AACE has seen a rise in research in recent years, likely due to its increased incidence [1,2,3,4,5,6,7,8,9,10, 18,19,20,21,22,23]. There are notable differences in the demographic characteristics of AACE cases based on age [18, 22, 23] and country of origin [10, 19,20,21,22,23]. The current study investigated the demographic characteristics of 118 AACE cases surgically treated in our strabismus referral center. Among these cases, 39% were preschool children (under 6 years old), 48.3% were primary school children (ages 6–11), and 12.7% were adolescents (12 years and older). Refractive errors were more myopic in the adolescent group compared to the other two groups. This group also exhibited a higher prevalence of diplopia as their presenting symptom, while their preoperative esotropia was significantly lower. It is important to note that children with AACE at the preschool age typically present with hyperopic refractive errors. However, they usually have a non-significant refractive error for their age and lack a refractive component, which helps differentiate their diagnosis from that of refractive accommodative ET and partially accommodative ET cases. Our findings are consistent with previous studies [10, 18,19,20,21,22,23], including the most recent study, which indicated a negative correlation between age and spherical equivalent of the involved eyes and the angle of deviation at distance [18].
The current study reported surgical outcomes of 118 cases diagnosed with acute acquired comitant esotropia. Preoperative esotropia was measured using the base-out breakpoint method, and patients were scheduled for bilateral medial rectus recession according to Park’s standard dosage table. The mentioned surgical plan led to an overall short-term success rate of 90.7%, a long-term success rate of 82.2%, and a reoperation rate of 5.9%. Eleven cases in our series did not achieve favorable ocular alignment after their first surgery; of whom eight experienced under-correction, while three developed over-correction. Previous studies have reported success rates for surgical correction in cases of AACE ranging from 66% to 98% [10, 24,25,26,27,28,29]. The high percentage of under-correction following BMR recession in AACE cases observed in some previous studies suggests the possibility of mismeasurement of the exact preoperative angle of esotropia [25, 29, 30]. To address this issue, some authors have recommended using an augmented dosage of BMR recession for AACE patients, based on Park’s standard Tables [25, 29,30,31]. On the other hand, other efforts have focused on accurately determining the preoperative angle of deviation [26, 32,33,34,35,36,37,38,39].
The Prism Adaptation Test (PAT) is commonly used to measure the preoperative angle of esotropia in order to achieve better postoperative outcomes [26, 33, 34]. A comparative study involving AACE cases showed that surgery guided by the results of the PAT produced better treatment outcomes compared to simple alternate prism cover testing [33]. Various methods of PAT, including short PAT, partial PAT, and long PAT, exhibited similar effectiveness in determining the angle of esodeviation [34]. The PAT method is thought to reveal a hidden level of esotropia that is significantly greater than what is identified during the initial measurement. This allows for a more accurate evaluation of the patient’s true potential for fusion. It is important to emphasize that using this method requires cooperation from both the patient and the physician, as well as additional time and potential costs [26, 33, 34, 37].
Some authors have reported that the monocular occlusion method, which was commonly used for intermittent exotropia, can also effectively reveal latent deviations in cases of acute esotropia [39]. Additionally, a recent study demonstrated that in cases of AACE, patients who underwent augmented-dose surgery based on the single Maddox rod test achieved more favorable surgical outcomes compared to those who were assessed using the conventional alternate prism cover test, particularly when there was a difference of over 5 PD in preoperative esotropia as evaluated by the two methods [36]. Another study conducted by Dai and colleagues assessed the effectiveness of the base-out recovery point method for maximizing fusional convergence and accurately measuring the preoperative angle of deviation [32]. Their study involved 22 cases categorized as AACE, all of whom were treated based on the angle determined by the preoperative base-out recovery point. Of these cases, 19 achieved orthotropia, and three individuals experienced minimal esophoria. In the current study, we used a measurement technique for determining the preoperative angle of esotropia that closely resembled the method described by Dai and colleagues [32]. This method achieved successful postoperative outcomes in over 90% of cases. The base-out recovery point method for measuring the angle of deviation is more convenient and cost-effective than the prism adaptation test, as it can be completed quickly without requiring additional time or effort.
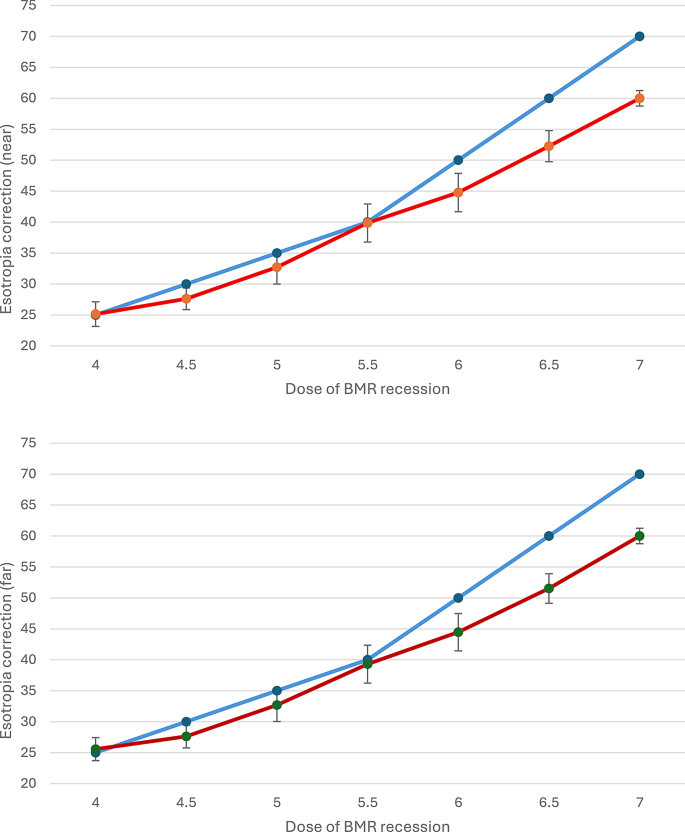
Our results indicated that patients with preoperative ET greater than 40 PD had an average residual esotropia of more than 5 PD (see Table 3; Fig. 2). Therefore, we recommend a slightly augmented surgical dosing for BMR recession when esotropia exceeds 40 PD. Our suggestion is as follows: For 45 PD of esotropia, a 6 mm BMR recession is recommended. For 50 PD, a 6.25 mm BMR recession is appropriate; for 55 PD, a 6.5 mm BMR recession; and for 60 PD, a 7 mm BMR recession. If esotropia exceeds 60 PD, combine the maximum BMR recession with a unilateral lateral rectus resection (Table 4).
Table 4 Surgical dose table based on the current results
Strabismus surgical planning for AACE largely depends on the surgeon’s experience and preference when choosing between BMR recession or unilateral recess-resect surgery [1,2,3]. While a few studies have suggested that unilateral recess-resect is preferable to BMR recession [16, 24], the limited number of AACE cases and the lack of direct comparisons between these two methods make it difficult to draw firm conclusions. Additionally, it’s important to consider the different techniques used to measure preoperative esotropia and the augmented surgical dosages applied in some studies when comparing these postoperative outcomes.
Our study had several limitations, primarily due to its retrospective nature, which resulted in variability in age and fusional potential of the included cases. Long-term follow-up data were available for fewer than half of the cases, which made it challenging to draw definitive conclusions. However, it is likely that patients who did not return for long-term follow-up visits had achieved stable ocular alignment and were satisfied with their surgical results. Variants such as the daily amount of near work, digital device usage, and history of prior psychosocial stress were not recorded in our medical and surgical sheets. Consequently, we were unable to categorize our cases using the traditional Burian and Miller classification. Additionally, preoperative measurements of esotropia were not compared with other alternative methods. The base-out breakpoint method for measuring esotropia could be challenging in patients with suppression, and the prism adaptation test would be a more suitable alternative in these cases [32]. And finally, there is insufficient information on the adoption and evolution of the base-out breakpoint method over time.
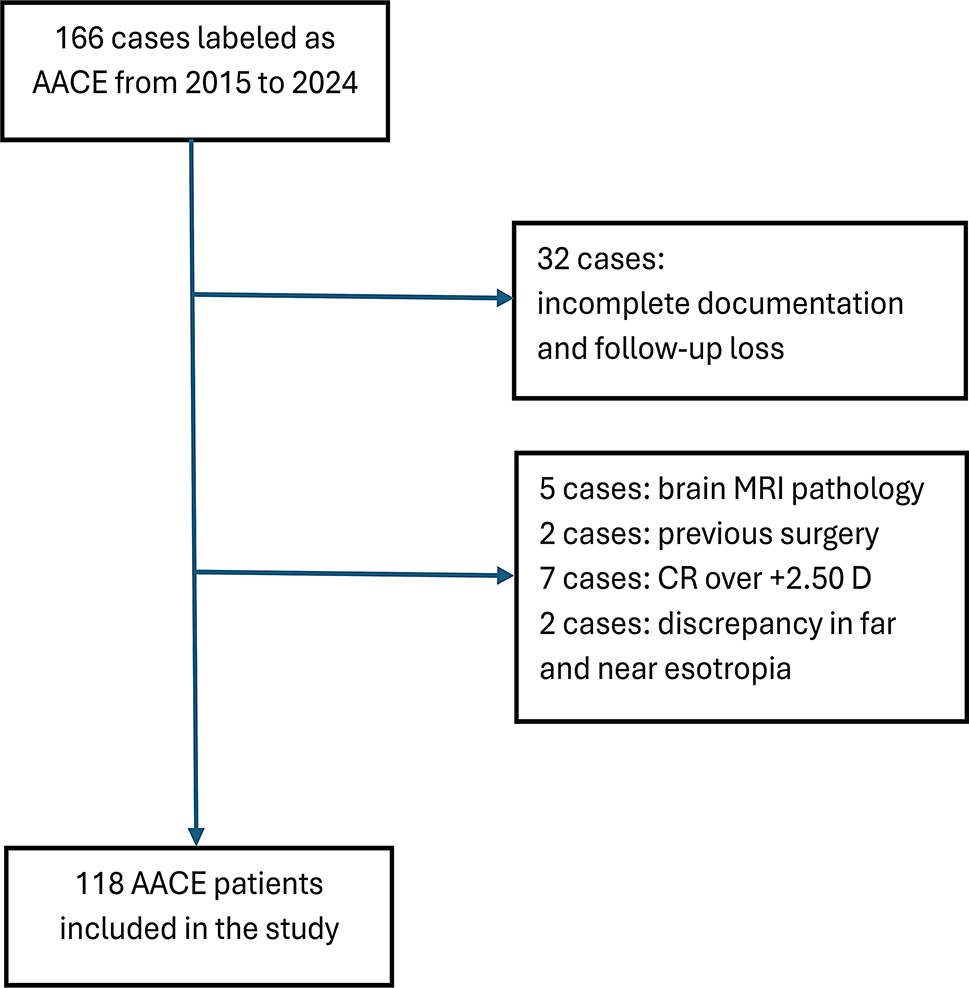
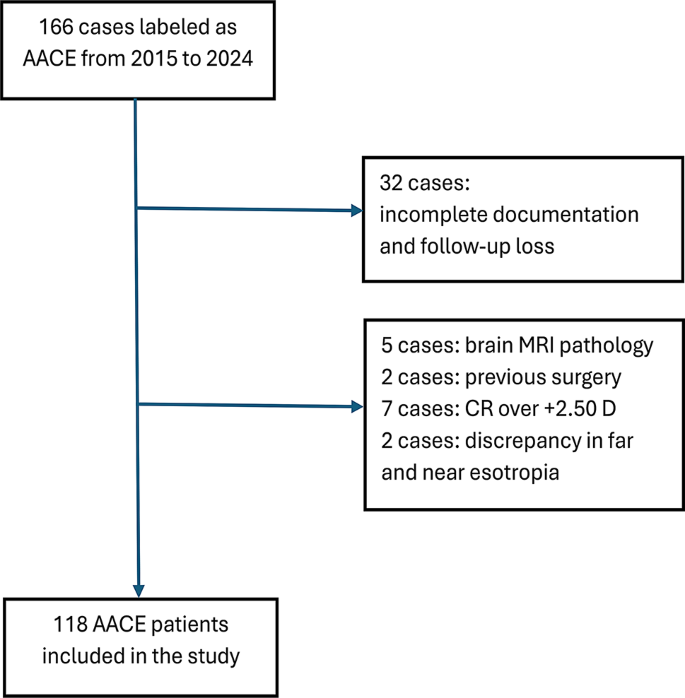
Flowchart of patient participation. AACE: Acute acquired comitant esotropia, MRI: Magnetic resonance imaging, CR: Cycloplegic refraction, D: Diopter
The X-axis illustrates the dosage of BMR recession, while the Y-axis represents the correction of esotropia in near (above figure) and far (bottom figure). The blue line indicates the recommended dosage for performing BMR recession according to Park. In contrast, the red line shows the average correction of esotropia observed in our study after performing the BMR recession dosage
The current study demonstrated that younger age was associated with a higher risk of surgical failure, as indicated in two previous studies [10, 40]. Other preoperative factors did not significantly impact the surgical outcomes. We reported an overall success rate of over 90% in AACE cases when performing standard bilateral medial rectus muscle recession, using preoperative measurements of esotropia assessed by the base-out breakpoint method. Future randomized clinical studies are recommended to determine the most suitable method for measuring preoperative esotropia and the best surgical approach. These studies should explore how preoperative esotropia measurements and surgical planning would affect the surgical success of patients diagnosed with acute acquired comitant esotropia.