of syringes used in hospital pharmacy compounding
Both BD Plastipak and BBraun Omnifix 1 mL syringes consist of a barrel made of polypropylene and a plunger head made of isoprene rubber. The barrel has a black graduation scale printed with ink on its surface to enable estimation of volume measurement of aspiration and withdrawal of liquid. The plunger head and the inner surface of the barrel are sprayed with PDMS medical-grade lubricant to facilitate smooth movement of the plunger20,21,22,23,24. Additionally, a label is affixed to the barrel to allow product distinction once the syringe is filled with the drug product to become a CCS but does not possess a low extractable profile quality.
Leachable studies
Three batches of TPT in BD Plastipak and BBraun Omnifix were analysed at six different time points, i.e., initial, 4 h, 72 h, 1 month, 6 months, and 12 months, at a refrigerated temperature, which was deemed the appropriate storage condition for this product on the basis of a conducted stability study10. There are two parts to this study: the first is the evaluation of leachables at the product expiration date, which is 12 months, to study the outcome of leachable compounds in these two common syringe types, and the second part is the monitoring of only lubricant-related compounds and their degradants at all time points to study the trend of degradation for these two syringe types.
Tables S1-4 compile the leachable compound data observed in both syringes, including identification methods, retention times, m/z values and adducts, and semiquantitative concentrations as well as toxicological assessment data, are in the supplementary material.
Evaluation of leachablesIdentification of leachables and functional implications
After 12 months of storage, both syringes presented similar patterns of leachable compounds, all of which were observed at low concentrations (between 0.1 and 15 ng/mL). BD Plastipak produced three times more diethylhexyladipate (DEHA) than did BBraun Omnifix. This could be due to the medical device formulation. DEHA is an important plasticizer that is responsible for ensuring flexibility in primary packaging and preventing brittleness47. It is fused with the polymer before extrusion through van der Waals interactions. Due to this weak bonding, DEHA compounds are easily removed by aqueous solutions, which explains the observed concentrations. Moreover, two other plasticizers were observed at very low concentrations only in BD Plastipak (sebacate and citrate derivatives).
Degradants of antioxidants were observed in both primary packages (i.e., 2,6-di-tert-butyl-4-hydroxy-4-methylcyclohexa-2,5-dien-1-one, 2,6-di-tert-butyl-p-cresol, 3-(3,5-di-tert-butyl-4-hydroxyphenyl)propanoic acid, 3-(3-5-di-tert-butyl-1-hydroxy-4-oxo-2,5-cyclohexadiene-1-yl)propanoic acid, and 3,5-di-tert-butyl-4-hydroxybenzyl alcohol). All these compounds are derived from 2,6-di-tert-butyl-p-cresol (BHT) and 3-(3,5-di-tert-butyl-4-hydroxyphenyl)propanoic acid (fenozan). BHT may be a small standalone antioxidant or a part of a more complex structure and fenozan is part of a larger structure (i.e., Irganox 1010, 1076, etc.). According to our observations, BD Plastipak released three times more of fenozan than BBraun Omnifix, which could be due to the presence of either more complex antioxidants or the instability of the polymer due to long-term storage. However, BBraun Omnifix syringes released the greatest number antioxidant derivatives. There could be a higher oxygen content in the drug formulation, which induced the oxidation of fenozan and BHT into their oxidated states (hydroxy, aldehyde, ketone), related to the porosity of the material.
Markers of rubber deterioration were also observed in BD Plastipak syringes. These compounds are rubber cross-linkers used in the curing of rubber. Usually, rubber plunger heads are thermoplastic elastomers and therefore should not require rubber crosslinkers, which would be more appropriate for thermoset elastomers. Nevertheless, low concentrations of rubber cross-linkers were observed at 12 months of storage.
Ink graduation markers were observed in both syringes. BBraun Omnifix has shown traces of acrylate derivatives (triethyleneglycol dimethacrylate) and caprolactam at low concentrations, whereas BD Plastipak released twice as much caprolactam than BBraun Omnifix. Moreover, bisphenol A (BPA) and phosphate flame retardants (triphenyl phosphate and tris(2-chloro-1-methylethyl) phosphate) were observed in greater amounts in BD Plastipak than in BBraun Omnifix. BPA was not found in the latter, but this would require more interbatch analysis to confirm its presence since it can appear in one batch and not another. Flame retardants have no place in syringes since their role is to prevent the spread of fire through electric cables and equipment. These compounds, including BPA, could result from industrial in-process contamination17,18.
Estimative toxicology of leachables
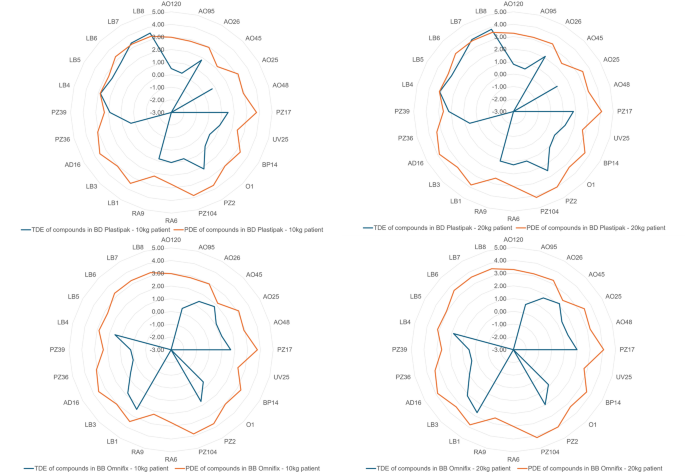
To estimate the risk of critical patients being exposed to potentially hazardous compounds, it is important to first determine the MDD of TPT, which is calculated at 1 mL, since it is administered only intravitreally or intracamerally during surgery. Next, PDE and TDE were calculated according to Eq. 3 and Eq. 5 for nonlubricant leachables. As a result, none of the TDEs of the identified compounds related to leachables surpassed their PDE thresholds, as shown in Fig. 1. DEHA was nearly the highest in concentration; however, many E&L experts say that this is normal. According to some toxicologists, DEHA can be viewed to be toxic with multiple endpoints, such as neurotoxic, hepatotoxic, and cardiotoxic, and a potential endocrine disruptor compound (EDC) of concern if infant patients are involved in the treatment48. More tests are needed to determine the safety of patients when exposed to off-label containers that have been used to store high-risk products.
Chromatograms and mass spectra in positive and negative modes are available in Figs. S1-S13 in the supplementary materials.
Risk assessment of topotecan PFS stored in BD Plastipak and BB Omnifix primary packaging after twelve months in refrigerated temperature. The compounds (along with the laboratory codes) identified, semiquantified and assessed are: 2,6-di-tert-butyl-4-hydroxy-4-methylcyclohexa-2,5-dien-1-one (AO120), 2,6-di-tert-butyl-p-cresol (AO95), 3-(3,5-di-tert-butyl-4-hydroxyphenyl)propanoic acid (AO26), 3-(3-5-di-tert-butyl-1-hydroxy-4-oxo-2,5-cyclohexadiene-1-yl)propanoic acid (AO45), 3,5-di-tert-butyl-4-hydroxybenzaldehyde (AO25), 3,5-Di-tert-butyl-4-hydroxybenzyl alcohol (AO48), Acetyl tributyl citrate (PZ17), Benzotriazole (UV25), Bisphenol A (BP14), Caprolactam (O1), Di-(2-ethylhexyl) adipate (PZ2), Di-(2-ethylhexyl) sebacate (PZ104), N, N-Dibutylformamide (RA6), N-butylformamide (RA9), Oleamide (LB1), Tetradecanamide (LB3), triethyleneglycol dimethacrylate (AD16), Triphenyl phosphate (PZ36), Tris(2-chloro-1-methylethyl)phosphate (PZ39), hexamethylcyclotrisiloxane (LB4), octamethylcyclotetrasiloxane (LB5), decamethyltetrasiloxane (LB6), decamethylcyclopentasiloxane (LB7), dodecamethylpentasiloxane (LB8).
Monitoring of lubricant-related compounds and their degradants
Six different time points—initial, 4 h, 72 h, 1 month, 6 months, and 12 months—were considered at refrigerated temperature, which was deemed the appropriate storage condition for this product based on the stability study10.
As mentioned in section “ Leachable studies”, Tables S1-4 compile the leachable compound data observed in both syringes, including identification methods, retention times, m/z values and adducts, and semiquantitative concentrations, as well as toxicological assessment data, and are in the supplementary material.
The monitoring of lubricants via a UHPLC-HRMS platform is challenging in terms of compound detectability and, to our knowledge, has not been attempted before due to instrument incompatibility. However, with the installation of PCI, as described in section “Post-column infusion (PCI)”, it is possible to identify and estimate the concentrations of some silicone degradants or oligomers. The main objectives of this study were twofold: (1) identify any non-silicone-related lubricants and any silicone-related degradants and (2) evaluate the toxicological risk of these compounds after long-term storage in patients for intravitreal administration to treat retinoblastoma.
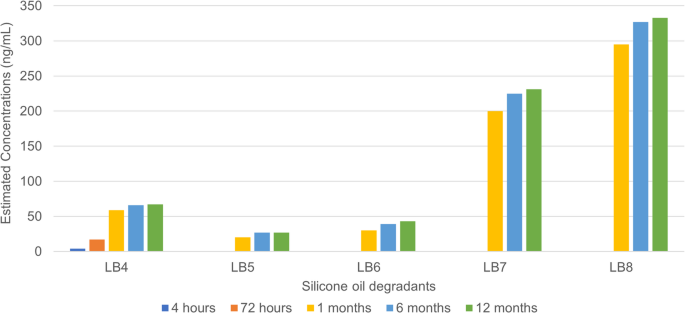
The release of silicone-based degradant/oligomers evolving in terms of estimated concentrations at different time points over a period of 12 months in the BD Plastipak. The compounds (along with the laboratory codes) identified, semiquantified and assessed are: hexamethylcyclotrisiloxane (LB4), octamethylcyclotetrasiloxane (LB5), decamethyltetrasiloxane (LB6), decamethylcyclopentasiloxane (LB7), dodecamethylpentasiloxane (LB8).
Identification of lubricant-related compounds
As illustrated in Fig. 2, five different silicone-related degradants were identified in the BD Plastipak syringe, and their concentrations were estimated to range from 4 to 300 ng/mL after 12 months of material‒solution contact. The concentration of these oligomers tends to increase slowly over time because of their instability in aqueous solution, especially when the device is not meant to be used as a storage device for more than 72 h, reflecting the quality of the silicone oil lubricant. From the initial time point to 72 h, little to no detectable presence of silicone-based oligomers was observed within the sensitivity limits of our analytical platform. The concentrations of these silicone-based oligomers are potentially too low to cause toxicological issues for patients of all ages, including infants and neonates for short-term use of these syringes for up to 72 h, which are labelled and strongly advised by the manufacturer, for all intents and purposes. However, as these syringes are used outside their regulated boundaries, an increase in the concentration of these oligomers is observed after 6 months, which is to be expected, especially with LB7 and LB8 having higher estimated concentrations than the rest. The increase in the concentration of all oligomers could be related to a small volume effect. Interestingly, at 6 months, an exhaustive asymptotic curve is observed, forming a plateau when the syringes are left in storage for 12 months. The stagnation appears after 6 months for all oligomeric silicone degradants, which is due to the equilibrium between the PDMS polymer and the oligomeric degradants. This reflects the solubility of the oligomers of interest and the tendency of PDMS to break down into oligomers due to steric hindrances and other molecular stresses. This depends on the angle of attack, which results in the formation of cyclic and linear silicone degradants. There was a four- to seventeen-fold increase between the initial filling in primary packaging and after twelve months of storage.
To understand slightly more about silicone oil, or PDMS, it is a popular lubricant used to enable frictionless surface transition between two objects. PDMS is a low-density polymer composed of silanol monomers. However, since they are linked by silanol bonds, they could be prone to hydrolysis when in contact with aqueous solution. When these bonds break oligomers, either linear or cyclic structures are formed and tend to leach into the drug solution49.
The identified degradants are siloxane and silane in nature and were detected in ESI positive mode as [M + H]+ adduct. The identification of silicone derivatives via UHPLC-HRMS is particularly unusual because these compounds are volatile to semivolatile by nature. However, the design of the current instrument layout enabled the identification of some siloxanes and silanes due to the installation of a PCI using ammonium hydroxide (NH4OH) at very low concentrations and at low flow rates17,18. It is hypothesized that the PCI transforms the ion source by creating an environment rich in proton and ammonium molecules, forcing the creation of adducts of silanol and siloxanes substances.
With respect to possible container‒content interactions, describing any interaction with a TPT drug formulation is difficult. It is not known if leachables interact with topotecan and its excipients until we observe signs of physical‒chemical phenomena, which are related to incompatibility between the drug formulation and the medical device. All we can do is describe the presence and concentration of leachables in the solution that may end up in the patient’s bloodstream via means of treatment. However, one good observation is that, on the basis of the results of the TPT stability study, TPT concentrations were not significantly affected since we established that they remained stable for 12 months in BBraun Omnifix Syringes and BD Plastipak Syringes.
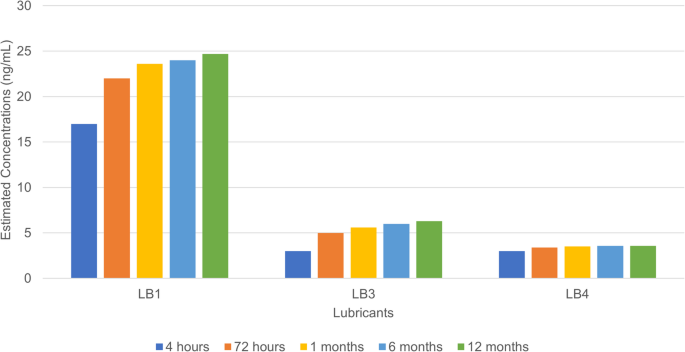
The release of oleamide and its degradants as well as silicone-based oligomeric contaminant evolving in terms of estimated concentrations at different time points over a period of 12 months. The compounds (along with the laboratory codes) identified, semiquantified and assessed are: Oleamide (LB1), Tetradecanamide (LB3), Hexamethylcyclotrisiloxane (LB4).
For BBraun Omnifix, as shown in Fig. 3, small concentrations of oleamide (LB1) were observed after 4 to 72 h of contact with the solution, i.e., between 20 and 25 ng/mL. The oleamide degradant tetradecanamide (LB3) was identified and semiquantified at concentrations less than 5 ng/mL. Oleamide degradation is usually linked to its intrinsic quality and is not related to in situ reactions with aqueous drug solutions. There was no further increase in concentration after 4 h. Oleamide and its degradant are lipophilic by nature50,51. This small molecule is an oleic acid derivative with an amide functional group that renders the molecule inert to acidic and basic compounds. Its original purpose was to serve as a slip agent; it is added at a small concentration during the moulding phase of the medical device and remains incorporated into the polymer, which explains its presence in the drug formulation. As an alternative to silicone-based lubricants, oleamide can be a very interesting choice for use in syringes and vials containing aqueous medication. It requires small concentrations to perform optimally as a lubricant50,51. Although it was identified at a small concentration, it was never added to the technical sheet because it served no purpose as a lubricant, and it has been assessed by E&L experts as safe before market release. After 12 months of storage, there was a negligible increase in oleamide concentration of approximately twofold. A silicone-related degradant called hexamethylcyclotrisiloxane (LB4), which comes from silicone oil as part of lubrification, was also detected.
The observation of oleamide in BBraun Omnifix syringes is particularly interesting since both syringes are sprayed with free silicon oil on the barrel and the plunger head52,53. According to our observations, the spraying technology of free silicone oil in BD Plastipak may differ from that of BBraun Omnifix. The former may have contributed to the added presence of silicone oligomers. It is even possible that there may be less free silicone oil sprayed in BBraun Omnifix, which makes sense when oleamide, which is already incorporated in rubber, is used as a secondary lubricant, hence reducing the reliance on silicone oil.
Estimative toxicology of lubricant-related compounds
In terms of risk assessment, as shown in Fig. 1, the only compounds whose TDE surpassed its PDE appeared to be decamethylcyclopentasiloxane (LB7) and dodecamethylpentasiloxane (LB8) at 1 to 12 months of batch storage, which could be considered nonrecommended for long-term contact exposure between this syringe and the drug formulation. Judging by the trend on the histogram shown in Fig. 2, the start of saturation seemed to be visible at the 1-month time point. Unfortunately, to clarify further, it would have been optimal to possess data at the 72-hour time point, but due to the high LODs for these compounds, the concentrations of LB7 and LB8 were not measurable and no models were constructed using their standards to estimate concentrations lower than their LODs. However, it is assumed that their concentration would be much lower than that at the 1-month time point since the lubricant is of medical grade and does not easily degrade when in contact with the formulation for less than 6 days. Importantly, Class 1 syringes are labelled for acute use for simple actions and, in the worst case, for short-term storage for up to 72 h. Therefore, their use for longer than 72 h, from 1 month to 12 months, for example, would not be recommended for infant patients. The other silicone degradants (LB4, LB5 and LB6) were found at relatively low concentrations, which put their TDEs below their PDE after 72 h, up to 12 months. Although syringes seem safe for use in adults, the use of these syringes in infant patients after 72 h of batch storage of medium- to high-risk compounding formulations, such as the current compounding PFS, it strongly discouraged.
In contrast, for BBraun Omnifix, although it may also seem to be a container misappropriation, it did not surpass the TDE-PDE threshold. There has been very little evolution of oleamide (LB1) and its degradant, tetradecanamide (LB3). In terms of safety risk assessment, none of the TDEs surpassed their PDE thresholds, which appears to be safe for use for up to 12 months. The use of only a silicone-based oligomeric degradant was also estimated to be safe because the TDE of the compound did not surpass its PDE threshold. Tables S3 and S4 compile the leachable compound toxicological data observed in both syringes in the supplementary material, including TDE and PDE.
In conclusion, BBraun Omnifix could be a good fit to condition TPT as a PFS, but would it be appropriate for long-term storage? More tests are needed to determine its safety to ensure that no potentially harmful entities can cause issues in frail and vulnerable patients. Moreover, the migration of free silicone oil can be the cause of floaters being injected into patients’ eyes. The appropriate use of primary packaging should be encouraged to reduce incidence, and the promotion of an E&L-related risk assessment should be undertaken to assure patient safety11,14,15.
Endocrine disruptor identification
Ten potential EDCs were identified in BD Plastipak (AO95, PZ17, UV25, BP14, PZ2, PZ36, PZ39, LB4, LB5, and LB7) in comparison to six in BBraun Omnifix (AO95, PZ17, PZ2, PZ36, PZ39, and LB4), nearly half the amount of the former. Although some of these compounds are found at low concentrations, EDCs are particular compounds that do not follow regular toxicology; they can have toxicological effects on the growth and development of younger patients, especially at low concentrations54. The compounds that contributed to the increase in EDCs in the BD Plastipak syringes were silicone-based oligomeric degradants. In contrast, BBraun Omnifix did not seem to release many EDCs because of the low contribution of lubricant-related compounds. All EDC information is compiled in Tables S3 and S4 in the supplementary information.
Limitations
It is essential to address several key limitations in analytics, toxicology, and comparative studies in this paper as these can significantly impact the reliability and interpretation of research findings.
Analytical limitations
First, monitoring volatile, semivolatile, and nonvolatile leachable compounds would be ideal for this type of study because of the level of risk of exposure to frail and/or vulnerable patients, such as infants. The current analytical method uses a fixed list of 200 commonly observed compounds, that are of toxicological concerns; therefore, compounds that are not listed cannot be assessed, which is part of the limitation of the method, and its semiquantitation method allows its user to estimate the compounds that are listed in the database. However, the silicone-related compounds were estimated with a larger margin of error as an estimation. It tends to overestimate the concentration because of the selection of the IS used. Moreover, silicone degradants were identified, and their concentrations were estimated via PCI-integrated LC‒MS. Due to the limitations of the instrument, not all degradants were identified; therefore, analysis via GC‒MS would have been an optimal method for analysing volatile and semivolatile compounds. Furthermore, it is concerning that any presence of oligomers could be related to interbatch variation. Silicone degradation can vary from batch to batch, which is why E&L must be performed. Finally, leachable assessments of other storage conditions (RT and freezing temperature) of the TPT PFS were not conducted. If this is done properly, it would yield multidimensional results, establishing the influence of temperature on the release of leachables and even their stability.
Toxicological limitations
A full toxicological assessment would have been adequate for this type of study. However, this approach could demand greater cost and more time to establish, which makes this current approach necessary as a means of first-step measurement.
Comparative study limitations
Finally, TPT conditioned in syringes made of COP and COC could have been used as a comparison to the other two syringes to demonstrate the low-extractable profile marketed and recommended for long-term storage of DPs17,18. However, there was also an intention to demonstrate case studies of off-label use of primary packaging. A glass syringe would have been the optimal control sample. While glass syringes are more inert, their use in ophthalmic surgery and other interventions is contraindicated because of the risk of ocular trauma from glass particles and plunger malfunction. There are many inconveniences due to the high degree of breakage and risk of particulates.
Expert opinionsThe use of appropriate primary packaging material
The off-label use of plastic primary packaging, including syringes, should not be underestimated. Both syringes tested herein, and many others that are not mentioned in this paper have already been assessed by manufacturers to be safe for use as intended as per their label, which is for simple aspiration and withdrawal of fluids, whether it is a drug formulation, a diluent, or even a biological fluid. Therefore, these items should not be used outside of their approved use for safety reasons. Industrial drug products intended for long-term batch production are conditioned in primary packaging materials that have been previously risk assessed by industrial E&L experts to ensure optimal patient safety for product market access. Therefore, as an expert opinion, hospital pharmacy compounders should consider doing the same for future endeavours. A recommendation to hospital pharmacy compounders would be the use of Class 2 and 3 syringes made of COP or COC, which are better suited for all drug formulations, including sensitive drug delivery, such as biologics and ophthalmic drug formulations, featuring low extractables and low silicone particle burden40,41,55,56. Melo et al. reported that there is often a lack of intraocular primary packaging available, forcing medical institutions to use syringes with free silicone oil. COC- and COP-made syringes could be optimal candidates and result in smaller volumes for low-volume administrations14,15,55,56,57.
Promotion of leachable assessment
Another point to recommend would be leachable risk assessment in hospital pharmacy batch compounding. Any off-label use of Class 1 syringes could be safe for adults, but probably not for infants or neonates. As an expert opinion, it would be ideal to perform a risk-based approach on medium- and high-risk drug products. The degree of risk should be based on the route of administration, the type of patients, the type of formulation, the selected medical devices, the frequency of administration, and the duration of treatment. This could be set up in the form of a workflow that could be adaptable, standardizable, affordable, and applicable for hospital pharmacy compounding practices11.
If off-label primary packaging is used because the appropriate packaging is deemed too costly to implement in hospital pharmacy production, it is good practice to at least perform an extractable study to ensure that batch-produced products are safe for use in frail and vulnerable patients. Although no regulation exists that obliges compounders to assess the E&L-related risk of PFS, compounders are ethically and morally liable to ensure a safe product for patients.
If appropriate packaging, such as a COC or COP syringe, is implemented in a hospital pharmacy batch compounding to bring about a PFS product to patients but it is too costly to perform a complete risk assessment, compounders can request a technical report issued from E&L studies from the manufacturer. The results can be used as a basis for the compounder’s product to estimate the safety of the product. In terms of extra safety measures, an extractable study can always be performed on the medical device, which does not cost as much as a full assessment.