Infurna FJ, Gerstorf D, Lachman ME. Midlife in the 2020s: opportunities and challenges. Am Psychol. 2020;75:470–85.
Lachman ME. Development in midlife. Annu Rev Psychol. 2004;55:305–31.
Bumpass LL, Aquilino W. A social map of midlife: family and work over the middle life course. John D. and Catherine T. MacArthur Foundation Research Network on Successful ….
Glymour MM, Ertel KA, Berkman LF. What can life-course epidemiology tell Us about health inequalities in old age. Annu Rev Gerontol Geriatr. 2009;29:27–56.
Puterman E, Gemmill A, Karasek D, Weir D, Adler NE, Prather AA, et al. Lifespan adversity and later adulthood telomere length in the nationally representative US health and retirement study. Proc Natl Acad Sci U S A. 2016;113: E6335–42.
Springer KW. Childhood physical abuse and midlife physical health: testing a multi-pathway life course model. Soc Sci Med. 2009;69:138–46.
Morozink JA, Friedman EM, Coe CL, Ryff CD. Socioeconomic and psychosocial predictors of interleukin-6 in the MIDUS National sample. Health Psychol. 2010;29:626.
Friedman EM, Montez JK, Sheehan CM, Guenewald TL, Seeman TE. Childhood adversities and adult cardiometabolic health: does the quantity, timing, and type of adversity matter? J Aging Health. 2015;27:1311–38.
Lachman ME, Schiloski KA. The psychosocial anti-inflammatories: sense of control, purpose in life, and social support in relation to inflammation, functional health and chronic conditions in adulthood. J Psychosom Res. 2024;187: 111957.
Kemp JM, Taylor VH, Kanagasabai T. Access to healthcare and depression severity in vulnerable groups the US: NHANES 2013–2018. J Affect Disord. 2024;352:473–8.
McLaughlin KA. The public health impact of major depression: a call for interdisciplinary prevention efforts. Prev Sci. 2011;12:361–71.
Horne G, Gautam A, Tumin D. Short- and long-term health consequences of gaps in health insurance coverage among young adults. Popul Health Manag. 2022;25:399–406.
Zhang X, Lemon TL. Health insurance and Self-Rated health from adolescence to early midlife in the U.S. Am J Prev Med. 2024;0.
Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the affordable care act on racial and ethnic disparities in health insurance coverage. Am J Public Health. 2016;106:1416–21.
Hill L, Artiga S, Published AD. Health Coverage by Race and Ethnicity, 2010–2022. KFF. 2024. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/. Accessed 27 Jan 2025.
Zhang X, Adams LB, Lemon TL. Health insurance coverage from adolescence to early midlife: variation across race and ethnicity. J Gen Intern Med. 2025:1–3.
Goldman HH, How Phantom Networks And Other Barriers Impede Progress On Mental Health Insurance Reform. Perspective examines Phantom networks and other barriers to access to mental health care. Health Aff (Millwood). 2022;41:1023–5.
Gao YN, Olfson M. Insurance and inpatient admission of emergency department patients with depression in the united States. Gen Hosp Psychiatry. 2022;78:28–34.
Espinoza-Kulick MAV, Cerdeña JP. We need health for all: mental health and barriers to care among Latinxs in California and Connecticut. Int J Environ Res Public Health. 2022;19:12817.
Carter SP, Cowan T, Snow A, Cerel J, Tucker R. Health insurance and mental health care utilization among adults who identify as transgender and gender diverse. Psychiatr Serv. 2020;71:151–7.
Winkelman TNA, Kieffer EC, Goold SD, Morenoff JD, Cross K, Ayanian JZ. Health insurance trends and access to behavioral healthcare among justice-involved individuals-United states, 2008–2014. J Gen Intern Med. 2016;31:1523–9.
Walker ER, Cummings JR, Hockenberry JM, Druss BG. Insurance status, use of mental health services, and unmet need for mental health care in the united States. Psychiatr Serv. 2015;66:578–84.
Meiselbach MK, Ettman CK, Shen K, Castrucci BC, Galea S. Unmet need for mental health care is common across insurance market segments in the united States. Health Aff Sch. 2024;2:qxae032.
Rowan K, McAlpine D, Blewett L. Access and cost barriers to mental health care by insurance status, 1999 to 2010. Health Aff Proj Hope. 2013;32:1723–30.
Hsiang WR, Lukasiewicz A, Gentry M, Kim C-Y, Leslie MP, Pelker R, et al. Medicaid patients have greater difficulty scheduling health care appointments compared with private insurance patients: a meta-analysis. Inquiry. 2019;56: 46958019838118.
Declercq E, Sakala C, Belanoff C. Women’s experience of agency and respect in maternity care by type of insurance in California. PLoS One. 2020;15: e0235262.
Graves JA, Nshuti L, Everson J, Richards M, Buntin M, Nikpay S, et al. Breadth and exclusivity of hospital and physician networks in US insurance markets. JAMA Netw Open. 2020;3: e2029419.
Atake E-H. Does the type of health insurance enrollment affect provider choice, utilization and health care expenditures? BMC Health Serv Res. 2020;20: 1003.
Wray CM, Khare M, Keyhani S. Access to care, cost of care, and satisfaction with care among adults with private and public health insurance in the US. JAMA Netw Open. 2021;4:e2110275.
Zhao J, Han X, Nogueira L, Fedewa SA, Jemal A, Halpern MT, et al. Health insurance status and cancer stage at diagnosis and survival in the united States. CA Cancer J Clin. 2022;72:542–60.
Fletcher SA, Cole AP, Lu C, Marchese M, Krimphove MJ, Friedlander DF, et al. The impact of underinsurance on bladder cancer diagnosis, survival, and care delivery for individuals under the age of 65 years. Cancer. 2020;126:496–505.
Sherman BW, Lawrence DF, Kuharic M, Chrones L, Patel S, Touya M. Mental health diagnoses and services utilization vary by wage level. Am J Manag Care. 2023;29:173–8.
Dasgupta S, Crim SM, Dawson L, Kates J, Weiser J, Klein PW, et al. Unmet needs for HIV ancillary care services by health care coverage and Ryan white HIV/AIDS program assistance. AIDS. 2022. https://doi.org/10.1097/QAD.0000000000003205.
Interrante JD, Admon LK, Carroll C, Henning-Smith C, Chastain P, Kozhimannil KB. Association of health insurance, geography, and race and ethnicity with disparities in receipt of recommended postpartum care in the US. JAMA Health Forum. 2022;3: e223292.
KIRBY JB KANEDAT. Unhealthy and uninsured: exploring Racial differences in health and health insurance coverage using a life table approach. Demography. 2010;47:1035–51.
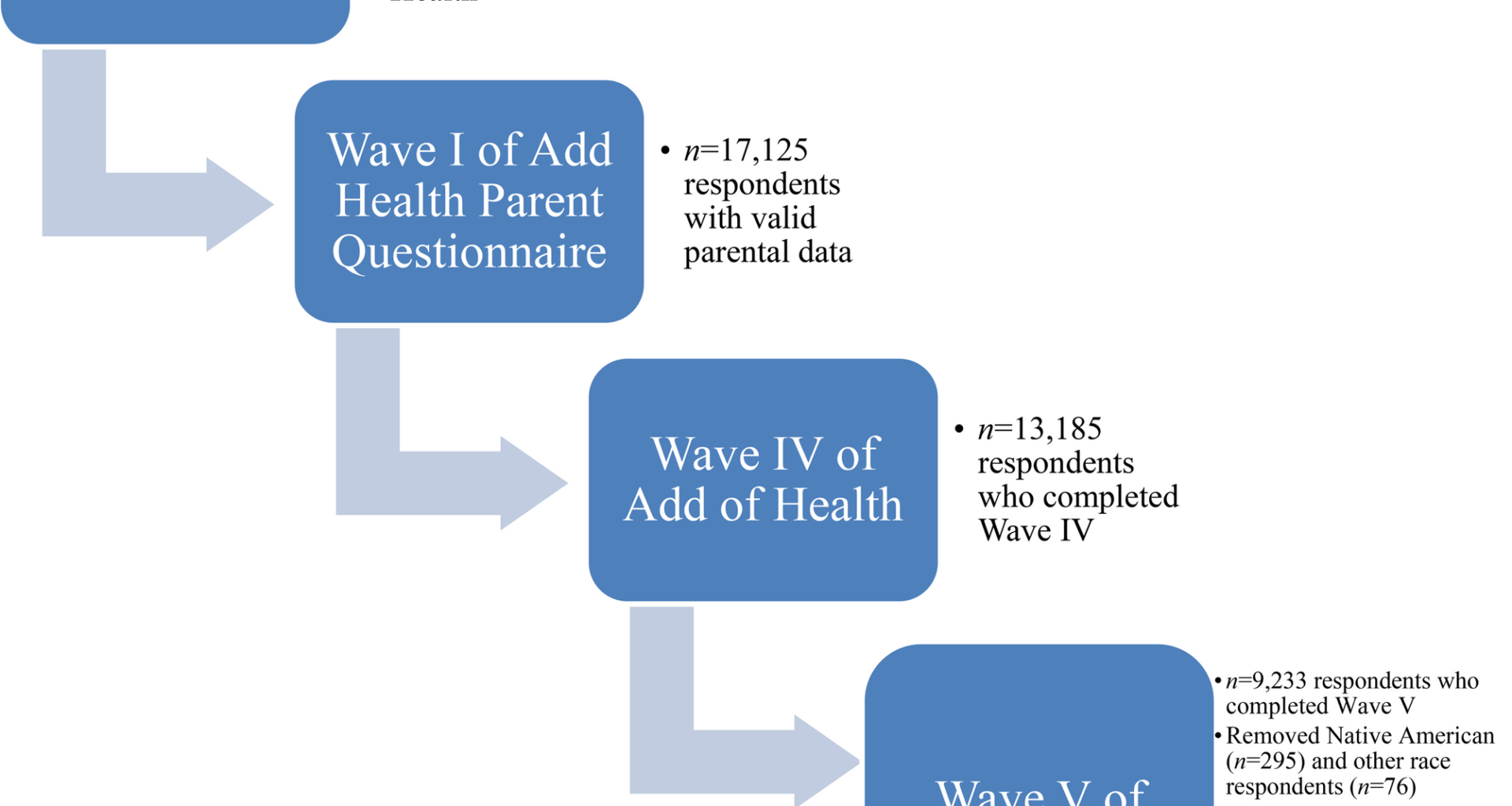
Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, et al. Cohort profile: the National longitudinal study of adolescent to adult health (Add health). Int J Epidemiol. 2019;48:1415–k1415.
Ross RK, Breskin A, Westreich D. When is a complete-case approach to missing data valid?? The importance of effect-measure modification. Am J Epidemiol. 2020;189:1583–9.
Wang N, Xie X. Associations of health insurance coverage, mental health problems, and drug use with mental health service use in US adults: an analysis of 2013 National survey on drug use and health. Aging Ment Health. 2019;23:439–46.
Radloff LS. The CES-D, scale. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Parsons HM, Maguire FB, Morris CR, Parikh-Patel A, Brunson AM, Wun T, et al. Impact of insurance type and timing of medicaid enrollment on survival among adolescents and young adults with cancer. Pediatr Blood Cancer. 2020;67: e28498.
Elze MC, Gregson J, Baber U, Williamson E, Sartori S, Mehran R, et al. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol. 2017;69:345–57.
Howell BA, Hawks LC, Balasuriya L, Chang VW, Wang EA, Winkelman TNA. Health insurance and mental health treatment use among adults with criminal legal involvement after medicaid expansion. Psychiatr Serv. 2023;74:1019–26.
Bruning J, Arif AA, Rohrer JE. Medical cost and frequent mental distress among the non-elderly US adult population. J Public Health. 2014;36:134–9.
Novak P, Anderson AC, Chen J. Changes in health insurance coverage and barriers to health care access among individuals with serious psychological distress following the affordable care act. Adm Policy Ment Health. 2018;45:924–32.
Korenman S, Hyson RT. Health insurance, labor market shocks, and mental health during the first year of the COVID-19 crisis. Econ Hum Biol. 2023;51: 101298.
Lee D-C, Liang H, Shi L. The convergence of racial and income disparities in health insurance coverage in the United States. Int J Equity Health. 2021;20: 96.
Gao Y, Burns R, Leach L, Chilver MR, Butterworth P. Examining the mental health services among people with mental disorders: a literature review. BMC Psychiatry. 2024;24: 568.
Betancourt J. Hispanic/Latino Adults Lack Adequate, Affordable Health Insurance Coverage. 2024. https://www.commonwealthfund.org/blog/2024/hispaniclatino-adults-lack-adequate-affordable-health-insurance-coverage. Accessed 18 Feb 2025.
Corallo B, Garfield R, Tolbert J, Published RR. Medicaid Enrollment Churn and Implications for Continuous Coverage Policies. KFF. 2021. https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-churn-and-implications-for-continuous-coverage-policies/. Accessed 18 Feb 2025.
McWilliams JM. Health consequences of uninsurance among adults in the United states: recent evidence and implications. Milbank Q. 2009;87:443–94.
Stuber J, Bradley E. Barriers to medicaid enrollment: who is at risk?? Am J Public Health. 2005;95:292–8.
Bacong AM, Menjívar C. Recasting the immigrant health paradox through intersections of legal status and race. J Immigr Minor Health. 2021;23:1092–104.
Buser JK. Treatment-seeking disparity between African Americans and whites: attitudes toward treatment, coping resources, and racism. J Multicult Couns Dev. 2009;37:94–104.
DeFreitas SC, Crone T, DeLeon M, Ajayi A. Perceived and personal mental health stigma in Latino and African American college students. Front Public Health. 2018;6: 49.
Snowden LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res. 2001;3:181–7.
Ward EC, Wiltshire JC, Detry MA, Brown RL. African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nurs Res. 2013;62:185–94.
Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing what matters most to identify culture-specific aspects of stigma. Int J Epidemiol. 2014;43:494–510.
Rivera KJ, Zhang JY, Mohr DC, Wescott AB, Bamgbose Pederson A. A narrative review of mental illness stigma reduction interventions among African Americans in the united States. J Ment Health Clin Psychol. 2021;5:20–31.
Broman CL. Race differences in the receipt of mental health services among young adults. Psychol Serv. 2012;9:38–48.
Williams L, Gorman R, Hankerson S. Implementing a mental health ministry committee in faith-based organizations: the promoting emotional wellness and spirituality program. Soc Work Health Care. 2014;53:414–34.
Pederson AB. Management of depression in Black people: effects of cultural issues. Psychiatr Ann. 2023;53:122–5.
Schwartz RC, Blankenship DM. Racial disparities in psychotic disorder diagnosis: a review of empirical literature. World J Psychiatry. 2014;4:133–40.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med 1982. 2018;199:219–29.
Alsan M, Wanamaker M. Tuskegee and the health of black, men. Q J Econ. 2018;133:407–55.
Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87:1773–8.
Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97:951–6.
Pederson AB, McLaughlin C, Hawkins D, Jain FA, Anglin DM, Yeung A, et al. Medical mistrust and willingness to use mental health services among a cohort of Black adults. Psychiatr Serv. 2025;76:318–25.
Vyas CM, Donneyong M, Mischoulon D, Chang G, Gibson H, Cook NR, et al. Association of race and ethnicity with late-life depression severity, symptom burden, and care. JAMA Netw Open. 2020;3: e201606.
Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35:317–27.
Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National survey of American life. Arch Gen Psychiatry. 2007;64:305–15.
Artiga S, Published NP. Gaps in Mental Health Care for Asian and Pacific Islander People and Other People of Color. KFF. 2023. https://www.kff.org/policy-watch/gaps-in-mental-health-care-for-asian-and-pacific-islander-people-and-other-people-of-color/. Accessed 28 July 2025.
Lee M, Bhimla A, Lu W, Ma GX. Correlates of mental health treatment receipt among Asian Americans with perceived mental health problems. J Behav Health Serv Res. 2021;48:199–212.
Ting JY, Hwang W-C. Cultural influences on help-seeking attitudes in Asian American students. Am J Orthopsychiatry. 2009;79:125–32.
Kim SB, Lee YJ. Factors associated with mental health help-seeking among Asian americans: a systematic review. J Racial Ethn Health Disparities. 2022;9:1276–97.
Gupta A, Szymanski DM, Leong FTL. The model minority myth: internalized racialism of positive stereotypes as correlates of psychological distress, and attitudes toward help-seeking. Asian Am J Psychol. 2011;2:101–14.
Kim PY, Lee D. Internalized model minority myth, Asian values, and help-seeking attitudes among Asian American students. Cultur Divers Ethnic Minor Psychol. 2014;20:98–106.
Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese Americans. J Community Psychol. 2004;32:27–43.
Lam AY, Jorm AF, Wong DF. Mental health first aid training for the Chinese community in Melbourne, Australia: effects on knowledge about and attitudes toward people with mental illness. Int J Ment Health Syst. 2010;4:18.
Tieu Y, Konnert C, Wang J. Depression literacy among older Chinese immigrants in canada: a comparison with a population-based survey. Int Psychogeriatr. 2010;22:1318–26.
Okazaki S, Kassem AM, Tu MC. Addressing Asian American mental health disparities: putting community-based research principles to work. Asian Am J Psychol. 2014;5:4–12.
Alang SM, McAlpine DD, Henning-Smith CE. Disability, health insurance, and psychological distress among US adults: an application of the stress process. Soc Ment Health. 2014;4:164–78.
Hughes PM, Hughes MS. Being uninsured is associated with clinical depression. Curr Psychol. 2023;42:12701–10.
Ojeda VD, Bergstresser SM. Gender, race-ethnicity, and psychosocial barriers to mental health care: an examination of perceptions and attitudes among adults reporting unmet need. J Health Soc Behav. 2008;49:317–34.
Wright B, Carlson E, Barlow MR, Flores MW, Spain DA, Lê Cook B. Ethnoracial differences in social determinants of health and acute mental health symptoms among adults hospitalized after emergency care. J Health Care Poor Underserved. 2024;35:903–19.
Cook BL, Trinh N-H, Li Z, Hou SS-Y, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv. 2017;68:9–16.
Lee SY, Xue Q, Spira AP, Lee HB. Racial and ethnic differences in depressive subtypes and access to mental health care in the United States. J Affect Disord. 2014;155:130–7.
Olfson M, Zuvekas SH, McClellan C, Wall MM, Hankerson SH, Blanco C. Racial-ethnic disparities in outpatient mental health care in the United States. Psychiatr Serv. 2023;74:674–83.
Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in US depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. 2022;63:726–33.
Assari S. Social determinants of depression: the intersections of race, gender, and socioeconomic status. Brain Sci. 2017;7: 156.
Iwata N, Turner RJ, Lloyd DA. Race/ethnicity and depressive symptoms in community-dwelling young adults: a differential item functioning analysis. Psychiatry Res. 2002;110:281–9.
Adams LB, Baxter SLK, Lightfoot AF, Gottfredson N, Golin C, Jackson LC, et al. Refining black men’s depression measurement using participatory approaches: a concept mapping study. BMC Public Health. 2021;21(1): 1194.
Adams LB, Gottfredson N, Lightfoot AF, Corbie-Smith G, Golin C, Powell W. Factor analysis of the CES-D 12 among a community sample of black men. Am J Mens Health. 2019. https://doi.org/10.1177/1557988319834105.
Adams LB, Farrell M, Mall S, Mahlalela N, Berkman L. Dimensionality and differential item endorsement of depressive symptoms among aging black populations in South Africa: findings from the HAALSI study. J Affect Disord. 2020;277:850–6.
Ali S, Cookson R, Dusheiko M. Addressing care-seeking as well as insurance-seeking selection biases in estimating the impact of health insurance on out-of-pocket expenditure. Soc Sci Med. 2017;177:127–40.
Afoakwah C, Byrnes J, Scuffham P, Nghiem S. Testing for selection bias and moral hazard in private health insurance: evidence from a mixed public-private health system. Health Econ. 2023;32:3–24.