Participants socio-demographics
Of the 386 pregnant women who agreed to participate in the study, most (79%) of the participants attended their 1st ANC visit after 8 weeks of gestation. The gestational age of approximately 44.3% of the participants was 24–34 weeks. Most of the participants (24.9%) were in the age group 30–34 years. More than half (53.4%) of the women were unmarried, while 73.8% had a secondary school education and 80.6% were unemployed. Less than half (41.7%) of the pregnant women were obese (> 30 kg/m2), and nearly a third of the women have been pregnant at least twice (26.2%), while 30.8% of the women have given birth to more than one child. A high proportion (81.6%) of the participants had never had a miscarriage before, and 82.6% had no family history of diabetes. A detailed description of the participants’ socio-demographic characteristics is shown in Table 2.
Table 2 Socio-demographic information of pregnant women participants
Table 2 outlines the socio-demographic characteristics of the participants receiving antenatal care at healthcare facilities under study. The socio-demographic data includes age, marital status, educational level, employment status, body mass index, gravity, parity, miscarriage and family history of diabetes. N = total number of pregnant women, % = percentage of pregnant women.
Level of awareness regarding GDM among participants receiving ANC during clinic visits
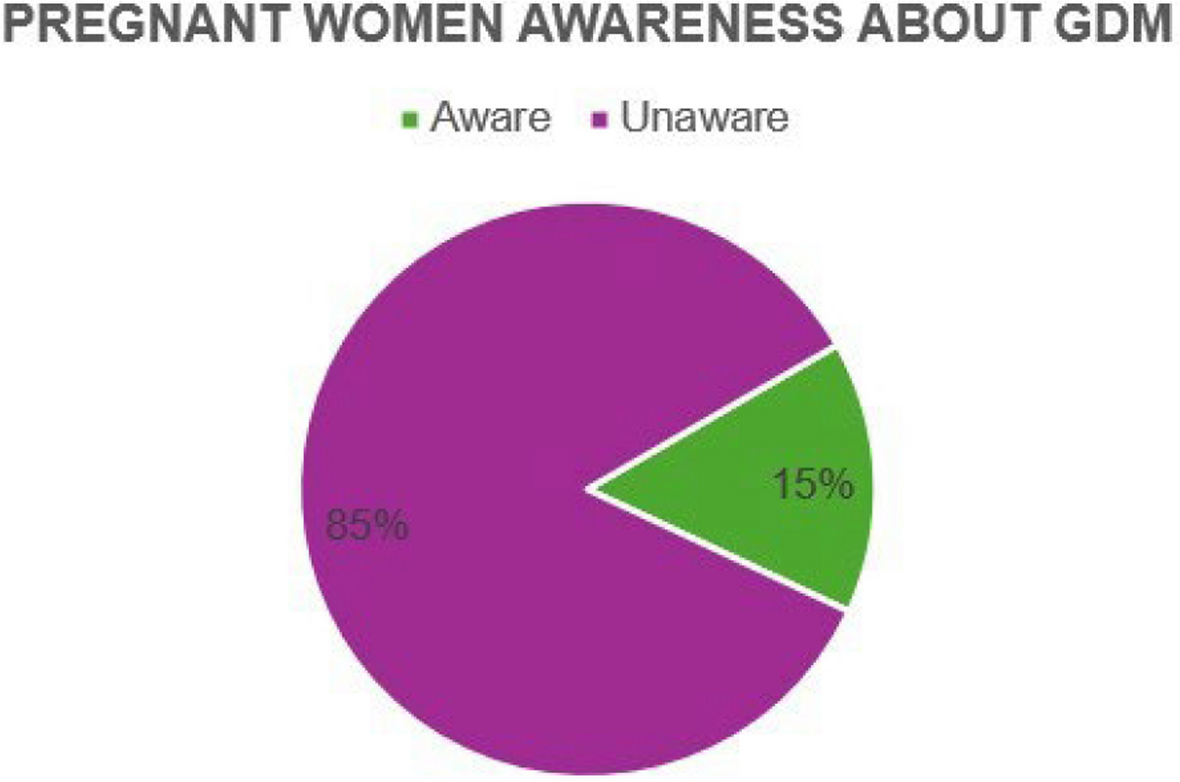
The majority of participants were unaware of GDM (84.7%) – with only 15.3% being aware, Fig. 1.
Awareness of pregnant women about gestational diabetes mellitus
For those who were aware of GDM (n = 59), various sources of information were identified and are shown, Table 2.
Table 3 outlines participants’ sources of information related to GDM. These sources include health workers, family, media (TV, online, radio, pamphlet) and school. No represents the number of pregnant women and % represents the percentage of pregnant women who have heard about GDM through the four identified sources of information.
Table 3 Sources of information of pregnant women who were aware of GDM
Approximately 70% of the participants had heard about GDM from healthcare workers while consulting at a clinic or hospital, and 18.6% heard about the condition from a family member who was either diagnosed or knew someone with diabetes mellitus. Also, approximately 9% of the participants learned about GDM from media sources (television, radio, newspaper, amphlet and/or online), with few (0.5%) having heard about GDM in school when learning Life sciences/biology.
Knowledge regarding GDM and its management among pregnant women receiving ANC at clinics
When asked about the occurrence of GDM, 66% of the pregnant women reported that GDM could not occur for the first time in pregnancy, while 34.2% of pregnant women had different views as they said it is possible that GDM could occur for the first time in pregnancy, Table 4.
Table 4 Pregnant women’s knowledge about risk factors, testing, treatment and long-term consequences of GDM
Table 4 summarises the participants’ knowledge regarding risk factors associated with GDM, testing methods, treatment or management and long-term consequences in mothers who had GDM during pregnancy and children born from mothers who had GDM. Firstly, (Yes) represents the percentage of pregnant women who agreed with questions related to risk factors, testing methods, treatment or management and long-term consequences associated with GDM. Secondly, (No) represents the percentage of pregnant women who disagreed with questions related to risk factors, testing method, treatment or management and long-tern consequences associated with GDM.
In our study, two thirds of the participants (66%) did not consider family history as a risk factor for GDM, while 34% reported that diabetes is a familial health condition. Most participants (72.3%) reported that obesity was not a risk factor associated with GDM, with only 27.7% reporting obesity as a risk factor. Three quarters of the participants (75.4%) reported that previous history of GDM was not a risk factor for GDM, compared to a quarter of participants (24.6%) who agreed that GDM could reoccur in subsequent pregnancies. When participants were asked if rapid weight gain (RWG) during pregnancy to be a risk factor associated with GDM, 78.2% of the participants disagreed, while 21.8% agreed. Our study finding also found that majority of participants (69.2%) had never heard about blood tests after a glucose load to test for GDM, while 30.8% were aware of this diagnostic method. When participants were asked if obesity before pregnancy was a risk factor associated with GDM, the majority (72.3%) disagreed, while only 27.7% agreed that it was.
Our other study finding indicated that 82% of the participants believed that it was necessary to test for GDM during pregnancy, while 18% said that it was not. This study also found that most participants 62.7% of participants were aware that diet modifications, exercise, and insulin could treat GDM, compared to 37%who were unaware. Most participants (85%) believed that GDM does not resolve after pregnancy, while 15% believed that it does. 60% of participants believed that not treating GDM poses a risk to the baby, while 40% disagreed. 73% of participants believed that mothers who had GDM in pregnancy were not at risk of developing Type 2 DM in future, while 27% believed that GDM could lead to Type 2 DM.