The Abridged version:
A Sacramento resident was diagnosed with seasonal depression after feeling like a “plane crashed” on top of him. He said when he moved to the region, his symptoms got worse.
An expert says seasonal depression “interferes with almost every aspect of life,” and explores what to add and take away from your routine to feel better. Examples include taking daily walks and limiting your alcohol intake.
Nutrition can help you cope. Reach for foods like fruits, vegetables and legumes to stave off feelings of sadness and fatigue during the winter season.
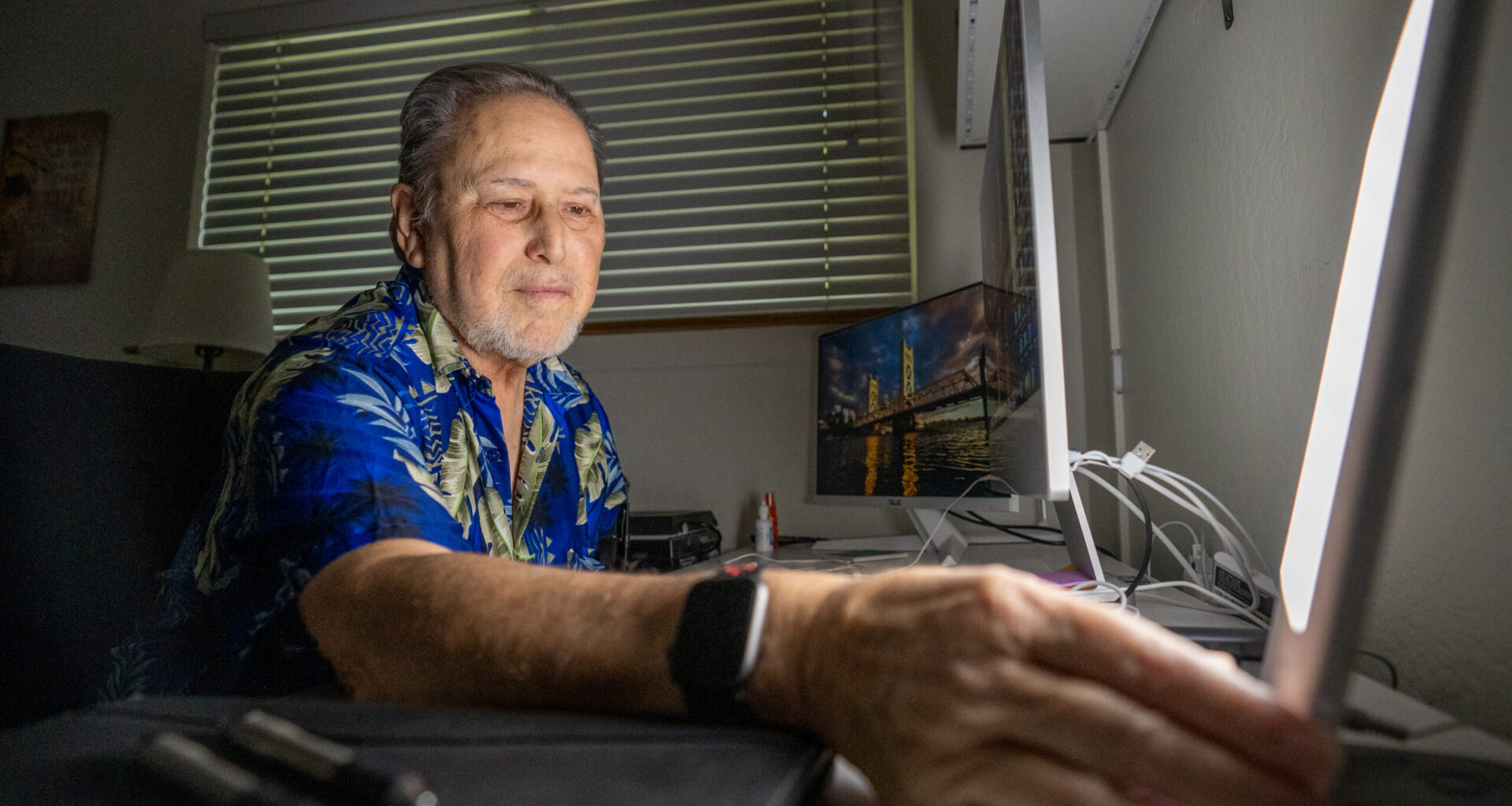
Soon after moving to Sacramento from Los Angeles for a new job, Michael Hansen realized something wasn’t quite right.
In the winter of 1994, then 38-year-old Hansen fell into a depression that seemed to correlate with the shift from summer to fall, but he wasn’t sure. It would take years before he had a name for his symptoms, which like clockwork left him feeling deregulated for months at a time.
In 1997, he was diagnosed with seasonal depression.
Seasonal depression — medically called seasonal affective disorder — is a common type of depression that follows a seasonal pattern, with symptoms that are typically triggered in the fall and improve in the spring, according to the National Institute of Mental Health.
“What I was not ready for was the endless winter gloom” in Sacramento, said Hansen. He recalled going 21 days straight that year “without even a hint of the sun,” which, much like this year, saw a record stretch of foggy and gloomy weather.
“It was like a plane crashed on top of me,” he said. “I fell into a terrible depression.”
Hansen didn’t leave the house, and eventually, he began neglecting work.
“Moving to Sacramento really highlighted the problem, and, you know, set me on a path to figuring out what the heck was going on,” he said.
Hansen is one of millions of people across the U.S. who, as the days get shorter and nights get longer, brace for symptoms more substantial than the colder weather itself.
 Michael Hansen in his office. (Cameron Clark)
Michael Hansen in his office. (Cameron Clark)
Seasonal depression ‘interferes with almost every aspect of life’
Seasonal depression affects about 5% of U.S. adults — roughly 13 million people — for roughly 40% of the year, according to the American Psychiatric Association.
While seasonal depression is treatable, it “interferes with almost every aspect of life,” said Gloria Petruzzelli, a licensed clinical psychologist with UC Davis Health Department of Psychiatry and Behavioral Sciences. If the following symptoms persist for two weeks, she said, seek help from a trained mental health professional:
Low mood
Loss of interest in hobbies and habits
Fatigue
Sleep and appetite changes
Difficulty concentrating
Restlessness or sluggish
Pattern of hopeless and worthless thoughts
“No matter what role or how long I’ve practiced, (seasonal depression) is something that we see recurring because of the time of the year,” said Petruzzelli, who’s been practicing in the Sacramento area for more than 15 years.
Young adults, women and people living in geographic locations with fewer daylight hours in the winter are at high risk of seasonal depression, according to the National Institute of Mental Health. Some people experience symptoms in the summer, but it’s not as common.
Hansen’s seasonal depression typically starts creeping in shortly after Halloween with symptoms of fatigue and low motivation. Sometimes, he said, all he can manage to do is lie in bed and watch television all day.
“You can find a way through this, but you have to be an advocate for yourself because even in this day and age, it’s difficult with doctors to get to a place where they understand what you’re experiencing, said Hansen, now 69, who’s been working with Stop Stigma Sacramento since 2015 to educate the region about mental illness. “You have to be brutally honest … and a lot of people won’t open up that way.”
Hansen was also diagnosed with bipolar disorder in 2015, which is a mental illness that causes periods of intense emotional shifts in mood, energy and ability to function, according to the American Psychiatric Association.
Mental illness is a common health condition in the region and affects all ages, according to Stop Stigma Sacramento, a mental health resource funded by the Sacramento County Division of Behavioral Health Services.
People are more likely to experience seasonal depression than generalized depression, especially those who haven’t experienced a significant trauma in their life, said La Viola Ward, a licensed professional clinical counselor.
“Just because (seasonal depression) comes seasonally doesn’t mean that it can’t feel really heavy,” said Ward, who serves clients in Sacramento and across the state of California through her private practice.
Seasonal changes and well-being
As the colder weather brings brighter mornings and darker nights, it’s normal not to feel like yourself.
That’s coming from Petruzzelli, who said the effects of seasonal changes highlight the connection between the body and the environment. The dip in sunlight hours during the colder months decreases serotonin and increases melatonin, triggering mood dips and fatigue.
The winter holiday season can exacerbate symptoms as people feel the extra pressure to be social and festive. For some, Ward said, the holidays bring financial stress and family conflict.
“You’re trying to physically stay warm, you’re trying to fiscally manage, and you’re trying to make sure that your mental health is balanced and managed,” she said. “It’s a very difficult thing.”
About 10% to 20% of people in the U.S. may experience winter blues, a mild form of seasonal depression where its effects aren’t as widespread, according to the Cleveland Clinic, an academic medical center.
The circadian rhythm is the body’s 24-hour clock that not only influences its wake-sleep cycle, but also other processes, including hormones, digestion and temperature, according to the Cleveland Clinic. Light or lack thereof affects its function the most.
Other factors include stress, mental health conditions and food intake.
“For anybody, no matter how good your mental health is, if your rhythm is disrupted, it’s going to cause some amount of stress,” said Kasturi Banerjee, a clinical health psychologist with the University of California, Los Angeles Health.
Psychological processes play a key role in how the body functions, said Banerjee, who specializes in digestive diseases. Factors such as nature, social and political events, and human interactions affect emotions.
Chronic stress keeps the digestive system in a state of flux, Banerjee said, leading to dysfunction in how the brain and the gut communicate through the nervous system over time. It also causes disruptions in behaviors such as eating and sleeping patterns.
“All of those things have an impact on how well our body is functioning,” she said.
Treating seasonal depression
Take charge of your mental health with a consistent routine, said Petruzzelli, who specializes in health and performance psychologies.
“We are whole people and what we put in our body and how we move our body … it’s all integrated,” she said.
Light therapy, vitamin D supplementation, therapy and medication are traditionally used to treat seasonal depression, according to UC Davis Health. Here are several behavioral changes to make, Petruzzelli said, to also combat symptoms:
Regular exercise
Daily walks outdoors
Consistent wake and sleep scheduled
Mindful movement (yoga and meditation)
Be social
Limit alcohol intake
Prioritize nutritious foods
“They’re boring things that we always hear, but they’re really important to being able to manage how we feel,” she said.
Ward, who experienced her own bouts of seasonal depression, said keeping the body warm and talking about your feelings helps.
“Suffering in silence, I think, is one of the worst things that people with any form of depression or anxiety can do because our internal dialog can oftentimes sound very factual,” she said. “If you allow yourself to just sit and listen to it, it can tell you really, really bad things.”
For Hansen, relief comes in many forms, including his 2-year-old Cavapoo named Luna.
“She is the absolute light of my life,” he said, “and the idea that you have a little creature that you’re responsible for that really depends on you helps with this as well.”
 Michael Hansen holds his dog, Luna. (Cameron Clark)
Michael Hansen holds his dog, Luna. (Cameron Clark)
Link between food and mood
What you eat affects your mental health.
The entire body, including the brain, needs adequate nutrition to run properly, said Carmen Moyers, a registered dietitian with Dignity Health Mercy Medical Group in Sacramento. Nutrients such as protein, healthy fats and carbohydrates influence mental capacity in both focus and mood.
Reach for fruits, vegetables and legumes, whole grains and omega-3 fatty acids to help stave off feelings of sadness and fatigue, said Moyers, who provides medical nutrition therapy to patients.
Omega-3 fatty acids are important fats used by the body to produce energy and tissue, according to the National Institute of Health. The problem, Moyers said, is that these essential nutrients that significantly affect the brain are typically lacking in the standard American diet.
The following foods provide omega-3 fatty acids, according to the National Institutes of Health:
Fatty fish (salmon, sardines and tuna)
Nuts and seeds (flaxseed, chia seeds and walnuts)
Oils derived from plants (flaxseed, soybean and canola oils)
Foods with nutrients added to them (certain eggs, yogurt and juices)
For some, Moyers said, mental health conditions affect food intake.
“Something is always better than nothing,” she said. “And if you’re depressed, I would much rather you eat a microwave dinner than nothing at all because you feel like it’s not healthy enough.”
Brianna Taylor is a regular contributor, covering Health and Wellness for Abridged.