Hyperthermia has been extensively utilized in the treatment of malignant tumors [14, 15], however, investigations into its correlation with RP are still relatively scarce. The result of our study indicate that hyperthermia can effectively reduce the incidence of grade ≥ 2 RP in patients receiving higher radiation doses.
The combination of radiotherapy and hyperthermia has changed the original single treatment model and improved the therapeutic effect. Studies have shown that when hyperthermia is combined with radiotherapy, it can enhance the anti-cancer effects of many types of cancer. Huilgol et al. [16] reported a Phase III randomized controlled study involving 54 patients with locally advanced head and neck tumors, aiming to evaluate the efficacy of local hyperthermia combined with radiotherapy. They found that the complete response rate in the combined group was significantly higher than that in the radiotherapy-only group (79% vs. 42%). Dong et al. [17] also reported on the long-term efficacy of hyperthermia combined with CRT in 80 patients with liver cancer. The data revealed that the rates of recurrence and mortality within the first six months and at the one-year mark were considerably lower in the group receiving combined therapy compared to the control group (p < 0.05). From the aforementioned studies, it can be seen that the combination of radiotherapy and hyperthermia can increase the therapeutic effect. However, the toxic and side effects related to the treatment should also be taken into account. Therefore, more in-depth research is needed to improve the treatment plan that combines radiotherapy and hyperthermia.
In our study, the incidence of grade ≥ 2 RP was 55.3% among patients in the RT group with a V20 exceeding 20%. A previous retrospective study showed that the incidence of grade ≥ 2 RP was 52.4% in patients with a V20 of less than 30% [18]. Another study reported a 51% incidence of grade ≥ 2 RP in patients with a V20 ranging between 26% and 30% [19]. In summary, the incidence of grade ≥ 2 RP in this study is consistent with the results of previous studies.
Our research results indicate that in patients with V20 > 20%, the incidence of grade ≥ 2 RP in the RHT group was significantly lower than that in the RT group, suggesting that hyperthermia can improve patients’ tolerance and has a certain preventive or therapeutic effect on the occurrence of RP. Meanwhile, we found that in the RT-alone group, the incidence of grade ≥ 2 RP was significantly higher when V20 > 20 Gy compared to V20 ≤ 20 Gy (55.32% vs. 34.29%, P = 0.024). In contrast, no statistically significant difference in the incidence of grade ≥ 2 RP was observed between different V20 levels within the RHT group. This suggests that hyperthermia may interact with V20 levels in reducing the risk of RP. On the other hand, with the increase in the number of hyperthermia times, the incidence of grade ≥ 2 RP also considerably decreased. It can be seen that hyperthermia can significantly decrease the incidence of RP in patients, especially reducing the incidence of grade ≥ 2 RP, and with the increase in the number of hyperthermia times, the incidence of moderate-to-severe RP considerably decreases. Multivariate analysis revealed that in patients with V20 > 20%, gender, PS score, and number of hyperthermia times are factors affecting the occurrence of RP in patients with thoracic tumors undergoing thoracic radiotherapy.
However, when not imposing limits on dosimetric variables, our analysis revealed no substantial differences in the incidence of RP across all severity levels and specifically for grade ≥ 2 between the two cohorts. This unexpected result may be explained by the following factor. Typically, V20 is considered one of the important dosimetric indicators for predicting RP. When V20 reaches a certain threshold, it may lead to a more significant risk of RP. Boonyawan et al. [20] analyzed the correlation between postoperative radiotherapy combined with concurrent chemotherapy and RP in 199 lung cancer patients and found that if the lung dose for patients was limited to V10 < 30% and V20 < 20%, the incidence of RP would be only 6%. In such cases, due to the low incidence of RP, the effect of hyperthermia on reducing the incidence of RP is not significant.
Our study found that although the incidence of grade ≥ 2 RP was lower in the RHT group, the incidence of grade < 2 RP appeared to be higher. Regarding this phenomenon, we propose the following possible explanations: On one hand, hyperthermia may stimulate cells such as macrophages and fibroblasts to increase the production of matrix metalloproteinases (MMPs), thereby contributing to tissue repair and regeneration [21]. In patients with grade < 2 RP, the lung architecture remains largely intact without large-scale collagen deposition; thus, the degradative effect of MMPs is not pronounced. On the other hand, the observed increase in the incidence of grade < 2 RP may be attributed to the fact that some cases initially classified as grade ≥ 2 RP were downgraded to grade < 2 RP following hyperthermia treatment.
Considering the significance of hyperthermia in decreasing the incidence of RP, it is imperative to conduct an in-depth exploration of its mechanisms of action.Hyperthermia is more likely to improve patient tolerance and reduce lung damage by inducing the expression of heat shock proteins (HSPs) and improving local blood flow. Numerous studies indicate that hyperthermia triggers the production of HSPs, such as HSP27, HSP70, and HSP90 [22, 23]. Furthermore, HSP70 may mitigate the occurrence of radiation-induced lung injury [24]. Several studies indicate that HSP70 may participate in DNA repair: it enhances base-excision repair by interacting with human apurinic/apyrimidinic endonuclease and by stimulating single-strand gap-filling via DNA polymerase β, thereby promoting the repair of damaged cells [25]. In addition, HSP70 possesses marked cytoprotective properties. Toll-like receptor 4 (TLR4) confers protection against hyperoxia-induced lung injury and mortality, and HSP70—acting as an endogenous ligand for TLR4—binds to the receptor to shield pulmonary tissue from lethal oxidative stress [26]. Moreover, HSP70 suppresses epithelial–mesenchymal transition (EMT) by inhibiting reactive oxygen species production, further amplifying its protective effects [27]. However, HSP70 may inhibit multiple aspects of the apoptotic pathway, thereby potentially compromising the therapeutic efficacy of treatment [28]. Their effect is also transient, with expression peaking within hours and declining thereafter [29]. This is why, in clinical practice, hyperthermia times are typically scheduled one to three times per week to sustain their biological influence. Thus, while HSPs induction likely contributes to the observed reduction in RP, it should be interpreted as a partial mechanism rather than the sole explanatory factor. On the other hand, under elevated ambient temperatures or pathological conditions, the body dissipates heat via vasodilation—a regulatory response that concurrently alters blood rheology. When vessels dilate, the enlarged lumen reduces the contact area between blood and the vascular wall, leading to a decrease in blood viscosity and a corresponding increase in flow. Hyperthermia harnesses this mechanism by inducing pulmonary vasodilation and accelerating circulation, thereby promoting the rapid transport and metabolism of inflammatory mediators. This clearance process prevents the excessive accumulation of cytokines at the lesion site, suppresses the development of an uncontrolled cytokine storm, and ultimately lowers the risk of RP.
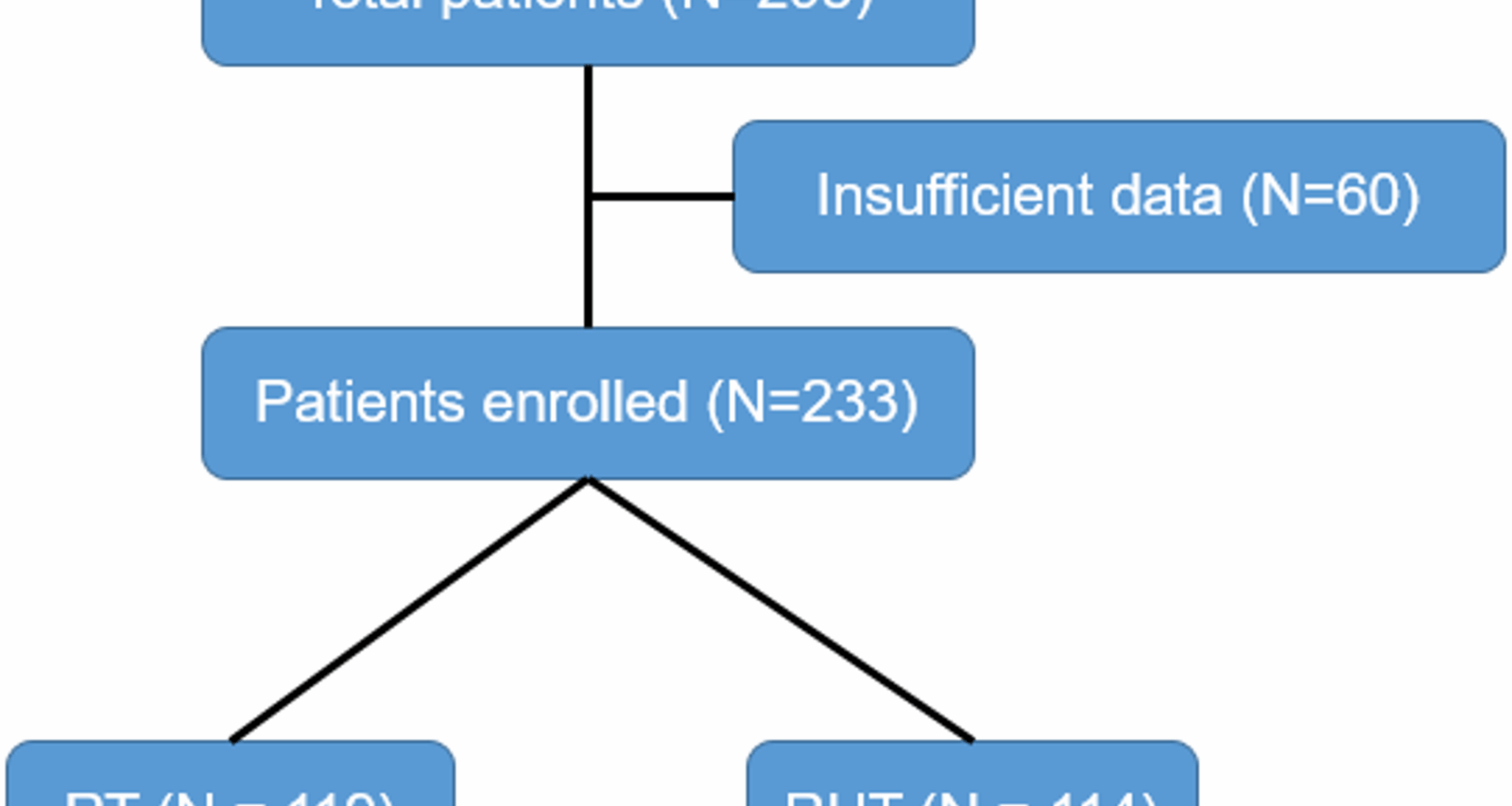
It should be noted that this study is not without limitations. As it is a retrospective study on RP, the baseline data balance of the patients in this study was not optimal. Furthermore, due to the relatively small sample size for some analyses, there may be some error regarding the impact of the number of hyperthermia times on the occurrence of RP. In order to address these limitations, the number of cases studied will be expanded in the next steps of research, with the aim of making the study more systematic and standardised.