Mika, J. et al. Symptom-based early-stage differentiation between SARS-CoV-2 versus other respiratory tract infections—Upper Silesia pilot study. Sci. Rep. 11 (1), 13580 (2021).
Zhang, J., Garrett, S. & Sun, J. Gastrointestinal symptoms, pathophysiology, and treatment in COVID-19. Genes Dis. 8 (4), 385–400 (2021).
Basu-Ray, I., Almaddah, N., Adeboye, A. & Soos, M. P. Cardiac Manifestations Of Coronavirus (COVID-19). StatPearls. Treasure Island (FL)2022.
Wang, X., Lei, J., Li, Z. & Yan, L. Potential effects of coronaviruses on the liver: an update. Front. Med. 8. (2021).
Li, Y. C., Bai, W. Z. & Hashikawa, T. The neuroinvasive potential of SARS-CoV2 May play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 92 (6), 552–555 (2020).
Mohseni Afshar, Z. et al. Dermatological manifestations associated with COVID-19: A comprehensive review of the current knowledge. J. Med. Virol. 93 (10), 5756–5767 (2021).
Singh, H., Kaur, H., Singh, K. & Sen, C. K. Cutaneous manifestations of COVID-19: A systematic review. Adv. Wound Care (New Rochelle). 10 (2), 51–80 (2021).
Conforti, C. et al. Cutaneous manifestations in confirmed COVID-19 patients: A systematic review. Biology (Basel) ;9(12). (2020).
Hayderi, L. E., Nikkels-Tassoudji, N. & Nikkels, A. F. Hair loss after varicella Zoster virus infection. Case Rep. Dermatol. 5 (1), 43–47 (2013).
Chu, C-B. & Yang, C-C. Dengue-associated Telogen effluvium: A report of 14 patients. Dermatologica Sinica. 35 (3), 124–126 (2017).
Hussain, N. et al. A systematic review of acute Telogen effluvium, a harrowing post-COVID-19 manifestation. J. Med. Virol. 94 (4), 1391–1401 (2022).
Lv, S. et al. A case of acute Telogen effluvium after SARS-CoV-2 infection. Clin. Cosmet. Investig Dermatol. 14, 385–387 (2021).
Rizzetto, G. et al. Telogen effluvium related to post severe Sars-Cov-2 infection: clinical aspects and our management experience. Dermatol. Ther. 34 (1), e14547 (2021).
Sattur, S. S. & Sattur, I. S. COVID-19 infection: impact on hair. Indian J. Plast. Surg. 54 (4), 521–526 (2021).
Shanshal, M. COVID-19 related anagen effluvium. J. Dermatolog Treat. 33 (2), 1114–1115 (2022).
Seyfi, S., Alijanpour, R., Aryanian, Z., Ezoji, K. & Mahmoudi, M. Prevalence of Telogen effluvium hair loss in COVID-19 patients and its relationship with disease severity. J. Med. Life. 15 (5), 631–634 (2022).
Shendre, M. E. R., Thejaswi, S. R., Mendagudli, C., Nair, V. U. & Rajesh, S. Acute Telogen effluvium: A Post-COVID-19 sequela. Clin. Dermatology Rev. 7 (2), 158–160 (2023).
Awad, N., Obaid, Z. M., Zaky, M. S. & Elsaie, M. L. Hair disorders associated with post-COVID-19 infection in females: a cross-sectional study. Ir. J. Med. Sci. 193 (2), 761–767 (2024).
Iancu, G. M. et al. SARS-CoV-2 Infection-A trigger factor for Telogen effluvium: review of the literature with a Case-Based guidance for clinical evaluation. Life (Basel) ;13(7). (2023).
Ji, S., Zhu, Z., Sun, X. & Fu, X. Functional hair follicle regeneration: an updated review. Signal. Transduct. Target. Therapy. 6 (1), 66 (2021).
Yu, J., Yu, D. W., Checkla, D. M., Freedberg, I. M. & Bertolino, A. P. Human hair keratins. J. Invest. Dermatol. 101 (1 Suppl), 56s–9s (1993).
Lolli, F. et al. Androgenetic alopecia: a review. Endocrine 57 (1), 9–17 (2017).
Rebora, A. Telogen effluvium: a comprehensive review. Clin. Cosmet. Investig Dermatol. 12, 583–590 (2019).
Grover, C. & Khurana, A. Telogen effluvium. Indian J. Dermatol. Venereol. Leprol. 79 (5), 591–603 (2013).
Malkud, S. Telogen effluvium: A review. J. Clin. Diagn. Res. 9 (9), WE01–3 (2015).
Phillips, T. G., Slomiany, W. P. & Allison, R. Hair loss: common causes and treatment. Am. Fam Physician. 96 (6), 371–378 (2017).
Alessandrini, A., Bruni, F., Piraccini, B. M. & Starace, M. Common causes of hair loss – clinical manifestations, trichoscopy and therapy. J. Eur. Acad. Dermatol. Venereol. 35 (3), 629–640 (2021).
Asghar, F., Shamim, N., Farooque, U., Sheikh, H. & Aqeel, R. Telogen effluvium: A review of the literature. Cureus 12 (5), e8320 (2020).
Mieczkowska, K. et al. Telogen effluvium: a sequela of COVID-19. Int. J. Dermatol. 60 (1), 122–124 (2021).
Olds, H. et al. Telogen effluvium associated with COVID-19 infection. Dermatol. Ther. 34 (2), e14761 (2021).
Aksoy, H., Yıldırım, U. M., Ergen, P. & Gürel, M. S. COVID-19 induced Telogen effluvium. Dermatol. Ther. 34 (6), e15175 (2021).
Goren, A. et al. A preliminary observation: male pattern hair loss among hospitalized COVID-19 patients in Spain – A potential clue to the role of androgens in COVID-19 severity. J. Cosmet. Dermatol. 19 (7), 1545–1547 (2020).
Abrantes, T. F. et al. Time of onset and duration of post-COVID-19 acute Telogen effluvium. J. Am. Acad. Dermatol. 85 (4), 975–976 (2021).
Koç Yıldırım, S., Erbağcı, E. & Demirel Öğüt, N. Evaluation of patients with Telogen effluvium during the pandemic: May the monocytes be responsible for post COVID-19 Telogen effluvium? J. Cosmet. Dermatol. 21 (5), 1809–1815 (2022).
Corrêa Giron, C., Laaksonen, A. & Barroso da Silva, F. L. On the interactions of the receptor-binding domain of SARS-CoV-1 and SARS-CoV-2 Spike proteins with monoclonal antibodies and the receptor ACE2. Virus Res. 285, 198021 (2020).
Jackson, C. B., Farzan, M., Chen, B. & Choe, H. Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 23 (1), 3–20 (2022).
Steiner, S. et al. SARS-CoV-2 biology and host interactions. Nat. Rev. Microbiol. 22 (4), 206–225 (2024).
Hoffmann, M. et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181 (2), 271– (2020). – 80.e8.
Mazeto, I. F. S. et al. Ultrastructural evidence for anagen hair follicle infection with SARS-CoV-2 in early-onset COVID-19 effluvium. J. Eur. Acad. Dermatol. Venereol. 36 (11), e865–e7 (2022).
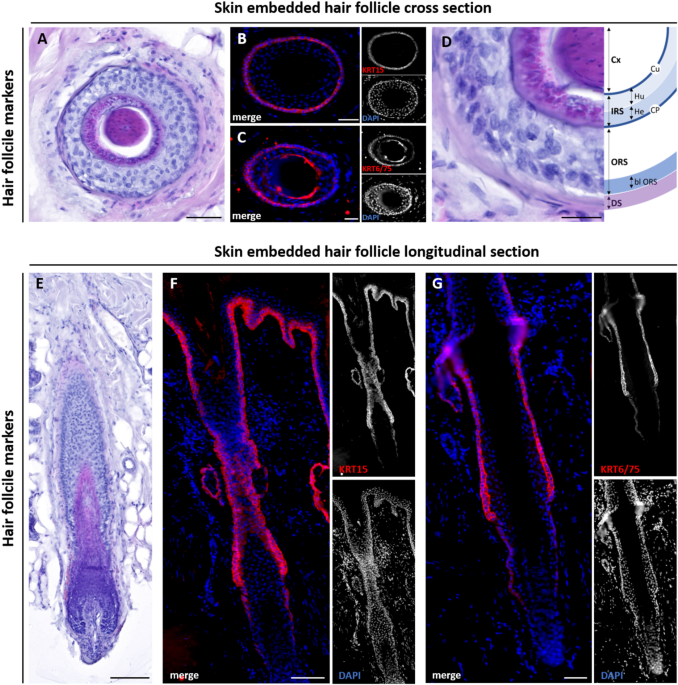
Limat, A. & Hunziker, T. Cultivation of keratinocytes from the outer root sheath of human hair follicles. Methods Mol. Med. 2, 21–31 (1996).
Prost-Squarcioni, C. [Histology of skin and hair follicle]. Med. Sci. (Paris). 22 (2), 131–137 (2006).
Martino, P. A., Heitman, N. & Rendl, M. The dermal sheath: an emerging component of the hair follicle stem cell niche. Exp. Dermatol. 30 (4), 512–521 (2021).
Lyle, S. et al. The C8/144B monoclonal antibody recognizes cytokeratin 15 and defines the location of human hair follicle stem cells. J. Cell. Sci. 111 (Pt 21), 3179–3188 (1998).
Schweizer, J. et al. New consensus nomenclature for mammalian keratins. J. Cell. Biol. 174 (2), 169–174 (2006).
Moll, R., Divo, M. & Langbein, L. The human keratins: biology and pathology. Histochem. Cell. Biol. 129 (6), 705–733 (2008).
Bragulla, H. H. & Homberger, D. G. Structure and functions of keratin proteins in simple, stratified, keratinized and cornified epithelia. J. Anat. 214 (4), 516–559 (2009).
Lenoir, M. C., Bernard, B. A., Pautrat, G., Darmon, M. & Shroot, B. Outer root sheath cells of human hair follicle are able to regenerate a fully differentiated epidermis in vitro. Dev. Biol. 130 (2), 610–620 (1988).
Xue, X. et al. High expression of ACE2 on keratinocytes reveals skin as a potential target for SARS-CoV-2. J. Invest. Dermatol. 141 (1), 206–9e1 (2021).
Klingenstein, M. et al. Evidence of SARS-CoV2 entry protein ACE2 in the human nose and olfactory bulb. Cells Tissues Organs. 209 (4–6), 155–164 (2020).
Wagner, V. P. et al. Histogenesis of keratoacanthoma: histochemical and immunohistochemical study. oral Surgery, oral medicine. Oral Pathol. Oral Radiol. 119 (3), 310–317 (2015).
Kobielak, K., Pasolli, H. A., Alonso, L., Polak, L. & Fuchs, E. Defining BMP functions in the hair follicle by conditional ablation of BMP receptor IA. J. Cell. Biol. 163 (3), 609–623 (2003).
Rogers, M. A., Winter, H., Schweizer, J., Langbein, L. & Praetzel, S. K6irs1, K6irs2, K6irs3, and K6irs4 represent the Inner-Root-Sheath-Specific type II epithelial keratins of the human hair Follicle1. J. Invest. Dermatology. 120 (4), 512–522 (2003).
Sperling, L. C., Hussey, S., Sorrells, T., Wang, J. A. & Darling, T. Cytokeratin 75 expression in central, centrifugal, cicatricial alopecia–new observations in normal and diseased hair follicles. J. Cutan. Pathol. 37 (2), 243–248 (2010).
Clemmensen, O. J., Hainau, B. & Hansted, B. The ultrastructure of the transition zone between specialized cells (Flugelzellen) of huxley’s layer of the inner root sheath and cells of the outer root sheath of the human hair follicle. Am. J. Dermatopathol. 13 (3), 264–270 (1991).
Klingenstein, S., Klingenstein, M., Kleger, A. & Liebau, S. From hair to iPSCs-A guide on how to reprogram keratinocytes and why. Curr. Protoc. Stem Cell. Biol. 55 (1), e121 (2020).
Ho, M. et al. Update of the keratin gene family: evolution, tissue-specific expression patterns, and relevance to clinical disorders. Hum. Genomics. 16 (1), 1 (2022).
Moll, R. [Cytokeratins as markers of differentiation. Expression profiles in epithelia and epithelial tumors]. Veroff Pathol. 142, 1–197 (1993).
Moll, R., Divo, M. & Langbein, L. The human keratins: biology and pathology. Histochem. Cell Biol. 129 (6), 705 (2008).
Hikmet, F. et al. The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol. 16 (7), e9610 (2020).
Li, M-Y., Li, L., Zhang, Y. & Wang, X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect. Dis. Poverty. 9 (1), 45 (2020).
Salamanna, F., Maglio, M., Landini, M. P. & Fini, M. Body localization of ACE-2: on the trail of the keyhole of SARS-CoV-2. Front. Med. (Lausanne). 7, 594495 (2020).
Li, F. et al. Distinct mechanisms for TMPRSS2 expression explain organ-specific Inhibition of SARS-CoV-2 infection by enzalutamide. Nat. Commun. 12 (1), 866 (2021).
Dong, M. et al. ACE2, TMPRSS2 distribution and extrapulmonary organ injury in patients with COVID-19. Biomed. Pharmacother. 131, 110678 (2020).
Nersisyan, S., Shkurnikov, M., Turchinovich, A., Knyazev, E. & Tonevitsky, A. Integrative analysis of MiRNA and mRNA sequencing data reveals potential regulatory mechanisms of ACE2 and TMPRSS2. PLoS One. 15 (7), e0235987 (2020).
Hamming, I. et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in Understanding SARS pathogenesis. J. Pathol. 203 (2), 631–637 (2004).
Koupenova, M. et al. SARS-CoV-2 initiates programmed cell death in platelets. Circ. Res. 129 (6), 631–646 (2021).
Zhang, J. et al. Understanding the role of SARS-CoV-2 ORF3a in viral pathogenesis and COVID-19. Front. Microbiol. 13, 854567 (2022).
Premeaux, T. A. et al. Emerging insights on caspases in COVID-19 Pathogenesis, Sequelae, and directed therapies. Front. Immunol. 13, 842740 (2022).
Hagman, K. et al. Prevalence and clinical relevance of viraemia in viral respiratory tract infections: a systematic review. Lancet Microbe. 6 (2), 100967 (2025).
Stein, S. R. et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature 612 (7941), 758–763 (2022).
Yuan, C. et al. The role of cell death in SARS-CoV-2 infection. Signal. Transduct. Target. Ther. 8 (1), 357 (2023).
Pontelli, M. C. et al. SARS-CoV-2 productively infects primary human immune system cells in vitro and in COVID-19 patients. J. Mol. Cell. Biol. ;14(4). (2022).
Ruetalo, N. et al. Antibody response against SARS-CoV-2 and seasonal coronaviruses in nonhospitalized COVID-19 patients. mSphere 6(1). (2021).