Ru D, Wen H, Zhang Y. A pre-generation of emergency reference plan model of public health emergencies with case-based reasoning. Risk Manag Healthc Policy. 2022;15:2371–88.
National Health Commission Website. Interpretation Q&A on. overall plan for implementing category B and B control for novel coronavirus infection. 2022. https://www.gov.cn/zhengce/2022-12/27/content_5733743.htm. Accessed 16 Feb 2024.
Burki T. WHO ends the COVID-19 public health emergency. Lancet Respir Med. 2023;11:588.
United Nations, Geneva. 2023. WHO: the new coronavirus epidemic is no longer a global health emergency, but the new coronavirus is still killing people and mutating. https://news.un.org/zh/story/2023/05/1117647. Accessed 25 Feb 2024.
Wang LX, Yan BB, Boasson V. A national fight against COVID-19: lessons and experiences from China. Aust N Z J Public Health. 2020;44(6):502–7.
Petropoulos F, Apiletti D, Assimakopoulos V, Babai MZ, Barrow DK, Ben Taieb S, et al. Forecasting: theory and practice. Int J Forecast. 2022;38:705–871.
Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–97.
Cabore JW, Karamagi HC, Kipruto H, Asamani JA, Droti B, Seydi ABW, et al. The potential effects of widespread community transmission of SARS-CoV-2 infection in the world health organization African region: a predictive model. BMJ Glob Health. 2020;5:e002647.
Watson GL, Xiong D, Zhang L, Zoller JA, Shamshoian J, Sundin P, et al. Pandemic velocity: forecasting COVID-19 in the US with a machine learning & bayesian time series compartmental model. PLoS Comput Biol. 2021;17:e1008837.
Lazebnik T, Bunimovich-Mendrazitsky S, Ashkenazi S, Levner E, Benis A. Early detection and control of the next epidemic wave using health communications: development of an artificial Intelligence-based tool and its validation on COVID-19 data from the US. Int J Environ Res Public Health. 2022;19(23):16023.
Yakob L. Zika virus after the public health emergency of international concern period, Brazil. Emerg Infect Dis. 2022;28:837–40.
Sayers DR, Hulse ST, Webber BJ, Burns TA, Denicoff AL. Notes from the field: use of emergency medical service data to augment COVID-19 public health surveillance in Montgomery county, maryland, from March to June 2020. JMIR Public Health Surveill. 2020;6:303–6.
Ho TS, Weng TC, Wang JD, Han HC, Cheng HC, Yang CC, et al. Comparing machine learning with case-control models to identify confirmed dengue cases. PLoS Negl Trop Dis. 2020;14:e0008843.
Zhou X, Li Y. Forecasting the COVID-19 vaccine uptake rate: an infodemiological study in the US. Hum Vaccines Immunother. 2022;18:2017216.
Aravamuthan S, Reyes JFM, Yandell BS, Döpfer D. Real-time estimation and forecasting of COVID-19 cases and hospitalizations in Wisconsin HERC regions for public health decision making processes. BMC Public Health. 2023;23:359.
Lurie N. H1N1 influenza, public health preparedness, and health care reform. N Engl J Med. 2009;361:843–5.
Baharoon S, Memish ZA. MERS-CoV as an emerging respiratory illness: a review of prevention methods. Travel Med Infect Dis. 2019;32:101520.
Gray GC, Robie ER, Studstill CJ, Nunn CL. Mitigating future respiratory virus pandemics: new threats and approaches to consider. Viruses. 2021;13:637.
Ahmad FB, Anderson RN, Knight K, Rossen LM, Sutton PD. Advancements in the National Vital Statistics System to meet the real-time data needs of a pandemic. Am J Public Health. 2021;111:2133–40.
Chua AQ, Al Knawy B, Grant B, Legido-Quigley H, Lee WC, Leung GM, et al. How the lessons of previous epidemics helped successful countries fight covid-19. BMJ. 2021;372:n486.
Jia P, Liu S, Yang S. Innovations in public health surveillance for emerging infections. Annu Rev Public Health. 2023;44:55–74.
Tzivian L, Benis A, Rusakova A, Syundyukov E, Seidmann A, Ophir Y. International scientific communication on COVID-19 data: management pitfalls understanding. J Public Health (Oxf). 2024;46(1):87–96.
Revere D, Nelson K, Thiede H, Duchin J, Stergachis A, Baseman J. Public health emergency preparedness and response communications with health care providers: a literature review. BMC Public Health. 2011;11:337.
Biggerstaff M, Slayton RB, Johansson MA, Butler JC. Improving pandemic response: employing mathematical modeling to confront coronavirus disease 2019. Clin Infect Dis. 2021;74:913–7.
Aiken EL, McGough SF, Majumder MS, Wachtel G, Nguyen AT, Viboud C, et al. Real-time estimation of disease activity in emerging outbreaks using internet search information. PLoS Comput Biol. 2020;16:e1008117.
Bhagavathula AS, Raubenheimer JE. A real-time infodemiology study on public interest in Mpox (monkeypox) following the world health organization global public health emergency declaration. Information. 2022;14:5.
Pooransingh S, Abdullah R, Battersby S, Kercheval R. COVID-19 highlights a critical need for efficient health information systems for managing epidemics of emerging infectious diseases. Front Public Health. 2021;9:767835.
Liu C. Health information systems amid COVID-19 outbreak: lessons from China. Health Inf Manag J. 2020;50:99–100.
Brownstein JS, Freifeld CC, Madoff LC. Digital disease detection — harnessing the web for public health surveillance. N Engl J Med. 2009;360:2153–7.
Centers for Disease Control and Prevention. Atlanta. 2022. What is NBS? https://www.cdc.gov/nbs/overview/index.html#print. Accessed 10 Mar 2024.
Bagherian H, Farahbaksh M, Rabiei R, Moghaddasi H, Asadi F. National communicable disease surveillance system: a review on information and organizational structures in developed countries. Acta Inform Med. 2017;25:271–6.
Jia P, Yang S. China needs a national intelligent syndromic surveillance system. Nat Med. 2020;26:990.
Yoo HS, Park O, Park HK, Lee EG, Jeong EK, Lee JK, et al. Timeliness of national notifiable diseases surveillance system in Korea: a cross-sectional study. BMC Public Health. 2009;9:93.
Dixon BE, Grannis SJ, McAndrews C, Broyles AA, Mikels-Carrasco W, Wiensch A, et al. Leveraging data visualization and a statewide health information exchange to support COVID-19 surveillance and response: application of public health informatics. J Am Med Inform Assoc. 2021;28:1363–73.
Valentin S, Arsevska E, Falala S, de Goër J, Lancelot R, Mercier A, et al. PADI-web: a multilingual event-based surveillance system for monitoring animal infectious diseases. Comput Electron Agric. 2020;169:105163.
Ouyang L, Yuan Y, Cao Y, Wang FY. A novel framework of collaborative early warning for COVID-19 based on blockchain and smart contracts. Inf Sci. 2012;570:124–43.
Silk BJ, Scobie HM, Duck WM, Palmer T, Ahmad FB, Binder AM, et al. COVID-19 surveillance after expiration of the public health emergency declaration ― United States, May 11, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:523–8.
Shih DC, Silver R, Henao OL, Alemu A, Audi A, Bigogo G, et al. Incorporating COVID-19 into acute febrile illness surveillance systems, Belize, Kenya, Ethiopia, Peru, and Liberia, 2020–2021. Emerg Infect Dis. 2022;28:34–41.
Ma R, Liu J, An S. Early warning response to rainstorm: designing a model with incentive and supervision mechanisms based on the principal-agent theory. Int J Disaster Risk Reduct. 2024;111:104683.
Jacobs JA, Jones E, Gabella BA, Spring B, Brownson RC. Tools for implementing an evidence-based approach in public health practice. Prev Chronic Dis. 2012;9:E116.
Malilay J, Heumann M, Perrotta D, Wolkin AF, Schnall AH, Podgornik MN, et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104:2092–102.
Qualters JR, Strosnider HM, Bell R. Data to action: using environmental public health tracking to inform decision making. J Public Health Manag Pract. 2015;21:S12–22.
Meng YJ, Zhang YZ, Wang SW, Wu SY, Zhou HN, Ke CW, et al. Lessons learned in the development of a web-based surveillance reporting system and dashboard to monitor acute febrile illnesses in Guangdong and Yunnan provinces, china, 2017–2019. Health Secur. 2020;18:S14–22.
Wang Q, Zhang T, Zhu H, Wang Y, Liu X, Bai G, et al. Characteristics of and public health emergency responses to COVID-19 and H1N1 outbreaks: a case-comparison study. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph17124409.
Liang HG, Xue YJ. Investigating public health emergency response information system initiatives in China. Int J Med Inform. 2004;73:675–85.
Kebede S, Gatabazi JB, Rugimbanya P, Mukankwiro T, Perry HN, Alemu W, et al. Strengthening systems for communicable disease surveillance: creating a laboratory network in Rwanda. Health Res Policy Syst. 2011;9:27.
Kinkade C, Russpatrick S, Potter R, Saebo J, Sloan M, Odongo G, et al. Extending and strengthening routine DHIS2 surveillance systems for COVID-19 responses in Sierra leone, Sri lanka, and Uganda. Emerg Infect Dis. 2022;28:S42–8.
Wilburn J, O’Connor C, Walsh AL, Morgan D. Identifying potential emerging threats through epidemic intelligence activities—looking for the needle in the haystack? Int J Infect Dis. 2019;89:146–53.
Zou Y. Leveraging digital infrastructure for pandemic governance: preparation, praxis, and paradox. Public Perform Manag Rev. 2022;46:140–64.
Sasangohar F, Moats J, Mehta R, Peres SC. Disaster ergonomics: human factors in COVID-19 pandemic emergency management. Hum Factors. 2020;62(7):1061–8.
Cao Y, Shan J, Gong Z, Kuang J, Gao Y. Status and challenges of public health emergency management in China related to COVID-19. Front Public Health. 2020;8:250.
Zhang TT, Wang Q, Wang Y, Bai G, Dai RM, Luo L. Early surveillance and public health emergency responses between novel coronavirus disease 2019 and avian influenza in China: a case-comparison study. Front Public Health. 2021;9:629295.
Blauer B, Brownstein JS, Gardner L, Kraemer MUG, Rioja ZBL, Mathieu E, et al. Innovative platforms for data aggregation, linkage and analysis in the context of pandemic and epidemic intelligence. Eurosurveillance. 2023;28(24):2200860.
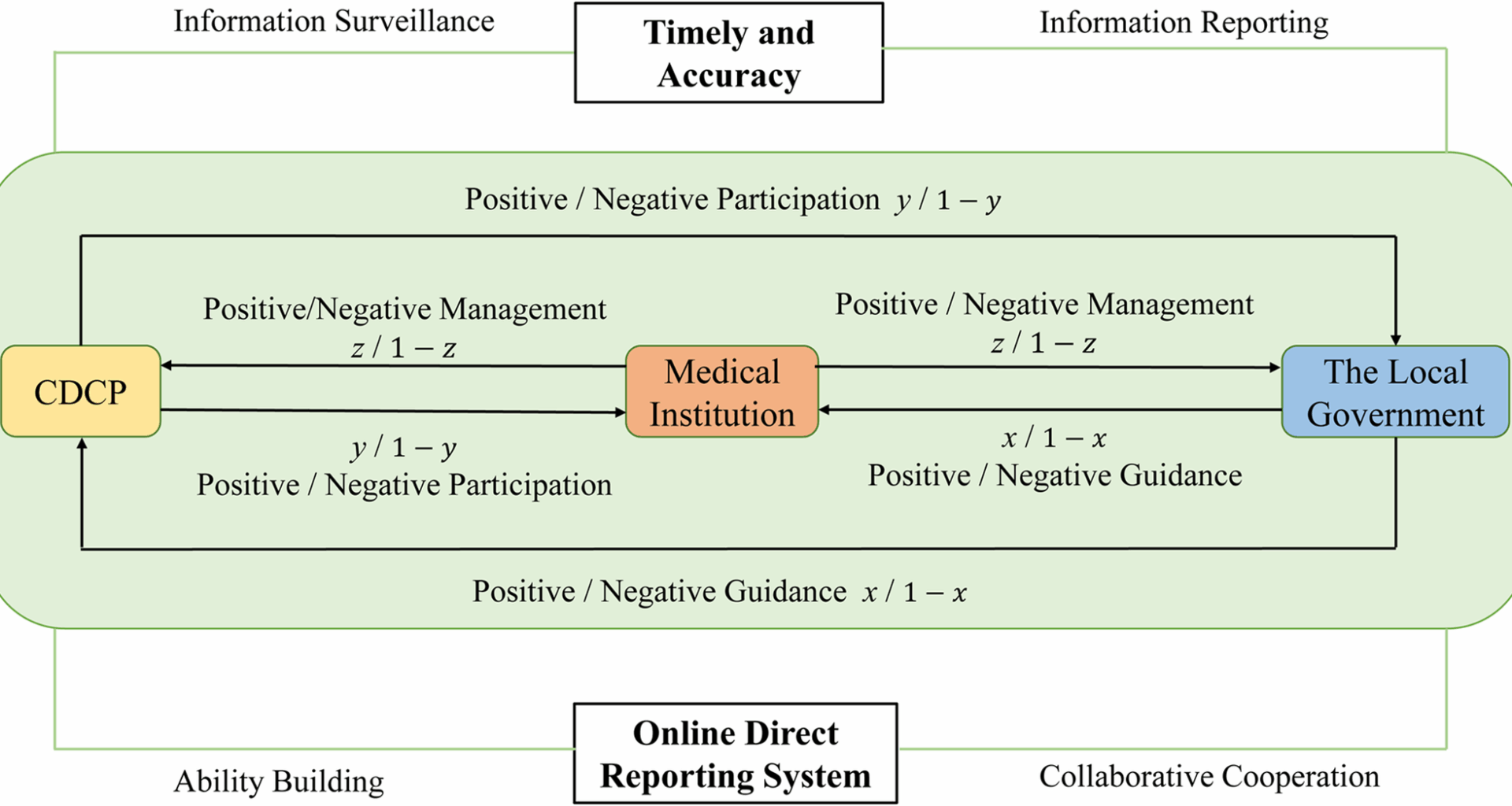
Liu J, Fu Z, Song Y, Ma R, Zhao Z. How to improve the effectiveness of Cooperation networks of emergency science communication for public health emergencies. Hum Soc Sci Commun. 2024;11:1149.
Wu Z, Tian H, Xu D, Chen J, Hu Y, Wang X, et al. Influencing factors and symbiotic mechanism of the integration of medical care and disease prevention during the COVID-19 pandemic: a cross-sectional survey of public hospital employees. Int J Environ Res Public Health. 2022;20(1):20:241.
Cheng LF, Liu GY, Huang HQ, Wang XG, Chen Y, Zhang J, et al. Equilibrium analysis of general N-population multi-strategy games for generation-side long-term bidding: an evolutionary game perspective. J Clean Prod. 2020;276:124123.
Fang L, An CX, Yi B. Research on detection and early warning mechanism of emergency public health medical education system based on internet of things technology. Comput Intell Neurosci. 2022;2022:3008206.
Chen S, Xu Q, Buchenberger J, Bagavathi A, Fair G, Shaikh S, et al. Dynamics of health agency response and public engagement in public health emergency: A case study of CDC tweeting patterns during the 2016 Zika epidemic. JMIR Public Health Surveill. 2018;4(4):73–85.
Sasie SD, Van Zuylen P, Ayano G, Aragaw FM, Spigt M. Information sharing across institutions: practices and barriers during public health emergencies in Ethiopia. Int J Med Inform. 2024;186:105439.
Ageron FX, Hugli O, Dami F, Caillet-Bois D, Pittet V, Eckert P, et al. Lessons from COVID-19 syndromic surveillance through emergency department activity: a prospective time series study from Western Switzerland. BMJ Open. 2022;12(5):e054504.
Gotham IJ, Sottolano DL, Hennessy ME, Napoli JP, Dobkins G, Le LH, et al. An integrated information system for all-hazards health preparedness and response: new York state health emergency response data system. J Public Health Manag Pract. 2007;13(5):486–96.
Soujaa I, Nukpezah JA, Benavides AD. Coordination effectiveness during public health emergencies: an institutional collective action framework. Adm Soc. 2021;53(7):1014–45.
Khan Y, Sanford S, Sider D, Moore K, Garber G, de Villa E, et al. Effective communication of public health guidance to emergency department clinicians in the setting of emerging incidents: a qualitative study and framework. BMC Health Serv Res. 2017;17:312.
Ma R, Liu J, An S. The early warning mechanism of public health emergencies through whistleblowing: a perspective based on considering the uncertainty of risk perception. Risk Manag Healthc Policy. 2023;16:503–23.
Whitelaw S, Mamas MA, Topol E, Van Spall HGC. Applications of digital technology in covid-19 pandemic planning and response. Lancet Digit Health. 2020;2(8):435–40.
Liu J, Dong C. Cross-departmental emergency coordination characteristics formed by multiple risks: evidence from production safety special emergency campaigns across government levels in China. Int J Disaster Risk Reduct. 2024;111:104672.
Westbrook G, Hollen H, Naqvi O, Neuwald S, Hann N, Cox G, et al. Achieving a healthy Oklahoma: cross-sector cooperation to improve public health preparedness and pandemic response. Health Secur. 2023;21:358–70.
Jacenko S, Blough S, Grant G, Tohme R, McFarland J, Hatcher C, et al. Lessons learnt from the applying the centers for disease control and prevention (CDC) evaluation framework to the measles incident management system response, USA, 2020–2021. BMJ Glob Health. 2023;8:e011861.
Zhao Y, Liu L, Qi Y, Lou F, Zhang J, Ma W. Evaluation and design of public health information management system for primary health care units based on medical and health information. J Infect Public Health. 2020;13:491–6.
Shah GH, Newell B, Whitworth RE. Health departments’ engagement in emergency preparedness activities: the influence of health informatics capacity. Int J Health Policy Manag. 2017;5:575–82.
Siya A, Mafigiri R, Migisha R, Kading RC. Uganda Mountain community health system—perspectives and capacities towards emerging infectious disease surveillance. Int J Environ Res Public Health. 2021;18:18:8562.
Lai S, Kitamura K. Update on emerging infections: news from the centers for disease control and prevention. Ann Emerg Med. 2021;78(1):49–52.
Herman-Roloff A, Aman R, Samandari T, Kasera K, Emukule G, Amoth P, et al. Adapting longstanding public health collaborations between government of Kenya and CDC Kenya in response to the COVID-19 pandemic, 2020–2021. Emerg Infect Dis. 2022;28:S159–67.
Tavakkoli M, Karim A, Fischer FB, Llamas LM, Raoofi A, Zafar S, et al. From public health policy to impact for COVID-19: a multi-country case study in Switzerland, Spain, Iran and Pakistan. Int J Public Health. 2022;67:1604969.
Woldetsadik MA, Fitzpatrick K, Del Castillo L, Miller B, Jarvis D, Carnevale C, et al. Stakeholders’ assessment of US centers for disease control and prevention’s contributions to the development of national public health institutes in seven countries. J Public Health Policy. 2021;42:589–601.
Meckawy R, Stuckler D, Mehta A, Al-Ahdal T, Doebbeling BN. Effectiveness of early warning systems in the detection of infectious diseases outbreaks: a systematic review. BMC Public Health. 2022;22(1):2216.
Leray LSG, Ward MP. Web-scraping applied to acquire difficult to access animal disease outbreak information, using African swine fever in Europe as an example. Transbound Emerg Dis. 2021;68(5):2795–805.
Chiang SC, Fisher HH, Bridwell ME, Rasulnia BB, Kuwabara SA. Motivators of continued participation in public health emergency response among federal public health workers: a qualitative study. Health Secur. 2021;19:386–92.
Perrotta DM, Lemmings J, Maillard JM. Enhancing epidemiology capacity during the 2014-15 West Africa Ebola outbreak: an assessment of the role of applied public health epidemiologists. J Public Health Manag Pract. 2020;26:595–601.
Zuber A, Pearson J, Sebeh Y, Jarvis D, Bratton S. Essential public health functions are not enough: fostering linkages between functions through national public health institutes improves public health impact. BMJ Glob Health. 2023;8:e011728.
Shoaib HM. Monkeypox as a potential emerging pandemic: a discussion on future risks and preparedness in Saudi Arabia. Front Public Health. 2023;11:1254545.
Haghighi H, Takian A, Raoofi A. Institutionalization of health system to combat the COVID-19 pandemic in Iran. Int J Public Health. 2023;68:1606197.
Keita M, Talisuna A, Chamla D, Burmen B, Cherif MS, Polonsky JA, et al. Investing in preparedness for rapid detection and control of epidemics: analysis of health system reforms and their effect on 2021 Ebola virus disease epidemic response in Guinea. BMJ Glob Health. 2023;8:e010984.
Lee CH, Wang D, Lyu S, Evans RD, Li L. A digital transformation-enabled framework and strategies for public health risk response and governance: China’s experience. Ind Manag Data Syst. 2022;123:133–54.
Romano S, Yusuf H, Davis C, Thomas MJ, Grigorescu V. An evaluation of syndromic surveillance-related practices among selected state and local health agencies. J Public Health Manag Pract. 2022;28(2):109–15.
Mao ZJ, Yao H, Zou Q, Zhang WT, Dong Y. Digital contact tracing based on a graph database algorithm for emergency management during the COVID-19 epidemic: case study. JMIR Mhealth Uhealth. 2021;9(1):e26836.
Keating P, Murray J, Schenkel K, Merson L, Seale A. Electronic data collection, management and analysis tools used for outbreak response in low- and middle-income countries: a systematic review and stakeholder survey. BMC Public Health. 2021;21(1):1741.
Ario AR, Makumbi I, Kadobera D, Bulage L, Ocom F, Kwesiga B, et al. Uganda National Institute of public health: establishment and experiences, 2013–2021. Glob Health Sci Pract. 2022;10(4):e2100784.
Liu J, Ma R, Song Y, Dong C. Developing the urban fire safety co-management system in China based on public participation. Fire. 2023;6:400.