In this study, we evaluated whether the time from index blood culture to the initiation of glycopeptide therapy affected 30-day in-hospital mortality in patients with MRSA bacteremia. After correcting for the immortal-time bias, we found no significant association between early glycopeptide initiation and 30-day mortality rates. Instead, host factors, such as metastatic solid tumor, along with host–pathogen interaction factors, such as initial septic shock, pneumonia, and unknown focus, emerged as significant predictors of mortality, which is consistent with previous studies [3, 17, 18]. In addition, we observed that the majority of deaths occurred within the first two weeks after the initial positive blood culture, a finding similar to previous reports [24].
Previous studies evaluating the effects of time to AAT in MRSA bacteremia have reported inconsistent results (Supplementary Table 6, Additional File 1) [4,5,6,7,8,9,10,11,12,13,14]. These discrepancies likely reflect differences in patient populations and methodological approaches, which require careful consideration. First, several MRSA bacteremia studies that reported no significant benefit of early AAT did not account for the immortal-time bias [4, 5, 8, 10]. Such bias can attenuate the effectiveness of early therapy because patients who survive longer inherently remain at risk of receiving delayed AAT [15]. Second, because the survival benefit of early AAT is most evident in patients with septic shock or organ dysfunction [11, 15, 16], cohorts that include a larger proportion of such patients are more likely to show a marked survival benefit from early therapy. This study used a landmark analysis to adjust for immortal-time bias and was performed in a cohort with a relatively high incidence of septic shock (28.2%). Nevertheless, we found no significant association between time to AAT and 30-day mortality, and a sensitivity analysis that excluded patients who received glycopeptide therapy > 120 h after the index blood culture produced similar results.
Additionally, the distribution of infection foci in SAB may have attenuated the effect of time to AAT because both mortality and incidence rates of metastatic complications vary substantially by focus [3, 25, 26]. In the majority of previous studies on MRSA bacteremia that failed to demonstrate a significant benefit of early AAT, catheter-related bloodstream infections (CRBSIs) accounted for a relatively large proportion of cases (Supplementary Table 6, Additional File 1) [4, 5, 10] and were associated with particularly low risk of mortality [3, 25]. This study included a relatively high proportion of osteoarticular infections (25.5%) compared with previous studies. Although osteoarticular infections are traditionally classified as intermediate-risk sources of SAB, together with soft tissue infections and unknown foci [3], osteomyelitis and prosthetic joint infections often follow a subacute course that lasts several weeks [27]. Furthermore, because osteoarticular infections often require source control [28], non-antibiotic interventions, combined with their typically slow clinical progression, may have blunted the impact of time to AAT on outcomes.
To control other antibiotic-related factors, we limited the initial antibiotic therapy to glycopeptides and evaluated the administered dosage. At both hospitals, vancomycin dosing was adjusted by TDM, and the median trough concentration exceeded 10 µg/mL. In contrast, teicoplanin was administered as weight-based doses without TDM, according to the clinician’s judgment. Consequently, teicoplanin was most often initiated at a 6 mg/kg loading dose, and in some cases, the loading dose was omitted, which may have resulted in suboptimal drug exposure in serious or complicated MRSA infections [29]. Given that teicoplanin therapy, compared with vancomycin, showed a trend toward higher mortality and a shorter time to AAT in the univariable analysis, underdosing of teicoplanin could have attenuated the benefit of early AAT.
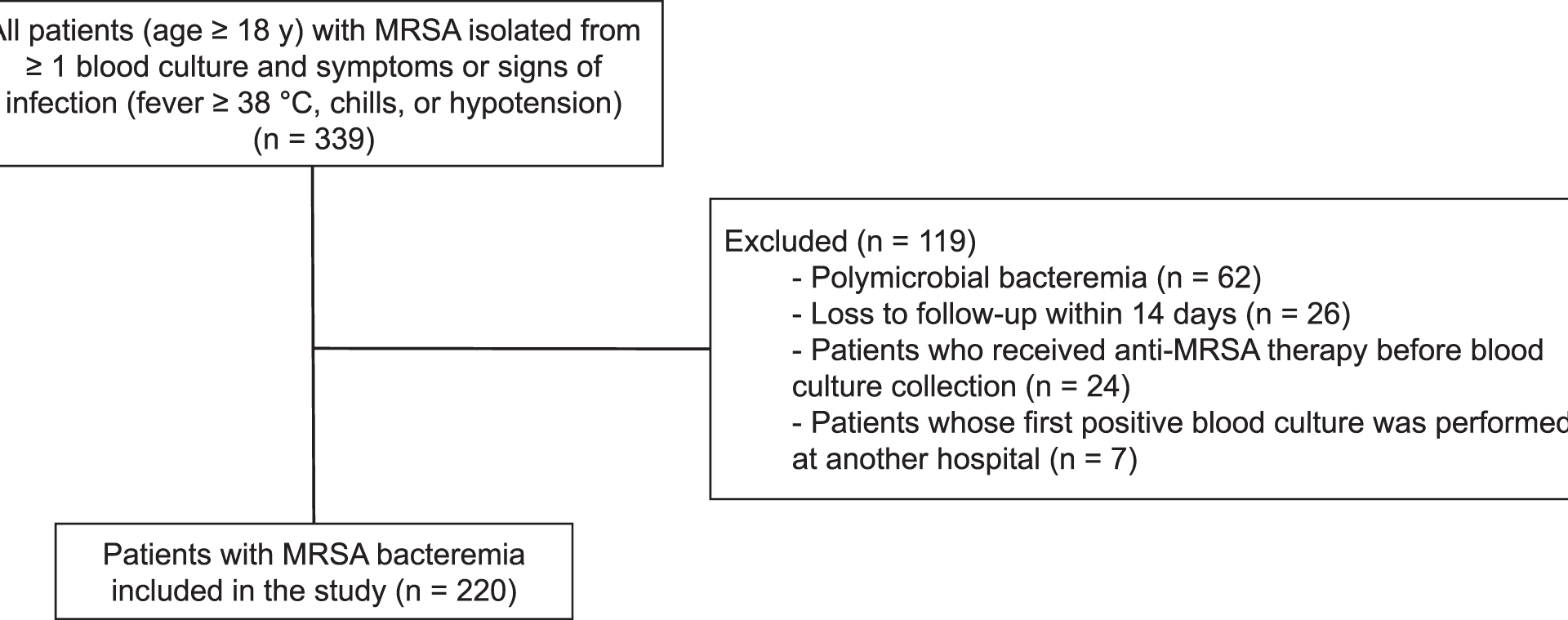
This study had several limitations. First, because this study relied on retrospectively extracted electronic medical records, residual confounding by indication may have persisted. Although we adjusted for key covariates, including the presence of septic shock, patients with severe illness were more likely to receive broad-spectrum agents such as glycopeptides earlier, potentially attenuating the benefits of early AAT. Second, although the cohort spans five years of MRSA bacteremia across two university-affiliated centers, the absolute number of deaths was modest, resulting in wide confidence intervals around several effect estimates. Consequently, the study may have lacked sufficient power to detect clinically meaningful but minimal benefit of early AAT. Third, because this study, similar to most previous investigations, defined the baseline as the time of blood culture collection, the interval from symptom onset to culture acquisition is likely to be longer in community-onset infections than in nosocomial cases [4,5,6,7,8,9,10, 12, 13]. Moreover, this unmeasured pre-hospital delay may vary considerably across studies owing to differences in healthcare accessibility among countries and regions. Thus, variations in the proportion of community-onset infections, together with regional differences in healthcare accessibility, may have influenced the observed effects of early AAT. Fourth, as this study was conducted in only two hospitals within a single country, the generalizability of our findings to other healthcare settings or countries may be limited. Fifth, we did not perform a separate sensitivity analysis restricted to patients with septic shock. The limited number of events in this subgroup would have constrained the number of covariates that could be included and increased the risk of overfitting, potentially resulting in unstable or misleading estimates. Sixth, although vancomycin TDM was changed from trough concentration–based dosing to AUC–based dosing during the study period, trough concentration was used as the monitoring parameter for analysis to ensure consistency across all patients. In addition, the timing of TDM varied among patients, making it difficult to consistently determine the exact time to reach therapeutic levels. Seventh, this study included only patients with clinical signs or symptoms of infection, and therefore those with MRSA bacteremia without overt manifestations may have been excluded.