Bladder cancer arising within a bladder diverticulum presents significant diagnostic and therapeutic challenges due to its distinctive anatomical features. Bladder diverticula can arise congenitally or because of chronic bladder outlet obstruction. Notably, the frequent absence of muscularis propria in the diverticular wall complicates accurate tumor staging and increases the likelihood of extravesical tumor extension, thus directly impacting both diagnostic precision and therapeutic planning. This poses challenges for complete transurethral resection in patients with urothelial carcinoma. Tumor markers, cytology, or risk stratification systems do not aid in prognosis of these atypical tumors. Male sex and increasing age are significant risk factors for malignancy development in diverticula [6].
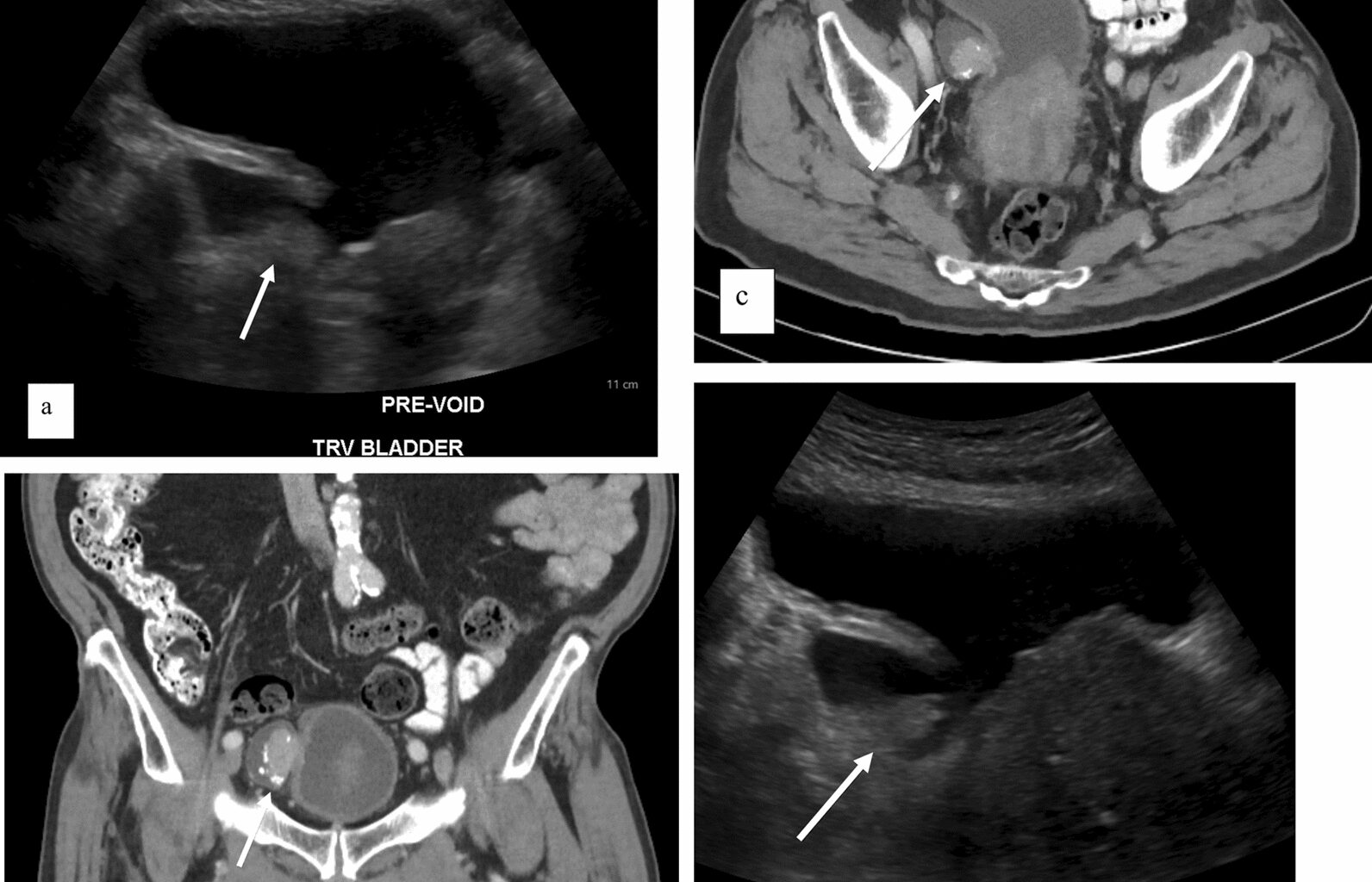
Patients typically present with painless hematuria, the most common symptom, accompanied by irritative voiding symptoms. In advanced cases, complications, such as urinary retention, recurrent infections, or palpable masses, may occur. Imaging, such as ultrasound and CT urography, are crucial for identifying tumors within diverticula. While ultrasound may detect masses, its sensitivity is lower. Cystoscopy remains the gold standard for direct visualization and biopsy, but obtaining adequate tissue samples can be challenging due to the anatomical constraints of the diverticulum.
Transurethral resection of bladder tumors is the cornerstone for initial management for noninvasive uroepithelial carcinoma of the bladder but they often require alternative treatments depending on tumor stage, grade, reoccurrence risk, and patient factors. Intravascular therapy, radical cystectomy or partial cystectomy, neuro adjuvant chemotherapy, immunotherapy, and radiation serve as additional options [1,2,3]. For nonmuscle-invasive disease confined to the diverticulum, conservative management options—including transurethral resection of the tumor can be considered, provided that complete resection is feasible and perforation risk is carefully assessed [7, 8]. For muscle-invasive or high-risk transitional cell carcinoma (TCC) within a diverticulum, radical cystectomy, partial cystectomy with diverticulectomy remains the recommended standard of care, primarily because complete tumor excision is often unachievable with transurethral techniques, which also carry substantial risk of perforation [1,2,3, 7, 8]. Regardless of initial management strategy, rigorous cystoscopic surveillance is critical following complete resection, given the substantial risk of disease recurrence or progression in this anatomically compromised setting.
This patient underwent transurethral resection due to his comorbidities. Transurethral resection may be attempted in such circumstances or with low grade disease but is often incomplete due to the lack of muscularis propria in the diverticular wall [7, 8]. Intravesical therapy with Bacillus Calmette-Guérin (BCG) or mitomycin C can be considered for recurrent superficial tumors. These agents reduce the risk of recurrence and, in the case of BCG, also lower the likelihood of progression in high-risk nonmuscle-invasive bladder cancer [8]. For advanced disease, combination chemotherapy regimens may be employed [8]. Radiation therapy plays a limited role but may be adjunctive in palliative settings [9].
Bladder carcinoma in diverticula has a poorer prognosis compared with intravesical carcinoma owing to delayed detection and early invasion [5, 10]. Regular follow-up with cystoscopy and imaging is critical for monitoring recurrence.