World Health Organisation. Cervical cancer. 2022. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer Accessed on: 2 Oct 2023.
Kutz JM, Rausche P, Gheit T, Puradiredja DI, Fuscp D. Barriers and facilitators of HPV vaccination in sub-Saharan Africa: a systematic review. BMC Public Health. 2923;23:974.
Isabirye A, Elwange BC, Singh K, Allegri MD. Individual and community-level determinants of cervical cancer screening in Zimbabwe: a multi-level analyses of a nationwide survey. BMC Womens Health. 2022;22:309.
Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gomez D, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and Related Diseases in Zimbabwe. Summary Report 10 March 2023; https://hpvcentre.net/statistics/reports/ZWE.pdf.
Kuguyo O, Matimba A, Tsikai N, Magwali T, Madziyire M, Gidiri M, et al. Cervical cancer in Zimbabwe: a situation analysis. Pan Afr Med J. 2017;27:215.
Zibako P, Tsikai N, Manyame S, Ginindza TG. Cervical cancer management in Zimbabwe (2019–2020). PLoS ONE. 2022;17(9): e0274884.
Bowden SJ, Doullgeraki T, Bouras E, Markozannes G, Athanasiou A, Grout-Smith H, et al. Risk factors for human papillomavirus infection, cervical intraepithelial neoplasia and cervical cancer: an umbrella review and follow-up Mendelian randomisation studies. BMC Med. 2023;21:274.
Plesa A, Socolov D, Huica I, Botezatu A, Iancu IV, Ungureanu C, et al. High-risk human papillomaviruses distribution in Romanian women with negative cytology. J Infect Dev Ctries. 2019;13(4):326–33.
Seyoum A, Assefa N, Gure T, Seyoum B, Mulu A, Mihret A. Prevalence and genotype distribution of high-risk human papillomavirus infection among sub-Saharan African women: a systematic review and meta-analysis. Front Public Health. 2022;10: 890880.
Rahangdale L, Mungo C, O’Connor S, Chibwesha CJ, Brewer NT. Human papillomavirus vaccination and cervical cancer risk. BMJ. 2022;379: e070115.
Zhao R, Sekar P, Bennis SL, Kulasingam S. A systematic review of the association between smoking exposure and HPV-related cervical cell abnormality among women living with HIV: implications for prevention strategies. Prev Med 2023; 170.107494.
Hemmat N, Baghi HB (2019) Association of human papillomavirus infection and inflammation in cervical cancer. Pathogens Dis 2019;77(5):ftz048.
Xi LF, Koutsky LA, Castle PE, Edelstein ZR, Meyers C, Ho J, et al. Relationship between cigarette smoking and human papillomavirus type 16 and 18 DNA load. Cancer Epidemiol Biomark Prev. 2010;18(12):3490–6.
Yang Z, Sub P, Dahlstrom KR, Gross N, Li G. Joint effect of human papillomavirus exposure, smoking and alcohol on risk of oral squamous cell carcinoma. BMC Cancer. 2023;23:457.
Laczano-Ponce E, Herrero R, Munoz N, et al. Epidemiology of HPV infection among Mexican women with normal cytology. Int J Cancer. 2001;91(3):412–20.
Utami TW, Kusuma F, Winarto H, Anggraeni TD, Peters AAW, Spaans V, et al. Tobacco use and its association with HPV infection in normal uterine cervix: a study from a sustainable development goals perspective. Tob Induc Dis. 2021;19(64).
Cooper D, Hoffman M, Carrara H, Rosenberg L, Kelly J, Stander I, et al. Determinants of sexual activity and its relation to cervical cancer risk among South African women. BMC Public Health. 2007;7:341.
Ajuwon AJ, Olaleye A, Faromoju B, Ladipo O. Sexual behavior and experience of sexual coercion among secondary school students in three states in North-Eastern Nigeria. BMC Public Health. 2006;6:310.
Manga MM, Fowotade A, Abdullahi YM, Ek-nafaty AU, Adamu DB, Pindiga HU, et al. Epidemiological patterns of cervical human papillomavirus infection among women presenting for cervical cancer screening in North-Eastern Nigeria. Infect Agent Cancer. 2015;10:39.
Thomas TL, Yarandi HN, Dalmida SG, Frados A, Klienert K. Cross-cultural differences and sexual risk behaviour of emerging adults. J Transcult Nurs. 2015;26(1):64–72.
Clarke MA, Risley C, Stewart MW, Geisinger KR, Hiser LM, Morgan JC, Owens KJ, Ayyalasomayajula K, Rive RM, Jannela A, et al. Age-specific prevalence of human papillomavirus and abnormal cytology at baseline in a diverse statewide prospective cohort of individuals undergoing cervical cance screening in Mississippi. Cancer Med. 2021;10(23):8641–50.
Mekonnen AG, Mittiku YM. Early onset of sexual activity as a potential risk of cervical cancer in Africa: a review of literature. PLOS Glob Public Health. 2023;3(3): e0000941.
Yin LX, D’Souza G, Westra WH, Wang SJ, va Zante A, Zhang Y, et al. Prognostic factors for human papillomavirus-positive and negative oropharyngeal carcinomas. The Laryngoscope. 2018;128(8):288–296.
Huang Y, He Q, Xu K, Zhou J, Yin J, Li F, et al. A new marker based on risk stratification of human papillomavirus DNA and tumour size to predict survival of locally advanced cervical cancer. Int J Gynecol Can. 2019;29:459–65.
Lin G, Yang LY, Lin YC, et al. Prognostic model based on magnetic resonance imaging, whole-tumour apparent diffusion coefficient values and HPV genotyping for stage IB-IV cervical cancer patients following chemoradiotherapy. Eur Radiol. 2019;29:556–65.
Rose BR, Thompson CH, Simpson JM, Jarrett CS, Elliott PM, Tattersall MH, et al. Human papillomavirus deoxyribonucleic acid as a prognostic indicator in early-stage cervical cancer: a possible role for type 18. Am J Obstet Gynecol. 1995;173:1461–8.
Nakagawa S, Yoshikawa H, Onda T, Kawana T, Iwamoto A, Taketani Y. Type of human papillomavirus is related to clinical features of cervical carcinoma. Cancer (Phila).1998;78:1935–41.
Schwartz M, Daling JR, Shera KA, Madeleine MM, McKnight B, Galloway DA, et al. Human papillomavirus and prognosis of invasive cervical cancer: a population-based study. J Clin Oncol. 2001;19(7):1906–15.
Im SS, Wilczynski SP, Burger RA, Monk BJ. Early stage cervical cancers containing human papillomavirus type 18 DNA have more nodal metastasis and deeper stromal invasion. Clin Cancer Res. 2003;9:4145–50.
Huang LW, Chao SL, Hwang JL. Human papillomavirus-31-related types predict better survival in cervical carcinoma. Cancer. 2004;100(2):327–34.
Van Bommel PF, van den Brule AJ, Helmerhorst TJ, Gallee MP, Gaarenstroom KN, Walboomers JM, et al. HPV DNA presence and HPV genotypes as prognostic factors in low-stage squamous cell cervical cancer. Gynecol Oncol. 1993;48:333–7.
Wright JD, Li J, Gerhard DS, Zhang Z, Huettner PC, Powell MA, et al. Human papillomavirus type and tobacco use as predictors of survival in early-stage cervical carcinoma. Gynecol Oncol. 2005;98(1):84–91.
Kuguyo O, Chambwe N, Nhachi CFB, Tsikai N, Dandara C, Matimba A. A cervical cancer biorepository for pharmacogenomics research in Zimbabwe. BMC Cancer. 2022;22:1320.
Kuguyo O, Matimba A, Madziyire MG, et al. Prevalence and predictors for cisplatin-induced toxicities in Zimbabwean women with cervical cancer. Future Oncol. 2024;20:1909–24.
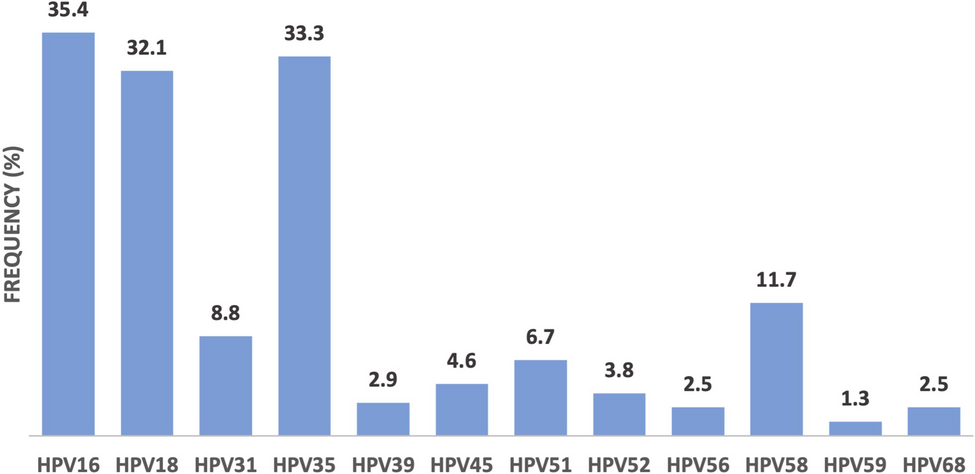
Kuguyo O, Dube Mandishora RS, Thomford NE, Makunike Mutasa R, Nhachi CFB, Matimba A, et al. High-risk HPV genotypes in Zimbabwean women with cervical cancer: comparative analyses between HIV-negative and HIV positive women. PLoS ONE. 2021;16(9): e035732.
Gagnon S, Hankins C, Tremblay C, Forest P, Pourreaux K, Coutlee F and Canadian Women’s HIV study group. Viral polymorphism in human papillomavirus types 33, 35 and persistent and transient infection in the genital tract of women. J Infect Dis. 2004;190(9):1575–1585.
Mboumba Bouassa RS, Ntsigouaye JA, Tsimba PCL, Nodjikouambaye ZA, et al. Genetic diversity of HPV35 in Chad and the Central African Republic, two landlocked countries of Central Africa: A cross sectional study. PLoS ONE. 2024;19(1):e0297054.
Hammes LS, Tekmal RR, Naud P, et al. Macrophages inflammation and risk of cervical intraepithelial neoplasia (CIN) progression—clinicopathological correlation. Gynecol Onol. 2007;105:157–65.
Fernandes JV, De Medeiros Fernandes TA, De Azevedo JC, Cobucci RN, De Carvalho MG, Andrade VS, De Arauj JM. Link between chronic inflammation and human papillomavirus-induced carcinogenesis (Review). Oncol Lett. 2015;9(3):1015–26.
Mastrogeorgiou M, Chatzkalil E, Theocharis S, Papoudou A, Peoc’h M, Mobarki M, Karpathiou G. The immune microenvironment of cancer of the uterine cervix. Histol Histopathol. 2024;39(10):1245–1271.
Wee CW, Huang A, Huskey KW, McCarthy EP. Obesity and the likelihood of sexual behaviour risk factors for HPV and cervical cancer. Obesity (Silver Spring). 2008;16(11):2552–5.
Urbute A, Thomsen LT, Belmonte F, Kesmodel US, Frederiksen K, Kjoer SK. The role of body mass index in incidence and persistence of cervical human papillomavirus infection. Ann Epidemiol. 2020;49:36–41.
Aguayo F, Munoz JP, Perez-Dominguez F, Carrillo-Beltran D, Oliva C, Calaf GM, et al. High-risk human papillomavirus and tobacco smoke interactions in epithelial carcinogenesis. Cancers (Basel). 2020;12(8):2201.
Prokopczyk B, Cox JE, Hoffmann D, Waggoner SE. Identification of tobacco-specific carcinogen in the cervical smokers and nonsmokers. J Natl Cancer Inst. 1997;89(12):868–73.
Kum-Nji P, Meloy L, Keyser-Marcus L. Tobacco smoke exposure as a risk factor for human papillomavirus infections in women 18–26 years old in the United States. PLoS ONE. 2019;14(10): e0223532.
Utami TW, Kusuma F, Winarto H, et al. Tobacco use and its association with HPV infection in normal uterine cervix: a study from a sustainable development goals perspective. Tob Induc Dis. 2021;19(64).
Berrington de Gonzalez A, Sweetland S, Green J. Comparison of risk factors for squamous cell and adenocarcinomas of the cervix: a meta-analysis. Br J Cancer. 2004;90(9):1787–1791.
Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gomez D, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and related diseases report: World. 2022. https://hpvcentre.net/statistics/reports/XWX.pdf Accessed on: 21 May 2022.
Munoz N, Franceshi S, Bosetti C, et al. Role of parity and human papillomavirus in cervical cancer: the IARC multicentric case-control study. Lancet. 2002;359:1093–101.
Castellsague X, Munoz N. Chapter 3: Cofactors in human papillomavirus carcinogenesis—role of parity, oral contraceptives, and tobacco smoking. J Natl Cancer.2003;31:20–8.
Matos A, Moutinho J, Pinto D, et al. The influence of smoking and other cofactors on the time to onset to cervical cancer in a southern European population. Eur J Cancer Prev. 2005;14(5):485–91.
Luhn P, Walker J, Schiffman M, et al. The role of co-factors in the progression from human papillomavirus infection to cervical cancer. Gynecol Oncol. 2013;128(2):265–70.
Tekalegn Y, Sahiledengle B, Woldeyohannes D, et al. High parity is associated with increased risk of cervical cancer: systematic review and meta-analysis of case-control studies. Women’s Health. 2022;18.
Tong SY, Lee YS, Park JS, Namkoong SE. Human papillomavirus genotype as a prognostic factor in carcinoma of the uterine cervix. IJGC. 2007;17(6):1307–13.
Genta ND, Martins TR, Lopez RVM, et al. Multiple HPV genotype infection impact on invasive cervical cancer presentation and survival. PLoS ONE. 2017;12(8): e0182854.
Lombard I, Vincent-Salomon A, Validire P, Zafrani B, de la Rochefordiere A, Clough K, et al. Human papillomavirus genotype as a major determinant of the course of cervical cancer. J Clin Oncol. 1998;16(8):2613–9.
Fernandes A, Viveros-Carreno D, Hoegi J, Avila M. Pareja R (2022) Human papilomavírus-independent cervical câncer. Int J Gynecol Cancer. 2022;32:1–7.
Rodriguez-Carunchio L, Soveral I, et al. HPV-negative carcinoma of the uterine cevric: a distinctive of cervical cancer with poor prognosis. BJOG. 2015;122:199–227.
Li P, Tan Y, Zhu LX, et al. Prognostic value of HPV DNA status in cervical cancer before treatment: a systematic review and meta-analysis. Oncotarget. 2017;8(39):66352–9.
LaMontagne DS, Manangazira P, Marembo J, et al. HPV vaccination coverage in three districts in Zimbabwe following national introduction of 0,12 month schedule among 10 to 14 year old girls. Vaccine. 2022;40(1):A58-66.