By stimulating the release of the neurotransmitter acetylcholine, it lowers the heart rate and blood pressure while supporting digestion and the immune function. That’s why, Etienne says, “we really want to try to get that vagus nerve activated, to get your nervous system back in balance.” When it’s not, he says, the effects often show up as “lack of sleep, being really low energy, mental health issues, and gut problems.”
The medical origins of VNS tools
Research into vagus nerve stimulation began in the 1980s, when scientists first tested it as a potential treatment for epilepsy. These devices were implanted in patients’ necks, close to the vagus nerve, and controlled remotely. “The major outcome measure was diminishing seizure frequency by more than 50 percent, so the FDA approved the application of VNS to treat seizures in 1997,” says Timea Hodics, neurologist and stroke researcher at Houston Methodist Hospital. “During those trials, they observed that people’s depression improved as well, so that approval followed in 2005.”
Exclusive Holiday Gift Bundle
Gift a subscription to wonder
The first FDA approval for transcutaneous, or non-implanted, VNS devices came in 2018, for cluster headaches and migraines, followed by approval for post-stroke rehabilitation treatment in 2021.
(Here’s how changing the way you breathe can improve your brain and body.)
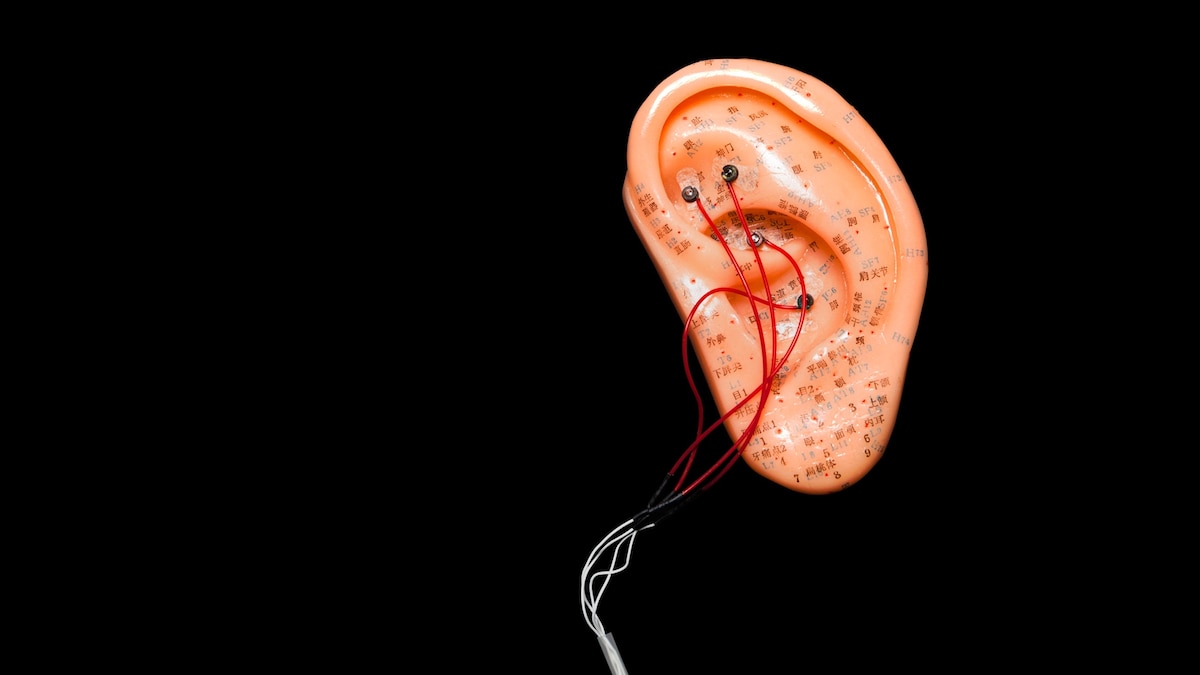
Consumer versions entered the market around five years ago. Using the same bioelectrical principles as implanted versions, these handheld or headphone-like tools are designed for brief daily use—typically from a few minutes to an hour. They deliver mild electrical pulses via auricular (ear) or cervical (neck) contact.
Since they’re “approximating where the nerve is,” Etienne says, the current is reduced because it has to travel through the skin. “Another big difference is that when the [device is] inside the patient’s body, we can actually guarantee they’re going to get a certain amount of stimulation every day.”
Are VNS devices proven to work?
While implanted VNS has been studied extensively, research on newer, non-invasive versions remains limited. A 2023 study found that transcutaneous VNS (tVNS) reduced acute stress in healthy young adults across five physiological outcomes, using a single-blind design to control for the placebo effect. A 2024 study showed it was a “powerful and effective” tool for reducing anxiety among retired teachers, but both these studies had small sample sizes (19 and 60 participants, respectively).
“The question is whether [tVNS] really decreased the anxiety or just decreased the symptoms,” says Hodics, commenting on the latter. “I would have liked to have some degree of additional measures to find out.” In contrast, she points out that another 2024 study, which found significant improvements in sleep quality among 68 people with chronic insomnia, relies on “subjective, self-reported measures” rather than observable data.
Still, researchers are finding intriguing intersections between bioelectrical science and mindfulness. A randomized controlled trial published in August found that tVNS augmented self-compassion training, with the authors suggesting that it could be a useful tool for “enhancing meditation-based psychotherapies.
Do experts recommend VNS devices?
As research continues, experts say vagus nerve stimulation may be most useful as a complement to other stress-management techniques—not a replacement for them.