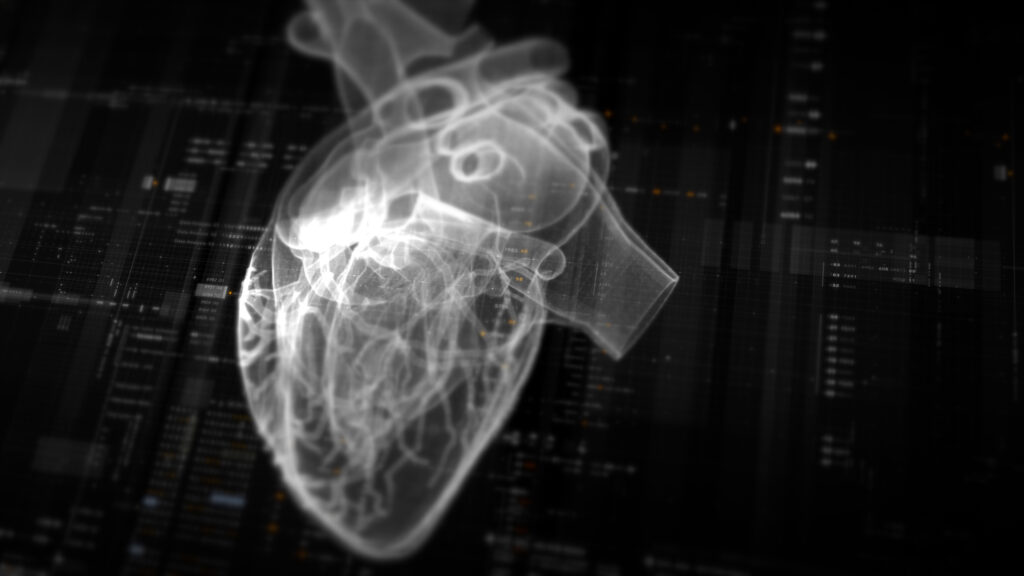
When patients visit Matthew Budoff for a CT angiogram of their heart, the preventive cardiologist may tell them about a new test. It’s not covered by insurance, he explains, but for an extra $850, an artificial intelligence algorithm can quantify and characterize the volume of plaque in their coronary arteries. How much of that plaque is calcified and stable? How much is the more dangerous soft plaque that could rupture and cause a heart attack or stroke?
Budoff is one of a relatively small number of cardiologists and radiologists who offer AI plaque analysis of those coronary CT studies. But next year, the technology is likely to see a significant boost as private insurance companies start to cover the algorithms from AI vendors Heartflow, Cleerly, and Elucid, and Medicare sets a national payment rate of just over $1,000.
The technology is coming of age as debate grows over the cost of devices powered by artificial intelligence and machine learning. AI device companies say that their algorithms’ price is justified by the downstream savings when the test results lead to better care and help avoid unnecessary, expensive procedures. But as insurance starts to cover more algorithms, some medical groups and physicians worry AI’s costs could balloon out of proportion with its benefits.
STAT+ Exclusive Story
Already have an account? Log in
This article is exclusive to STAT+ subscribers
Unlock this article — and get additional analysis of the technologies disrupting health care — by subscribing to STAT+.
Already have an account? Log in
Individual plans
Group plans
To read the rest of this story subscribe to STAT+.