WHO Team Infection Prevention and Control (IPC). Global report on infection prevention and control. WHO https://www.who.int/publications/i/item/9789240051164 (2022).
Warren, J. L., Chitwood, M. H., Sobkowiak, B., Colijn, C. & Cohen, T. Spatial modeling of Mycobacterium tuberculosis transmission with dyadic genetic relatedness data. Biometrics 79, 3650–3663 (2023).
Martin, J. S. H. et al. Patient and strain characteristics associated with Clostridium difficile transmission and adverse outcomes. Clin. Infect. Dis. 67, 1379–1387 (2018).
Han, J. H. et al. Whole-genome sequencing to identify drivers of carbapenem-resistant Klebsiella pneumoniae transmission within and between regional long-term acute-care hospitals. Antimicrob. Agents Chemother. 63, e01622-19 (2019).
Fishbein, S. R. S. et al. Randomized controlled trial of oral vancomycin treatment in Clostridioides difficile-colonized patients. mSphere 6, e00936-20 (2021).
Wirth, T. et al. Niche specialization and spread of Staphylococcus capitis involved in neonatal sepsis. Nat. Microbiol. 5, 735–745 (2020).
DelaFuente, J. et al. Within-patient evolution of plasmid-mediated antimicrobial resistance. Nat. Ecol. Evol. 6, 1980–1991 (2022).
Magill, S. S. et al. Changes in prevalence of health care-associated infections in U.S. hospitals. N. Engl. J. Med. 379, 1732–1744 (2018).
Allegranzi, B. et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377, 228–241 (2011).
WHO Team Infection Prevention and Control (IPC), Integrated Health Services (IHI). Global report on the epidemiology and burden of sepsis: current evidence, identifying gaps and future directions. https://www.who.int/publications/i/item/9789240010789 (WHO, 2020).
Markwart, R. et al. Epidemiology and burden of sepsis acquired in hospitals and intensive care units: a systematic review and meta-analysis. Intensive Care Med. 46, 1536–1551 (2020).
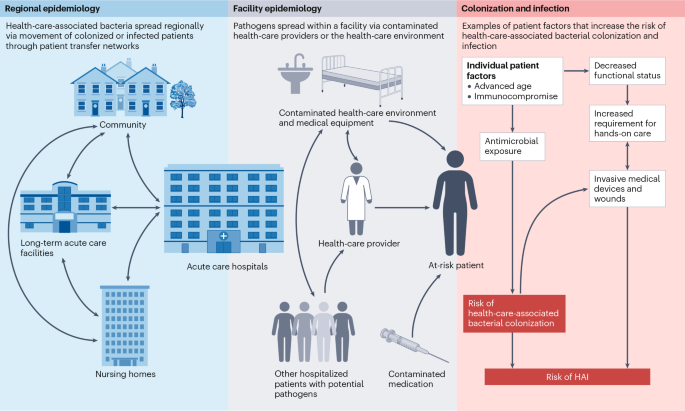
Siegel, J. D., Rhinehart, E., Jackson, M., Chiarello, L. & Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am. J. Infect. Control 35, S65–S164 (2007).
Strassle, P. D. et al. Risk factors for healthcare-associated infections in adult burn patients. Infect. Control Hosp. Epidemiol. 38, 1441–1448 (2017).
Escandon-Vargas, K. et al. Healthcare-associated infections in burn patients: timeline and risk factors. Burns 46, 1775–1786 (2020).
Santomasso, B. D. et al. Management of immune-related adverse events in patients treated with chimeric antigen receptor T-cell therapy: ASCO Guideline. J. Clin. Oncol. 39, 3978–3992 (2021).
Baden, L. R. et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J. Natl Compr. Canc. Netw. 14, 882–913 (2016).
Taplitz, R. A. et al. Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J. Clin. Oncol. 36, 3043–3054 (2018).
Sajiki, D. et al. Risk factors of bloodstream infection after allogeneic hematopoietic cell transplantation in children/adolescent and young adults. PLoS ONE 19, e0308395 (2024).
Dettenkofer, M. et al. Surveillance of nosocomial sepsis and pneumonia in patients with a bone marrow or peripheral blood stem cell transplant: a multicenter project. Clin. Infect. Dis. 40, 926–931 (2005).
van Delden, C. et al. Burden and timeline of infectious diseases in the first year after solid organ transplantation in the Swiss Transplant Cohort Study. Clin. Infect. Dis. 71, e159–e169 (2020).
Abdo-Cuza, A. A. et al. Health care-associated infection in solid organ transplant recipients. Transpl. Proc. 52, 509–511 (2020).
D’Agata, E. M., Mount, D. B., Thayer, V. & Schaffner, W. Hospital-acquired infections among chronic hemodialysis patients. Am. J. Kidney Dis. 35, 1083–1088 (2000).
Abbasi, S. H., Aftab, R. A. & Chua, S. S. Risk factors associated with nosocomial infections among end stage renal disease patients undergoing hemodialysis: a systematic review. PLoS ONE 15, e0234376 (2020).
Teja, B. et al. Complication rates of central venous catheters: a systematic review and meta-analysis. JAMA Intern. Med. 184, 474–482 (2024).
Clack, L., Passerini, S., Wolfensberger, A., Sax, H. & Manser, T. Frequency and nature of infectious risk moments during acute care based on the inform structured classification taxonomy. Infect. Control Hosp. Epidemiol. 39, 272–279 (2018).
Wolfensberger, A. et al. Transfer of pathogens to and from patients, healthcare providers, and medical devices during care activity — a systematic review and meta-analysis. Infect. Control Hosp. Epidemiol. 39, 1093–1107 (2018).
Won, S. Y. et al. Emergence and rapid regional spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin. Infect. Dis. 53, 532–540 (2011).
Wang, J. et al. Application of combined genomic and transfer analyses to identify factors mediating regional spread of antibiotic-resistant bacterial lineages. Clin. Infect. Dis. 71, e642–e649 (2020).
van Dulm, E. et al. High prevalence of multidrug resistant Enterobacteriaceae among residents of long term care facilities in Amsterdam, the Netherlands. PLoS ONE 14, e0222200 (2019).
CDC. HAI and Antimicrobial Use Prevalence Surveys. https://www.cdc.gov/healthcare-associated-infections/php/haic-eip/antibiotic-use.html?CDC_AAref_Val=https://www.cdc.gov/hai/eip/antibiotic-use.html (2024).
Suetens, C. et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eur. Surveill. 23, 1800516 (2018).
Eriksen, H. M. et al. Healthcare-associated infection among residents of long-term care facilities: a cohort and nested case–control study. J. Hosp. Infect. 65, 334–340 (2007).
Tesini, B. L. & Dumyati, G. Health care-associated infections in older adults: epidemiology and prevention. Infect. Dis. Clin. North Am. 37, 65–86 (2023).
High, K. P. et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the infectious Diseases Society of America. J. Am. Geriatr. Soc. 57, 375–394 (2009).
Mody, L., Maheshwari, S., Galecki, A., Kauffman, C. A. & Bradley, S. F. Indwelling device use and antibiotic resistance in nursing homes: identifying a high-risk group. J. Am. Geriatr. Soc. 55, 1921–1926 (2007).
Nicolle, L. E., Bentley, D. W., Garibaldi, R., Neuhaus, E. G. & Smith, P. W. Antimicrobial use in long-term-care facilities. SHEA Long-Term-Care Committee. Infect. Control Hosp. Epidemiol. 21, 537–545 (2000).
Thompson, N. D. et al. Antimicrobial use in a cohort of US nursing homes, 2017. JAMA 325, 1286–1295 (2021).
Ricchizzi, E. et al. Antimicrobial use in European long-term care facilities: results from the third point prevalence survey of healthcare-associated infections and antimicrobial use, 2016 to 2017. Eur. Surveill. 23, 1800394 (2018).
Versporten, A. et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob. Health 6, e619–e629 (2018).
Magill, S. S. et al. Assessment of the appropriateness of antimicrobial use in US hospitals. JAMA Netw. Open 4, e212007 (2021).
Goodman, K. E. et al. Significant regional differences in antibiotic use across 576 US hospitals and 11 701 326 adult admissions, 2016–2017. Clin. Infect. Dis. 73, 213–222 (2021).
Alshubaily, A. M., Alosaimi, A. S., Alhothli, B. I., Althawadi, S. I. & Alghamdi, S. M. Risk of invasive MDRO infection in MDRO-colonized patients. Infect. Control Hosp. Epidemiol. https://doi.org/10.1017/ice.2024.156 (2024).
Simkins, J. et al. Clinical outcomes of intestinal transplant recipients colonized with multidrug-resistant organisms: a retrospective study. Transpl. Int. 30, 924–931 (2017).
Shenoy, E. S., Paras, M. L., Noubary, F., Walensky, R. P. & Hooper, D. C. Natural history of colonization with methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE): a systematic review. BMC Infect. Dis. 14, 177 (2014).
Denkel, L. A. et al. Infections caused by extended-spectrum beta-lactamase-producing Enterobacterales after rectal colonization with ESBL-producing Escherichia coli or Klebsiella pneumoniae. Clin. Microbiol. Infect. 26, 1046–1051 (2020).
Tischendorf, J., de Avila, R. A. & Safdar, N. Risk of infection following colonization with carbapenem-resistant Enterobactericeae: a systematic review. Am. J. Infect. Control 44, 539–543 (2016).
Willems, R. P. J. et al. Incidence of infection with multidrug-resistant Gram-negative bacteria and vancomycin-resistant enterococci in carriers: a systematic review and meta-regression analysis. Lancet Infect. Dis. 23, 719–731 (2023).
Martin, R. M. et al. Molecular epidemiology of colonizing and infecting isolates of Klebsiella pneumoniae. mSphere 1, e00261-16 (2016).
Popovich, K. J. et al. MRSA transmission in intensive care units: genomic analysis of patients, their environments, and healthcare workers. Clin. Infect. Dis. 72, 1879–1887 (2021).
El Haddad, L. et al. Emergence and transmission of daptomycin and vancomycin-resistant enterococci between patients and hospital rooms. Clin. Infect. Dis. 73, 2306–2313 (2021).
Hawken, S. E. et al. Cohorting KPC+ Klebsiella pneumoniae (KPC-Kp)-positive patients: a genomic expose of cross-colonization hazards in a long-term acute-care hospital (LTACH). Infect. Control Hosp. Epidemiol. 41, 1162–1168 (2020).
Kong, L. Y. et al. Clostridium difficile: investigating transmission patterns between infected and colonized patients using whole genome sequencing. Clin. Infect. Dis. 68, 204–209 (2019).
Gouliouris, T. et al. Quantifying acquisition and transmission of Enterococcus faecium using genomic surveillance. Nat. Microbiol. 6, 103–111 (2021).
Armstrong, G. L. et al. Pathogen genomics in public health. N. Engl. J. Med. 381, 2569–2580 (2019).
Fitzpatrick, M. A., Ozer, E. A. & Hauser, A. R. Utility of whole-genome sequencing in characterizing Acinetobacter epidemiology and analyzing hospital outbreaks. J. Clin. Microbiol. 54, 593–612 (2016).
Snitkin, E. S. et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci. Transl. Med. 4, 148ra116 (2012).
Nienaber, J. J. et al. Methicillin-susceptible Staphylococcus aureus endocarditis isolates are associated with clonal complex 30 genotype and a distinct repertoire of enterotoxins and adhesins. J. Infect. Dis. 204, 704–713 (2011).
De Maio, N., Wu, C. H. & Wilson, D. J. SCOTTI: efficient reconstruction of transmission within outbreaks with the structured coalescent. PLoS Comput. Biol. 12, e1005130 (2016).
Didelot, X., Kendall, M., Xu, Y., White, P. J. & McCarthy, N. Genomic epidemiology analysis of infectious disease outbreaks using TransPhylo. Curr. Protoc. 1, e60 (2021).
Snitkin, E. S. et al. Integrated genomic and interfacility patient-transfer data reveal the transmission pathways of multidrug-resistant Klebsiella pneumoniae in a regional outbreak. Sci. Transl. Med. 9, eaan0093 (2017). An integrated epidemiological and genomic investigation of the regional emergence and spread of KPC-producing K. pneumoniae identified patterns of intrafacility and interfacility transmission that could be targeted for intervention.
Marimuthu, K. et al. Whole genome sequencing reveals hidden transmission of carbapenemase-producing Enterobacterales. Nat. Commun. 13, 3052 (2022). Examination of clonal carbapenemase-producing Enterobacterales (CPE) and plasmid-mediated transmission dynamics from a nation-wide surveillance programme in Singapore over a 5-year period found that plasmid-mediated transmission accounted for 50% of CPE dissemination.
Spencer, M. D. et al. Whole genome sequencing detects inter-facility transmission of carbapenem-resistant Klebsiella pneumoniae. J. Infect. 78, 187–199 (2019).
Lane, C. R. et al. Search and contain: impact of an integrated genomic and epidemiological surveillance and response program for control of carbapenemase-producing Enterobacterales. Clin. Infect. Dis. 73, e3912–e3920 (2021).
Jochim-Vukosavic, A. et al. Epidemiology and infection control of vancomycin-resistant enterococci at a German university hospital: a three-year retrospective cohort study. PLoS ONE 19, e0297866 (2024).
Ziakas, P. D., Anagnostou, T. & Mylonakis, E. The prevalence and significance of methicillin-resistant Staphylococcus aureus colonization at admission in the general ICU setting: a meta-analysis of published studies. Crit. Care Med. 42, 433–444 (2014).
Lee, B. Y. et al. Tracking the spread of carbapenem-resistant Enterobacteriaceae (CRE) through clinical cultures alone underestimates the spread of CRE even more than anticipated. Infect. Control Hosp. Epidemiol. 40, 731–734 (2019).
Hawken, S. E. et al. Threshold-free genomic cluster detection to track transmission pathways in health-care settings: a genomic epidemiology analysis. Lancet Microbe 3, e652–e662 (2022). Integration of epidemiological metadata into genomic analyses can overcome limitations of cluster detection based on SNV thresholds and improve the ability to track pathways of pathogen transmission in health-care settings.
Sundermann, A. J. et al. Genomic sequencing surveillance of patients colonized with vancomycin-resistant enterococci improves detection of healthcare-associated transmission. BMC Glob. Public Health 3, 69 (2025).
Keegan, L. T. et al. Environmental and health care personnel sampling and unobserved Clostridium difficile transmission in ICU. JAMA Netw. Open 8, e252787 (2025).
Sansom, S. E. et al. Comparison of daily versus admission and discharge surveillance cultures for multidrug-resistant organism detection in an intensive care unit. J. Infect. Dis. 230, 807–815 (2024).
D’Agata, E. M., Gautam, S., Green, W. K. & Tang, Y. W. High rate of false-negative results of the rectal swab culture method in detection of gastrointestinal colonization with vancomycin-resistant enterococci. Clin. Infect. Dis. 34, 167–172 (2002).
Snyder, G. M. & D’Agata, E. M. Diagnostic accuracy of surveillance cultures to detect gastrointestinal colonization with multidrug-resistant Gram-negative bacteria. Am. J. Infect. Control 40, 474–476 (2012).
Miles-Jay, A. et al. Longitudinal genomic surveillance of carriage and transmission of Clostridioides difficile in an intensive care unit. Nat. Med. 29, 2526–2534 (2023).
Sansom, S. E. et al. Rapid environmental contamination with Candida auris and multidrug-resistant bacterial pathogens near colonized patients. Clin. Infect. Dis. 78, 1276–1284 (2024).
Verhougstraete, M. et al. Impact of terminal cleaning in rooms previously occupied by patients with healthcare-associated infections. PLoS ONE 19, e0305083 (2024).
Vernon, M. O. et al. Chlorhexidine gluconate to cleanse patients in a medical intensive care unit: the effectiveness of source control to reduce the bioburden of vancomycin-resistant enterococci. Arch. Intern. Med. 166, 306–312 (2006).
Stimson, J. et al. Beyond the SNP threshold: identifying outbreak clusters using inferred transmissions. Mol. Biol. Evol. 36, 587–603 (2019).
Eyre, D. W. et al. Diverse sources of C. difficile infection identified on whole-genome sequencing. N. Engl. J. Med. 369, 1195–1205 (2013). The study found that most Clostridioides difficile infections in a large UK region were genetically distinct, indicating that symptomatic patients were responsible for only a minority of transmission events and that diverse, often unidentified sources contribute to the overall burden of infection.
Forde, B. M. et al. Clinical implementation of routine whole-genome sequencing for hospital infection control of multi-drug resistant pathogens. Clin. Infect. Dis. 76, e1277–e1284 (2023).
Coll, F. et al. Definition of a genetic relatedness cutoff to exclude recent transmission of methicillin-resistant Staphylococcus aureus: a genomic epidemiology analysis. Lancet Microbe 1, e328–e335 (2020). Using a retrospective genomic and epidemiological analysis of MRSA data from two prospective observational cohort studies in the UK, the authors applied multiple approaches to calculate within-host diversity of MRSA to establish SNV cut-offs above which MRSA transmission was unlikely.
Gorrie, C. L. et al. Key parameters for genomics-based real-time detection and tracking of multidrug-resistant bacteria: a systematic analysis. Lancet Microbe 2, e575–e583 (2021).
Paterson, G. K. et al. Capturing the cloud of diversity reveals complexity and heterogeneity of MRSA carriage, infection and transmission. Nat. Commun. 6, 6560 (2015).
Hall, M. D. et al. Improved characterisation of MRSA transmission using within-host bacterial sequence diversity. eLife 8, e46402 (2019).
David, S. et al. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat. Microbiol. 4, 1919–1929 (2019). The authors describe the genomic epidemiology of carbapenem-resistant K. pneumoniae in a large European cohort and propose a value for the number of SNVs that optimized discrimination of hospital clusters.
Miles-Jay, A. et al. A multisite genomic epidemiology study of Clostridioides difficile infections in the USA supports differential roles of healthcare versus community spread for two common strains. Microb. Genom. 7, 000590 (2021).
Bush, S. J. et al. Genomic diversity affects the accuracy of bacterial single-nucleotide polymorphism-calling pipelines. Gigascience 9, giaa007 (2020).
Harris, S. R. et al. Whole-genome sequencing for analysis of an outbreak of meticillin-resistant Staphylococcus aureus: a descriptive study. Lancet Infect. Dis. 13, 130–136 (2013). An outbreak investigation integrated epidemiological and genomic data to delineate complex transmission pathways during a year-long MRSA outbreak and identified targets for interventions that ended the outbreak.
Okomo, U. et al. Investigation of sequential outbreaks of Burkholderia cepacia and multidrug-resistant extended spectrum beta-lactamase producing Klebsiella species in a West African tertiary hospital neonatal unit: a retrospective genomic analysis. Lancet Microbe 1, e119–e129 (2020).
Acosta, F. et al. In-depth study of a nosocomial outbreak caused by extensively drug-resistant Pseudomonas aeruginosa using whole genome sequencing coupled with a polymerase chain reaction targeting strain-specific single nucleotide polymorphisms. Am. J. Epidemiol. 189, 841–849 (2020).
Permana, B. et al. Using genomics to investigate an outbreak of vancomycin-resistant Enterococcus faecium ST78 at a large tertiary Hospital in Queensland. Microbiol. Spectr. 11, e0420422 (2023).
Suleyman, G. et al. Use of whole genomic sequencing to detect New Delhi metallo-B-lactamase (NDM)-producing Escherichia coli outbreak associated with endoscopic procedures. Infect. Control Hosp. Epidemiol. 45, 965–972 (2024).
Sundermann, A. J. et al. Outbreak of Pseudomonas aeruginosa infections from a contaminated gastroscope detected by whole genome sequencing surveillance. Clin. Infect. Dis. 73, e638–e642 (2021).
van Ingen, J. et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: a molecular epidemiological study. Lancet Infect. Dis. 17, 1033–1041 (2017).
Johnson, R. C. et al. Investigation of a cluster of Sphingomonas koreensis infections. N. Engl. J. Med. 379, 2529–2539 (2018).
Mellmann, A. et al. Real-time genome sequencing of resistant bacteria provides precision infection control in an institutional setting. J. Clin. Microbiol. 54, 2874–2881 (2016).
Sherry, N. L. et al. Multi-site implementation of whole genome sequencing for hospital infection control: a prospective genomic epidemiological analysis. Lancet Reg. Health West Pac. 23, 100446 (2022).
Ward, D. V. et al. Integration of genomic and clinical data augments surveillance of healthcare-acquired infections. Infect. Control Hosp. Epidemiol. 40, 649–655 (2019).
Neumann, B. et al. Comprehensive integrated NGS-based surveillance and contact-network modeling unravels transmission dynamics of vancomycin-resistant enterococci in a high-risk population within a tertiary care hospital. PLoS ONE 15, e0235160 (2020).
Wu, C. T. et al. Rapid whole genome characterization of antimicrobial-resistant pathogens using long-read sequencing to identify potential healthcare transmission. Infect. Control Hosp. Epidemiol. 46, 1–7 (2024).
Sundermann, A. J. et al. Outbreak of vancomycin-resistant Enterococcus faecium in interventional radiology: detection through whole-genome sequencing-based surveillance. Clin. Infect. Dis. 70, 2336–2343 (2020). Application of prospective genomic surveillance across a hospital system identified an occult outbreak of vancomycin-resistant E. faecium that was traced to the interventional radiology department using a case–control study.
White, R. T. et al. The rapid detection of a neonatal unit outbreak of a wild-type Klebsiella variicola using decentralized Oxford Nanopore sequencing. Antimicrob. Resist. Infect. Control 14, 6 (2025).
Dymond, A. et al. Genomic surveillance of methicillin-resistant Staphylococcus aureus: a mathematical early modeling study of cost-effectiveness. Clin. Infect. Dis. 70, 1613–1619 (2020).
Price, V. et al. A systematic review of economic evaluations of whole-genome sequencing for the surveillance of bacterial pathogens. Microb. Genom. 9, mgen000947 (2023).
Fox, J. M., Saunders, N. J. & Jerwood, S. H. Economic and health impact modelling of a whole genome sequencing-led intervention strategy for bacterial healthcare-associated infections for England and for the USA. Microb. Genom. 9, mgen001087 (2023).
Berbel Caban, A. et al. PathoSPOT genomic epidemiology reveals under-the-radar nosocomial outbreaks. Genome Med. 12, 96 (2020).
Kumar, P. et al. Method for economic evaluation of bacterial whole genome sequencing surveillance compared to standard of care in detecting hospital outbreaks. Clin. Infect. Dis. 73, e9–e18 (2021).
Gordon, L. G. et al. Budget impact analysis of routinely using whole-genomic sequencing of six multidrug-resistant bacterial pathogens in Queensland, Australia. BMJ Open 11, e041968 (2021).
Aanensen, D. M. et al. Whole-genome sequencing for routine pathogen surveillance in public health: a population snapshot of invasive Staphylococcus aureus in Europe. mBio 7, e00444-16 (2016).
Young, B. C. et al. Antimicrobial resistance determinants are associated with Staphylococcus aureus bacteraemia and adaptation to the healthcare environment: a bacterial genome-wide association study. Microb. Genom. 7, 000700 (2021).
Coll, F. et al. Longitudinal genomic surveillance of MRSA in the UK reveals transmission patterns in hospitals and the community. Sci. Transl. Med. 9, eaak9745 (2017). Genomic surveillance of MRSA in the east of England identified putative outbreaks involving hundreds of patients and including hospital outbreaks, outbreaks that spanned the hospital and community, and community outbreaks, including in households.
Sundermann, A. J. et al. Pathogen genomics in healthcare: overcoming barriers to proactive surveillance. Antimicrob. Agents Chemother. 69, e0147924 (2025).
Thiede, S. N. et al. Genomic epidemiology suggests community origins of healthcare-associated USA300 methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 226, 157–166 (2022).
Huang, S. S. et al. Decolonization to reduce postdischarge infection risk among MRSA carriers. N. Engl. J. Med. 380, 638–650 (2019).
McDonald, L. C. et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N. Engl. J. Med. 353, 2433–2441 (2005).
Loo, V. G. et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N. Engl. J. Med. 353, 2442–2449 (2005).
Bauer, K. A. et al. Impact of the NAP-1 strain on disease severity, mortality, and recurrence of healthcare-associated Clostridium difficile infection. Anaerobe 48, 1–6 (2017).
Dong, Q. et al. Virulence and genomic diversity among clinical isolates of ST1 (BI/NAP1/027) Clostridioides difficile. Cell Rep. 42, 112861 (2023).
Newcomer, E. P. et al. Genomic surveillance of Clostridioides difficile transmission and virulence in a healthcare setting. mBio 15, e0330023 (2024).
Saund, K., Pirani, A., Lacy, D. B., Hanna, P. C. & Snitkin, E. Strain variation in Clostridioides difficile cytotoxicity associated with genomic variation at both pathogenic and nonpathogenic loci. mSphere 7, e0017422 (2022).
Eyre, D. W. et al. Two distinct patterns of Clostridium difficile diversity across Europe indicating contrasting routes of spread. Clin. Infect. Dis. 67, 1035–1044 (2018). Genomic sequencing of C. difficile isolates across Europe identified two distinct patterns of transmission: one suggesting predominantly health-care-associated acquisition and the second Europe-wide dissemination via an undetermined route or routes.
Zacharioudakis, I. M., Zervou, F. N., Pliakos, E. E., Ziakas, P. D. & Mylonakis, E. Colonization with toxinogenic C. difficile upon hospital admission, and risk of infection: a systematic review and meta-analysis. Am. J. Gastroenterol. 110, 381–390 (2015).
O’Grady, K. et al. Defining the phylogenetics and resistome of the major Clostridioides difficile ribotypes circulating in Australia. Microb. Genom. 10, 001232 (2024).
Rupnik, M. et al. Distribution of Clostridioides difficile ribotypes and sequence types across humans, animals and food in 13 European countries. Emerg. Microbes Infect. 13, 2427804 (2024).
Knight, D. R. et al. Genomic epidemiology and transmission dynamics of recurrent Clostridioides difficile infection in Western Australia. Eur. J. Clin. Microbiol. Infect. Dis. 42, 607–619 (2023).
Barker, A. K., Krasity, B., Musuuza, J. & Safdar, N. Screening for asymptomatic Clostridium difficile among bone marrow transplant patients: a mixed-methods study of intervention effectiveness and feasibility. Infect. Control Hosp. Epidemiol. 39, 177–185 (2018).
Longtin, Y., Gilca, R. & Loo, V. G. Effect of detecting and isolating asymptomatic Clostridium difficile carriers-reply. JAMA Intern. Med. 176, 1573 (2016).
Cho, J. et al. Clostridioides difficile whole-genome sequencing differentiates relapse with the same strain from reinfection with a new strain. Clin. Infect. Dis. 72, 806–813 (2021).
Sader, H. S. et al. Frequency of occurrence and antimicrobial susceptibility of bacteria isolated from respiratory samples of patients hospitalized with pneumonia in Western Europe, Eastern Europe and the USA: results from the SENTRY Antimicrobial Surveillance Program (2016–19). JAC Antimicrob. Resist. 3, dlab117 (2021).
Navon-Venezia, S., Kondratyeva, K. & Carattoli, A. Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol. Rev. 41, 252–275 (2017).
Munoz-Price, L. S. et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect. Dis. 13, 785–796 (2013).
David, S. et al. Integrated chromosomal and plasmid sequence analyses reveal diverse modes of carbapenemase gene spread among Klebsiella pneumoniae. Proc. Natl Acad. Sci. USA 117, 25043–25054 (2020).
Lapp, Z. et al. Distinct origins and transmission pathways of bla(KPC) Enterobacterales across three U.S. states. J. Clin. Microbiol. 61, e0025923 (2023).
Luterbach, C. L. et al. A network analysis of carbapenem-resistant Klebsiella pneumoniae among healthcare facilities. Sci. Rep. 15, 27565 (2025).
Popovich, K. J. & Snitkin, E. S. Whole genome sequencing — implications for infection prevention and outbreak investigations. Curr. Infect. Dis. Rep. 19, 15 (2017).
Lam, M. M. C. et al. Population genomics of hypervirulent Klebsiella pneumoniae clonal-group 23 reveals early emergence and rapid global dissemination. Nat. Commun. 9, 2703 (2018).
Russo, T. A. & Marr, C. M. Hypervirulent Klebsiella pneumoniae. Clin. Microbiol. Rev. 32, e00001-19 (2019).
Dong, N., Lin, D., Zhang, R., Chan, E. W. & Chen, S. Carriage of blaKPC-2 by a virulence plasmid in hypervirulent Klebsiella pneumoniae. J. Antimicrob. Chemother. 73, 3317–3321 (2018).
Alm, E. K. A., Linkevicius, M., Monnet D. & Plachouras D. Emergence of hypervirulent Klebsiella pneumoniae ST23 carrying carbapenemase genes in EU/EEA countries, first update, Stockholm, Sweden (2024).
Gu, D. et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect. Dis. 18, 37–46 (2018).
Brennan, C. et al. A geographic cluster of healthcare-associated carbapenemase-producing hypervirulent Klebsiella pneumoniae sequence type 23. Eur. J. Clin. Microbiol. Infect. Dis. https://doi.org/10.1007/s10096-022-04535-z (2022).
Higgs, C. et al. Optimising genomic approaches for identifying vancomycin-resistant Enterococcus faecium transmission in healthcare settings. Nat. Commun. 13, 509 (2022).
Campbell, F. et al. outbreaker2: a modular platform for outbreak reconstruction. BMC Bioinformatics 19, 363 (2018).
Valles-Colomer, M. et al. The person-to-person transmission landscape of the gut and oral microbiomes. Nature 614, 125–135 (2023). Integrative analysis of multiple large international metagenomic data sets with known family relationships was used to describe sharing of gut and oral microbial strains among cohabiting individuals.
Olm, M. R. et al. inStrain profiles population microdiversity from metagenomic data and sensitively detects shared microbial strains. Nat. Biotechnol. 39, 727–736 (2021).
Charalampous, T. et al. Routine metagenomics service for ICU patients with respiratory infection. Am. J. Respir. Crit. Care Med. 209, 164–174 (2024).
Fourgeaud, J. et al. Performance of clinical metagenomics in France: a prospective observational study. Lancet Microbe 5, e52–e61 (2024).
Chiu, C. Y. & Miller, S. A. Clinical metagenomics. Nat. Rev. Genet. 20, 341–355 (2019). Comprehensive review of metagenomic next-generation sequencing in the clinical laboratory.
CDC. Innovative Studies Investigate Spread of Antimicrobial Resistance in Communities and Hospitals (ARCH) https://www.cdc.gov/international-infection-control/php/stories/ar-spread-studies.html (CDC, 2024).
NIHR Global Health Research Unit. Genomic Surveillance of Antimicrobial Resistance https://ghru.pathogensurveillance.net/#home (NIHR, 2025).
Ludden, C. et al. Defining nosocomial transmission of Escherichia coli and antimicrobial resistance genes: a genomic surveillance study. Lancet Microbe 2, e472–e480 (2021). This study provides evidence of extensive diversity within the population of E. coli colonizing and infecting adult patients on two haematology wards, with carriage of multiple strains of E. coli being common, challenging the practice of single-colony genomic epidemiology investigations.
Ammerlaan, H. S., Troelstra, A., Kruitwagen, C. L., Kluytmans, J. A. & Bonten, M. J. Quantifying changes in incidences of nosocomial bacteraemia caused by antibiotic-susceptible and antibiotic-resistant pathogens. J. Antimicrob. Chemother. 63, 1064–1070 (2009).
Nurjadi, D. et al. Surveillance for colonization, transmission, and infection with methicillin-susceptible Staphylococcus aureus in a neonatal intensive care unit. JAMA Netw. Open 4, e2124938 (2021).
Mathers, A. J. et al. Molecular dissection of an outbreak of carbapenem-resistant Enterobacteriaceae reveals intergenus KPC carbapenemase transmission through a promiscuous plasmid. mBio 2, e00204-11 (2011).
Shankar, C. et al. Tracking bla (KPC) plasmid dissemination within and between Enterobacterales across Michigan over a decade. Preprint at bioRxiv https://doi.org/10.1101/2025.08.18.670900 (2025).
Gu, Y. et al. Dissemination of bla(NDM)-harboring plasmids in carbapenem-resistant and hypervirulent Klebsiella pneumoniae. Microbiol. Spectr. 13, e0196824 (2025).
Lapp, Z. et al. Regional spread of blaNDM-1-containing Klebsiella pneumoniae ST147 in post-acute care facilities. Clin. Infect. Dis. 73, 1431–1439 (2021).
Balasubramanian, R., Van Boeckel, T. P., Carmeli, Y., Cosgrove, S. & Laxminarayan, R. Global incidence in hospital-associated infections resistant to antibiotics: an analysis of point prevalence surveys from 99 countries. PLoS Med. 20, e1004178 (2023).
CDC. HAI Pathogens and Antimicrobial Resistance Report, 2018–2021 (Centers for Disease Control and Prevention, 2023).
Goh, L. P. W., Marbawi, H., Goh, S. M., Bin Abdul Asis, A. K. & Gansau, J. A. The prevalence of hospital-acquired infections in Southeast Asia (1990–2022). J. Infect. Dev. Ctries 17, 139–146 (2023).
Cassini, A. et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect. Dis. 19, 56–66 (2019).
CDC. Antibiotic Resistance Threats in the United States, 2019 (Centers for Disease Control and Prevention, 2019).
CDC. COVID-19: U.S. Impact on Antimicrobial Resistance, Special Report 2022, Atlanta, GA (2022).
CDC. Antimicrobial Resistance Threats in the United States, 2021–2022 https://www.cdc.gov/antimicrobial-resistance/data-research/threats/update-2022.html (CDC, 2024).
Wolford, H. et al. Antimicrobial-resistant infections in hospitalized patients. JAMA Netw. Open 8, e2462059 (2025).
Eure, T. R., Stone, N. D., Mungai, E. A., Bell, J. M. & Thompson, N. D. Antibiotic-resistant pathogens associated with urinary tract infections in nursing homes: summary of data reported to the National Healthcare Safety Network Long-term Care Facility Component, 2013-2017. Infect. Control Hosp. Epidemiol. 42, 31–36 (2021).
McKinnell, J. A. et al. High prevalence of multidrug-resistant organism colonization in 28 nursing homes: an ‘iceberg effect’. J. Am. Med. Dir. Assoc. 21, 1937–1943.e2 (2020).
Segerman, B. The most frequently used sequencing technologies and assembly methods in different time segments of the bacterial surveillance and RefSeq genome databases. Front. Cell Infect. Microbiol. 10, 527102 (2020).
World Health Organization. GLASS Whole-Genome Sequencing for Surveillance of Antimicrobial Resistance (World Health Organization, 2020).
Meslier, V. et al. Benchmarking second and third-generation sequencing platforms for microbial metagenomics. Sci. Data 9, 694 (2022).
Macesic, N. et al. Genomic dissection of endemic carbapenem resistance reveals metallo-beta-lactamase dissemination through clonal, plasmid and integron transfer. Nat. Commun. 14, 4764 (2023).
Garza-Ramos, U. et al. Whole genome analysis of Gram-negative bacteria using the EPISEQ CS application and other bioinformatic platforms. J. Glob. Antimicrob. Resist. 33, 61–71 (2023).
Durand, G. et al. Routine whole-genome sequencing for outbreak investigations of Staphylococcus aureus in a national reference center. Front. Microbiol. 9, 511 (2018).
Harris, P. N. A. et al. Rapid nanopore sequencing and predictive susceptibility testing of positive blood cultures from intensive care patients with sepsis. Microbiol. Spectr. 12, e0306523 (2024).
Lang, A. S., Buchan, A. & Burrus, V. Interactions and evolutionary relationships among bacterial mobile genetic elements. Nat. Rev. Microbiol. https://doi.org/10.1038/s41579-025-01157-y (2025).
Bush, K. & Bradford, P. A. Epidemiology of beta-lactamase-producing pathogens. Clin. Microbiol. Rev. 33, e00047-19 (2020).
Frost, L. S., Leplae, R., Summers, A. O. & Toussaint, A. Mobile genetic elements: the agents of open source evolution. Nat. Rev. Microbiol. 3, 722–732 (2005).
Evans, D. R. et al. Systematic detection of horizontal gene transfer across genera among multidrug-resistant bacteria in a single hospital. eLife 9, e53886 (2020).
Orlek, A. et al. Plasmid classification in an era of whole-genome sequencing: application in studies of antibiotic resistance epidemiology. Front. Microbiol. 8, 182 (2017).
Acman, M. et al. Role of mobile genetic elements in the global dissemination of the carbapenem resistance gene bla(NDM). Nat. Commun. 13, 1131 (2022).
Redondo-Salvo, S. et al. Pathways for horizontal gene transfer in bacteria revealed by a global map of their plasmids. Nat. Commun. 11, 3602 (2020).
Hawkey, J. et al. ESBL plasmids in Klebsiella pneumoniae: diversity, transmission and contribution to infection burden in the hospital setting. Genome Med. 14, 97 (2022).
Leon-Sampedro, R. et al. Pervasive transmission of a carbapenem resistance plasmid in the gut microbiota of hospitalized patients. Nat. Microbiol. 6, 606–616 (2021).
Frolova, D. et al. Applying rearrangement distances to enable plasmid epidemiology with pling. Microb. Genom. 10, 001300 (2024).
Knudsen, P. K. et al. Transfer of a bla (CTX-M-1)-carrying plasmid between different Escherichia coli strains within the human gut explored by whole genome sequencing analyses. Sci. Rep. 8, 280 (2018).
Kocer, K. et al. Comparative genomic analysis reveals a high prevalence of inter-species in vivo transfer of carbapenem-resistance plasmids in patients with haematological malignancies. Clin. Microbiol. Infect. 26, 780.e1–780.e8 (2020).
Mustapha, M. M. et al. Genomic diversity of hospital-acquired infections revealed through prospective whole-genome sequencing-based surveillance. mSystems 7, e0138421 (2022).
Xie, O. et al. Overlapping Streptococcus pyogenes and Streptococcus dysgalactiae subspecies equisimilis household transmission and mobile genetic element exchange. Nat. Commun. 15, 3477 (2024).