SINCE the 1980s, researchers have worked tirelessly to develop effective treatments that can suppress the HIV virus to undetectable levels. As a result, by taking a single daily dose of an antiretroviral (ARV) medicine, people with HIV can now expect to live long and healthy lives – as well as prevent transmission to others.
The impact has been dramatic, with annual global AIDS-related deaths having fallen from 2.1 million at the peak in 2004 to 630,000 in 2024. The number of new acquisitions has plummeted too: an estimated 1.3 million people acquired the virus in 2024, marking a 60 per cent decline since the peak in 1995.
“We’re at a pivotal moment in the quest to end the HIV epidemic,” says Jean van Wyk, chief medical officer at ViiV Healthcare. This quest is to meet the UN’s 2030 goals that ViiV has been involved with since the 1980s as the pioneers of the first ARV medicine.
Barriers to care
Despite the tremendous progress in scientific innovation, there is still a long way to go. “As more progress has been made, many people have become complacent about HIV,” says van Wyk. Of the 41 million people living with HIV today, nearly a quarter are not receiving life-saving treatment and new transmissions are not falling fast enough. “We’re still seeing new diagnoses in a broader range of communities, and we’re certainly at risk of missing our goal,” he says.
So what will it take to end the epidemic?
The most basic principle is to get tested for HIV. Early diagnosis can lead to early treatment and have a tremendous impact on the course of disease. Although testing has improved since the setbacks during the global pandemic, about 5.3 million people still did not know that they were living with HIV in 2024, according to UNAIDS.
Advanced therapy
Another goal is to develop innovative treatment options that address the realities of day to day living. For many, especially those at the margins who are dealing with challenges like mental health issues, substance abuse or homelessness, having to take a pill every day can be a barrier to staying on treatment. For them, ARV therapy has advanced from several pills throughout the day with considerable side effects, to one pill a day, or longer-acting options.
Improvements to quality-of-life are also important. Even for those who stick to their treatments, says Babafemi Taiwo, vice president and head of early development at ViiV, “the pills are a constant reminder of the trauma of diagnosis and the burdens of living with HIV, which makes it difficult for people to be truly free from the virus.” Linking individuals to quality health care is key to allowing people living with HIV to live long, healthy lives and reduce the likelihood of transmission to sexual partners.
Preventing HIV in the first place is a vital step to ending the HIV epidemic. PrEP (preexposure prophylaxis) is medicine that greatly reduces the likelihood of becoming HIV-positive if exposed. With multiple options available, including daily oral pills or long-acting treatment, more people can feel empowered to take control of their health and reduce the chance of acquiring HIV.
Addressing and eliminating stigma will be crucial too. According to the CDC, HIV has been marked by intense stigma, rooted in fear and misconceptions that persist from the epidemic’s early days. “Fear of disclosure is a major problem,” says Taiwo. “There is fear that somebody might find your pills in your backpack or in your locker.”
“It’s hard to imagine, but I still see women who I have been looking after for 25 years, and they only feel able to talk about their status with us in the clinic,” says Annemiek de Ruiter, head of global medical sciences at ViiV and a consultant physician specialising in HIV care. Many of her patients experience intense fear and stigma, often years after diagnosis. “I’ve become very aware of people who are still hiding their medication and every day trying to find a moment when nobody’s watching to take it.”
Given this stigma, many people avoid being tested or taking their HIV medicine for fear of being labelled. It also helps to explain why, for all the scientific progress, eliminating stigma remains one of the major challenges in ending the epidemic. As the only global company solely focused on preventing, treating and ultimately curing HIV, ViiV is unafraid to disrupt the status quo for HIV treatment and prevention by designing innovations that meet the evolving needs of the HIV community.
That’s why ViiV is continuing to develop therapies that can make it easier to stick with treatment, with options for longer dosing intervals and more freedom. De Ruiter says longer-acting medicines could overcome many of the practical and social challenges faced by those living with the virus.
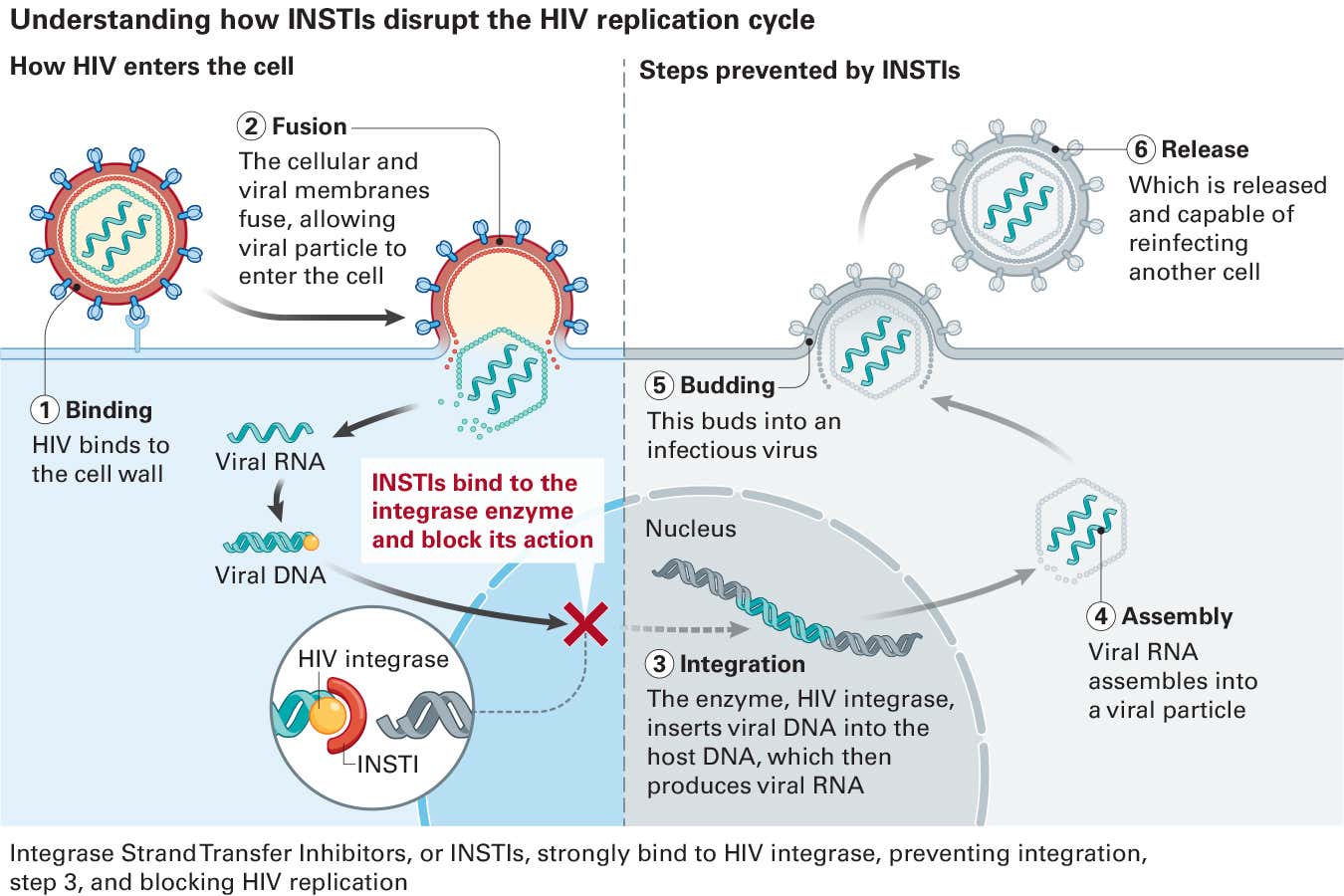
Relentless in the pursuit to end HIV, ViiV’s world-class scientists are continuing to define the future of long-acting innovation with the next generation of HIV treatment, including a portfolio built around a class of drugs known as integrase strand transfer inhibitors, or INSTIs.
Longer-acting options
“INSTIs play a central role in modern HIV care and are considered the gold standard,” says Sherene Min, vice president and head of global clinical development at ViiV. “Longer-acting therapies, in particular, will address many of the challenges around stigma, adherence and quality of life.”
Certain medicines developed by ViiV have been used in combination with other ARVs to achieve optimal viral suppression or for HIV prevention. Now, ViiV is developing longeracting therapies as the next generation of long-acting HIV tools and the cornerstone for HIV care of tomorrow. These treatments must have a high barrier to resistance, staying ahead of the virus, and might be delivered in different formulations to offer a range of treatment and prevention options.
“We’ve learned that if you give people choice, they’re more likely to have success with treatment,” says Min. “You need to think about what is going to fit best with people’s lives.” That is especially important when it comes to tackling HIV in children, who often struggle with access and adherence to treatments, says Min. ViiV is currently developing innovative formulations designed for them.
All of that has important consequences for the UN’s goal of ending the epidemic by 2030. ViiV believes the next generation of INSTIs will be a big part of the solution, so that no person living with HIV is left behind.
“The tremendous strides we’ve made provide so much hope,” says van Wyk. “We’re getting to the point where we can talk about ending the HIV epidemic, which is an incredible feat of science. But we have to keep pushing because there is more to do.”
To find out more visit: viivhealthcare.com/ending-hiv/