AM and CAM were uncommon but severe complications of AOM, particularly in children. To date, no universally accepted guidelines are available about the appropriate diagnostic and therapeutic workout [8, 14]. Thus, the management of AM or CAM may consistently depend on the available professional specialties in a certain hospital and on the physicians’ experience.
In this context, our study aimed to share our experience at an Italian third-level pediatric university hospital in managing AM and CAM. Secondly, we aimed to compare our findings with those reported by the current literature, as the incidence of AM and CAM have been increasing after the SARS-CoV-2 pandemic period [15, 16].Notably, we found a higher median age at admission than the literature reported. Several studies reported a median age of 2 years [2, 3, 13, 14], whereas we found a median age of about 4 years. This finding may be explained by the enactment of the Italian guidelines provided in 2019 recommending immediate antibiotic therapy in children < 2 years old diagnosed with AOM and a wait-and-see strategy for older ones [17].
Consistently to the current literature, the diagnosis of AM was essentially driven by signs and symptoms, in particular, the presence of swelling, erythema, and tenderness of the retroauricular region with or without the protrusion of the auricular pinna was robustly associated with an AM diagnosis [8, 18]. In contrast, CAM diagnosis may be challenging when considering clinical features alone, as most patients were initially admitted for neurological disorders [6]. Hence, an otological origin should not be underestimated in a child complaining of a neurological disorder and a history of previous AOM. In such a similar scenario, a CT scan or an MRI were mandatory. The statistically higher number of CT scans in the CAM group may be explained by the radiation-sparing policy of our hospital, where a CT scan was performed only in cases of neurological signs or missed clinical improvement after a 48-hour IVAT schedule. In addition, we found a significantly increased CRP in patients with CAM, and higher but not significant WBC and neutrophils count. Thus, an elevated CRP value (in our cohort, above 12 mg/dL) at presentation should prompt the clinician to suspect a complicated form of the disease. This finding is consistent with literature from other countries (e.g. United Kingdom, Spain, Israel) although in these studies the higher value of CRP was not significant [19,20,21,22].
On the whole, 17 out of 85 patients were finally diagnosed with CAM (20.0%) at our center throughout the study period, a value that is in line with existing literature [17, 18]. Although our sample size was limited, the incidence of AM and CAM was similar to other studies over the SARS-CoV-2 pandemic and post-pandemic period [19, 20]. Many recent studies have reported an increase in AM and its complications after COVID-19 restrictions were lifted [15, 16]. In our study, we noticed a decreased incidence during the SARS-CoV-2 pandemic period, likely due to the containment measures and social distancing, while a significant increase in the post-pandemic period was observed, consistently with other respiratory infections in children [15, 23,24,25].
The high rate of CAM in our cohort may be partially attributed to the referral nature of our center, where difficult-to-treat patients from other facilities are concentrated. Indeed 11/85 patients had prior hospitalization in a non-tertiary center where a pediatric-specific multidisciplinary team was not available. The lack of a dedicated team may have contributed to a delayed diagnosis and the increased risk of developing a CAM. Furthermore, patients with CAM had a higher rate of previous home empiric antibiotic therapy, nonetheless, they did not have a shorter hospital stay compared to the AM group as reported by other studies [26]. Probably, they were patients with the worst baseline condition so their general doctors prescribed more antibiotics, however, we cannot establish whether a wrong antibiotic regimen was a risk factor for complications development. Notably, among patients for whom information on home treatment was available, the most frequently used antibiotic was amoxicillin-clavulanic acid, which, although broader in spectrum, does not align with current European guidelines for AOM that recommend amoxicillin monotherapy [27]. Nevertheless, the use of amoxicillin-clavulanic acid may be a more effective empirical choice in certain clinical settings, given the high rate of β-lactamase production by gram-negative microorganisms such as H. influenzae and Moraxella catarrhalis.
P. aeruginosa was the most frequently isolated bacteria in the AM group and S. pyogenes in the CAM group. Historically, S. pneumoniae, S. pyogenes, and H. influenzae have historically been recognized as the most common causes of AM and CAM. The pathogenic role of P. aeruginosa, however, remains uncertain. Several authors suggest that P. aeruginosa should be considered a contaminant originating from the outer ear, and that this pathogen causes a less aggressive form of disease [2, 28,29,30,31]. This hypothesis is supported by the fact that P. aeruginosas was rarely isolated in complicated cases within our cohort.
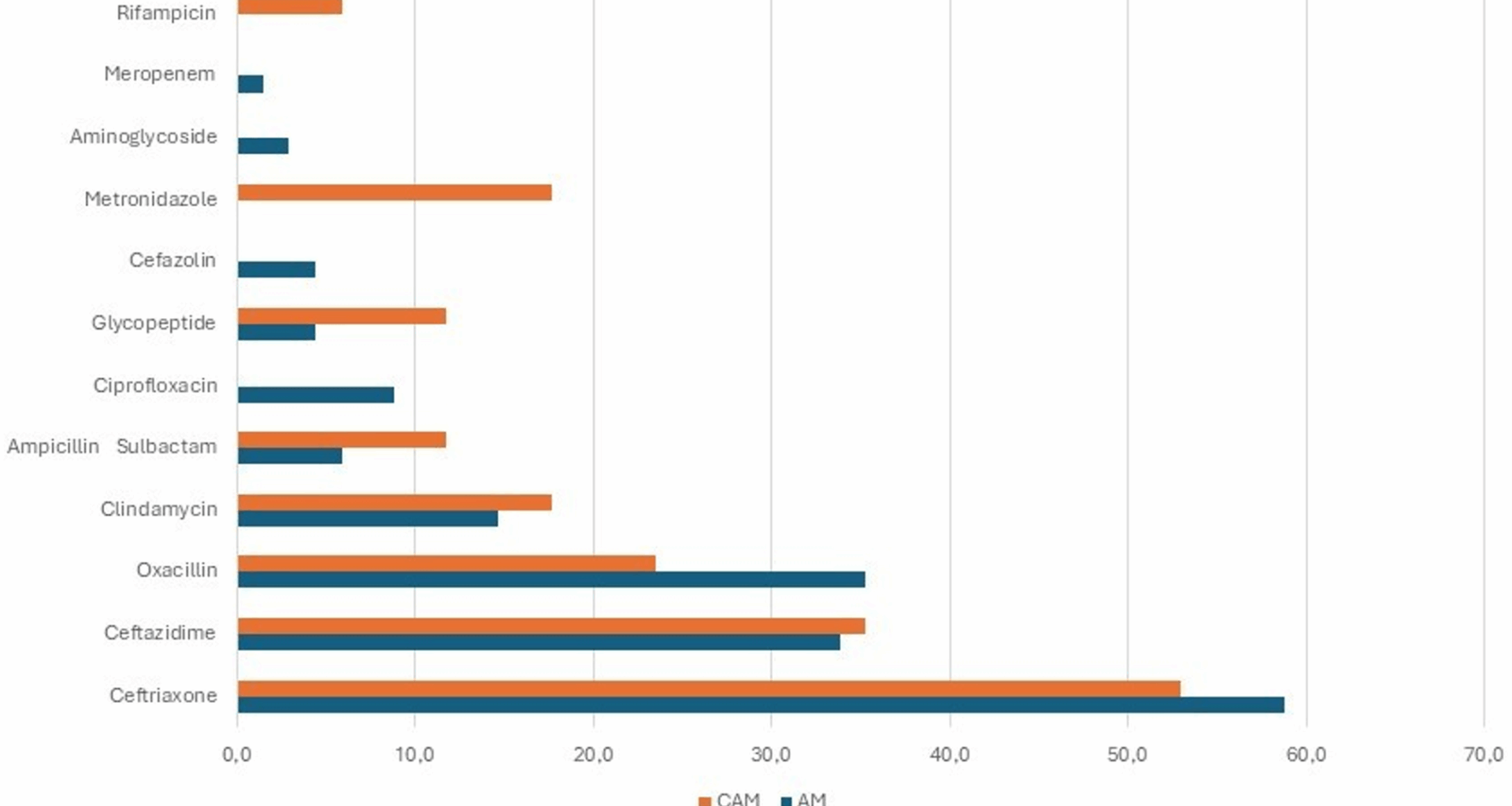
At admission, almost all patients with AM started broad-spectrum IVAT with third-generation cephalosporins or ampicillin/sulbactam to cope with S. pneumoniae, S. pyogenes, and H. influenzae [32]. IVAT was later modified according to the molecular or cultural findings on otorrhea material in over 60% of patients. Eighteen different schedules were employed, and this may reflect the absence of local and international guidelines. Indeed, therapeutic choices were based on the individual judgment of the attending clinicians rather than on a predefined protocol, which explains the observed variability in treatment approaches. According to the current literature, in our cohort third-generation cephalosporins (ceftriaxone or ceftazidime) were the most commonly used antibiotics, alone or in combination with another antibiotic [33,34,35]. Unfortunately, due to the small sample size and the retrospective nature of the study, it is not possible to determine whether a specific therapeutic regimen was initiated in response to the development of a complication or may have contributed to it. As a result, no definitive conclusions can be drawn regarding the relative effectiveness of different treatment strategies. Most patients fully recovered with IVAT alone, so it appeared to be the most appropriate first-line strategy in patients with AM as per the current evidence. However, more studies are needed to discern whether the third-generation cephalosporins should be used alone or in combination, and which one is the most appropriate combination. Moreover, multidisciplinary management (e.g. pediatrician, ENT, and infectivologist) should be also considered as an effective tool for an early diagnosis and a correct therapeutic approach.
In the case of CAM, surgery was the mainstay of treatment, followed by IVAT. Patients underwent mastoidectomy associated with abscess drainage in the event of abscess’ presence. We did not report postoperative complications and only one patient needed an abscess drainage one month after the first surgery for a new episode of AM. A recently published review stated mastoidectomy to be the most effective treatment option in patients affected with CAM, so we may speculate that mastoidectomy should represent the treatment of choice in patients with CAM [8, 36].
Certainly, the low number of patients and the short follow-up period represented the major limitations of our study, as well as its retrospective nature which may have affected the accuracy of diagnosis due to possible deficiencies in clinical records and variability in imaging findings. We recognize that further studies on larger cohorts and longer follow-up periods are warranted to highlight possible signs, symptoms, laboratory, and radiological findings that may facilitate the diagnosis of CAM. Expert agreement and recommendations about the most appropriate diagnostic and treatment work-up are needed to cope with these two rare but severe entities.