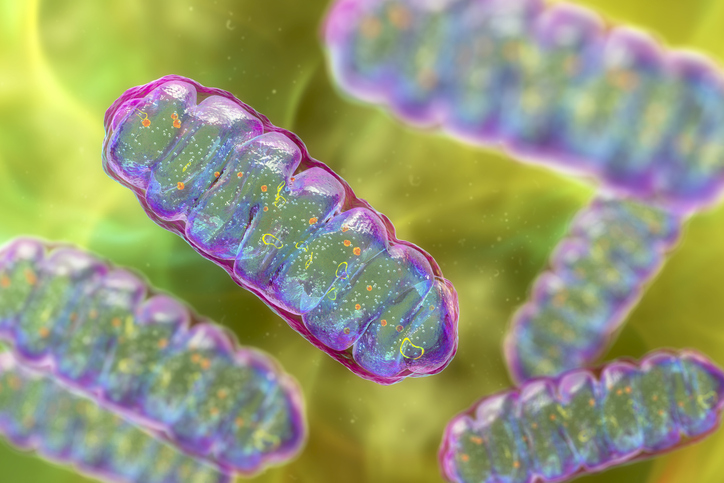
Barth Syndrome is a rare X-linked genetic condition caused by a mutation in the Tafazzin gene, which is essential for healthy mitochondria. When this gene fails to function properly, it produces less of a needed phospholipid called cardiolipin (CL) and much more of a harmful lipid called monolysocardiolipin (MLCL) in tissues. Build-up of MLCL disrupts the function and structure of mitochondria, making it harder to generate needed energy.
Patients with the condition, which affects mostly boys, experience muscle weakness, frequent infections, and cardiomyopathy. Heart transplants can help manage cardiac symptoms, but many children with the syndrome do not live past early childhood. However, findings reported in a recent Nature paper point to a potential path to developing targeted therapies for this rare condition. The paper, which is titled “Genetic suppression features ABHD18 as a Barth syndrome therapeutic target,” is the result of an international collaboration involving scientists from academia and industry, including the Hospital for Sick Children and the University of Toronto.
In it, scientists reveal that blocking the activity of the ABHD18 gene restored mitochondrial health and improved heart function in preclinical models. Before this study, “ABHD18 was initially an uncharacterized gene and had no described function,” said Sanna Masud, a former PhD candidate in the lab of Jason Moffat, PhD, senior scientist and program head for the genetics and genome biology program at the Hospital for Sick Children. However, after several experiments, including screening for genes that interact with Tafazzin, “we discovered that ABHD18 encodes a key regulator of CL metabolism.”
Specifically, the scientists found that ABHD18 acts as a suppression gene that affects the pathway involved in CL production, meaning it can reduce or counteract the effects of a malfunctioning gene. As they explain in the paper, “ABHD18 converts CL into monolysocardiolipin (MLCL) in vitro, and its inactivation in cells and mice results in a shift to nCL in serum and tissues.”
Fixing Tafazzin directly is complex, the scientists say, so targeting ABHD18 could be a viable therapeutic alternative. And the preclinical data seems to confirm it. By blocking ABHD18 with a small-molecule drug called ABD646, the scientists report that they successfully reduced MLCL levels in multiple preclinical models of Barth syndrome. Furthermore, they also report observing improved mitochondrial health and heart function in studies using a zebrafish model and patient-derived cells. ”It’s one of the most striking examples of a disease modifier that this research team has ever seen,” said Vincent Blomen, PhD, study co-lead and senior director of discovery sciences at Scenic Biotech.
Moffat, who is also a professor in the department of molecular genetics at the University of Toronto, added, “ABHD18 gives us a direct path to correcting the underlying problem of this rare condition and can provide real hope for patients and families. This is a perfect example of how research can inform new therapies and care for some of the rarest conditions.”